Neurointervention.
2023 Mar;18(1):38-46. 10.5469/neuroint.2023.00017.
Strong Contrast Stagnation of Unilateral Vertebral Artery on Three-Dimensional Black Blood-Enhanced MRI Predicts Acute Medulla Infarction
- Affiliations
-
- 1Jeonbuk National University Medical School, Jeonju, Korea
- 2Department of Radiology, Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2539945
- DOI: http://doi.org/10.5469/neuroint.2023.00017
Abstract
- Purpose
This study aimed to evaluate angiographic and contrast enhancement (CE) patterns on three-dimensional (3D) black blood (BB) contrast-enhanced MRI in patients with acute medulla infarction.
Materials and Methods
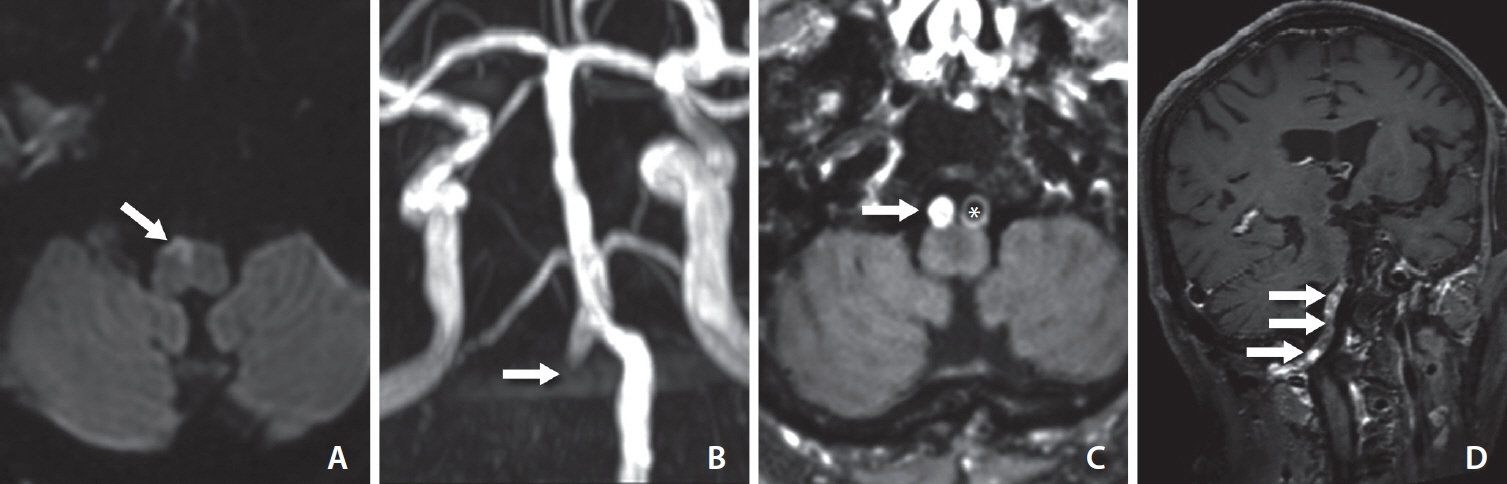
