Korean J Radiol.
2015 Oct;16(5):1029-1037. 10.3348/kjr.2015.16.5.1029.
Dynamic Contrast-Enhanced MRI Using a Macromolecular MR Contrast Agent (P792): Evaluation of Antivascular Drug Effect in a Rabbit VX2 Liver Tumor Model
- Affiliations
-
- 1Department of Radiology, Konkuk University School of Medicine, Seoul 05030, Korea.
- 2Department of Radiology and Institute of Radiation Medicine, Seoul National University Hospital, Seoul 03080, Korea. hanjk@snu.ac.kr
- 3Department of Radiology, Sheikh Khalifa Specialty Hospital, Ras Al Khaimah, United Arab Emirates.
- 4Department of Internal Medicine, Seoul National University Hospital, Seoul 03080, Korea.
- 5Department of Radiology, Yonsei University College of Medicine, Seoul 03722, Korea.
- KMID: 2160770
- DOI: http://doi.org/10.3348/kjr.2015.16.5.1029
Abstract
OBJECTIVE
To evaluate the utility of dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) using macromolecular contrast agent (P792) for assessment of vascular disrupting drug effect in rabbit VX2 liver tumor models.
MATERIALS AND METHODS
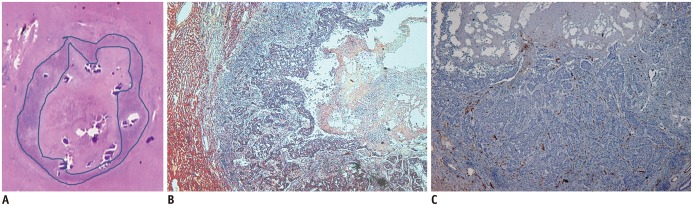
This study was approved by our Institutional Animal Care and Use Committee. DCE-MRI was performed with 3-T scanner in 13 VX2 liver tumor-bearing rabbits, before, 4 hours after, and 24 hours after administration of vascular disrupting agent (VDA), using gadomelitol (P792, n = 7) or low molecular weight contrast agent (gadoterate meglumine [Gd-DOTA], n = 6). P792 was injected at a of dose 0.05 mmol/kg, while that of Gd-DOTA was 0.2 mmol/kg. DCE-MRI parameters including volume transfer coefficient (K(trans)) and initial area under the gadolinium concentration-time curve until 60 seconds (iAUC) of tumors were compared between the 2 groups at each time point. DCE-MRI parameters were correlated with tumor histopathology. Reproducibility in measurement of DCE-MRI parameters and image quality of source MR were compared between groups.
RESULTS
P792 group showed a more prominent decrease in K(trans) and iAUC at 4 hours and 24 hours, as compared to the Gd-DOTA group. Changes in DCE-MRI parameters showed a weak correlation with histologic parameters (necrotic fraction and microvessel density) in both groups. Reproducibility of DCE-MRI parameters and overall image quality was not significantly better in the P792 group, as compared to the Gd-DOTA group.
CONCLUSION
Dynamic contrast-enhanced magnetic resonance imaging using a macromolecular contrast agent shows changes of hepatic perfusion more clearly after administration of the VDA. Gadolinium was required at smaller doses than a low molecular contrast agent.
Keyword
MeSH Terms
-
Animals
Antineoplastic Agents/therapeutic use
Benzophenones/therapeutic use
Disease Models, Animal
Heterocyclic Compounds/administration & dosage/*chemistry
Liver Neoplasms/drug therapy/pathology/*radiography
*Magnetic Resonance Imaging
Male
Organometallic Compounds/administration & dosage/*chemistry
Rabbits
Reproducibility of Results
Valine/analogs & derivatives/therapeutic use
Antineoplastic Agents
Benzophenones
Heterocyclic Compounds
Organometallic Compounds
Valine
Figure
Reference
-
1. Delrue LJ, Casneuf V, Van Damme N, Blanckaert P, Peeters M, Ceelen WP, et al. Assessment of neovascular permeability in a pancreatic tumor model using dynamic contrast-enhanced (DCE) MRI with contrast agents of different molecular weights. MAGMA. 2011; 24:225–232. PMID: 21567161.
Article2. Choyke PL, Dwyer AJ, Knopp MV. Functional tumor imaging with dynamic contrast-enhanced magnetic resonance imaging. J Magn Reson Imaging. 2003; 17:509–520. PMID: 12720260.
Article3. Barrett T, Kobayashi H, Brechbiel M, Choyke PL. Macromolecular MRI contrast agents for imaging tumor angiogenesis. Eur J Radiol. 2006; 60:353–366. PMID: 16930905.
Article4. Jacquier A, Bucknor M, Do L, Robert P, Corot C, Higgins CB, et al. P846, a new gadolinium based low diffusion magnetic resonance contrast agent, in characterizing occlusive infarcts, reperfused ischemic myocardium and reperfused infarcts in rats. MAGMA. 2008; 21:207–218. PMID: 18446394.
Article5. Lemasson B, Serduc R, Maisin C, Bouchet A, Coquery N, Robert P, et al. Monitoring blood-brain barrier status in a rat model of glioma receiving therapy: dual injection of low-molecular-weight and macromolecular MR contrast media. Radiology. 2010; 257:342–352. PMID: 20829544.
Article6. Daldrup H, Shames DM, Wendland M, Okuhata Y, Link TM, Rosenau W, et al. Correlation of dynamic contrast-enhanced MR imaging with histologic tumor grade: comparison of macromolecular and small-molecular contrast media. AJR Am J Roentgenol. 1998; 171:941–949. PMID: 9762973.
Article7. Port M, Corot C, Raynal I, Idee JM, Dencausse A, Lancelot E, et al. Physicochemical and biological evaluation of P792, a rapid-clearance blood-pool agent for magnetic resonance imaging. Invest Radiol. 2001; 36:445–454. PMID: 11500594.
Article8. Turetschek K, Floyd E, Shames DM, Roberts TP, Preda A, Novikov V, et al. Assessment of a rapid clearance blood pool MR contrast medium (P792) for assays of microvascular characteristics in experimental breast tumors with correlations to histopathology. Magn Reson Med. 2001; 45:880–886. PMID: 11323815.
Article9. Fries P, Runge VM, Bücker A, Schürholz H, Reith W, Robert P, et al. Brain tumor enhancement in magnetic resonance imaging at 3 tesla: intraindividual comparison of two high relaxivity macromolecular contrast media with a standard extracellular gd-chelate in a rat brain tumor model. Invest Radiol. 2009; 44:200–206. PMID: 19300099.10. Kim KW, Lee JM, Jeon YS, Lee IJ, Choi Y, Park J, et al. Vascular disrupting effect of CKD-516: preclinical study using DCE-MRI. Invest New Drugs. 2013; 31:1097–1106. PMID: 23299389.
Article11. Lee J, Bae S, Lee SH, Choi H, Kim YH, Kim SJ, et al. Discovery of a potent tubulin polymerization inhibitor: synthesis and evaluation of water-soluble prodrugs of benzophenone analog. Bioorg Med Chem Lett. 2010; 20:6327–6330. PMID: 20850313.
Article12. Lee J, Kim SJ, Choi H, Kim YH, Lim IT, Yang HM, et al. Identification of CKD-516: a potent tubulin polymerization inhibitor with marked antitumor activity against murine and human solid tumors. J Med Chem. 2010; 53:6337–6354. PMID: 20690624.
Article13. Joo I, Lee JM, Han JK, Choi BI. Intravoxel incoherent motion diffusion-weighted MR imaging for monitoring the therapeutic efficacy of the vascular disrupting agent CKD-516 in rabbit VX2 liver tumors. Radiology. 2014; 272:417–426. PMID: 24697148.
Article14. Joo I, Kim JH, Lee JM, Choi JW, Han JK, Choi BI. Early quantification of the therapeutic efficacy of the vascular disrupting agent, CKD-516, using dynamic contrast-enhanced ultrasonography in rabbit VX2 liver tumors. Ultrasonography. 2014; 33:18–25. PMID: 24936491.
Article15. Tofts PS, Brix G, Buckley DL, Evelhoch JL, Henderson E, Knopp MV, et al. Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging. 1999; 10:223–232. PMID: 10508281.
Article16. Marckmann P, Skov L, Rossen K, Dupont A, Damholt MB, Heaf JG, et al. Nephrogenic systemic fibrosis: suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol. 2006; 17:2359–2362. PMID: 16885403.
Article17. van Dijke CF, Brasch RC, Roberts TP, Weidner N, Mathur A, Shames DM, et al. Mammary carcinoma model: correlation of macromolecular contrast-enhanced MR imaging characterizations of tumor microvasculature and histologic capillary density. Radiology. 1996; 198:813–818. PMID: 8628876.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Diagnosis of a Pulmonary Embolism: Comparison of P792 and Gd-DOTA for First-Pass Perfusion MRI and Contrast-Enhanced 3D MRA in a Rabbit Model
- Early quantification of the therapeutic efficacy of the vascular disrupting agent, CKD-516, using dynamic contrast-enhanced ultrasonography in rabbit VX2 liver tumors
- The Comparative Imaging Study on Mn-phthalocyanine and Mangafodipir trisodium in Experimental VX2 Animal Model
- Contrast Enhanced US in the Abdomen
- Current Limitations and Potential Breakthroughs for the Early Diagnosis of Hepatocellular Carcinoma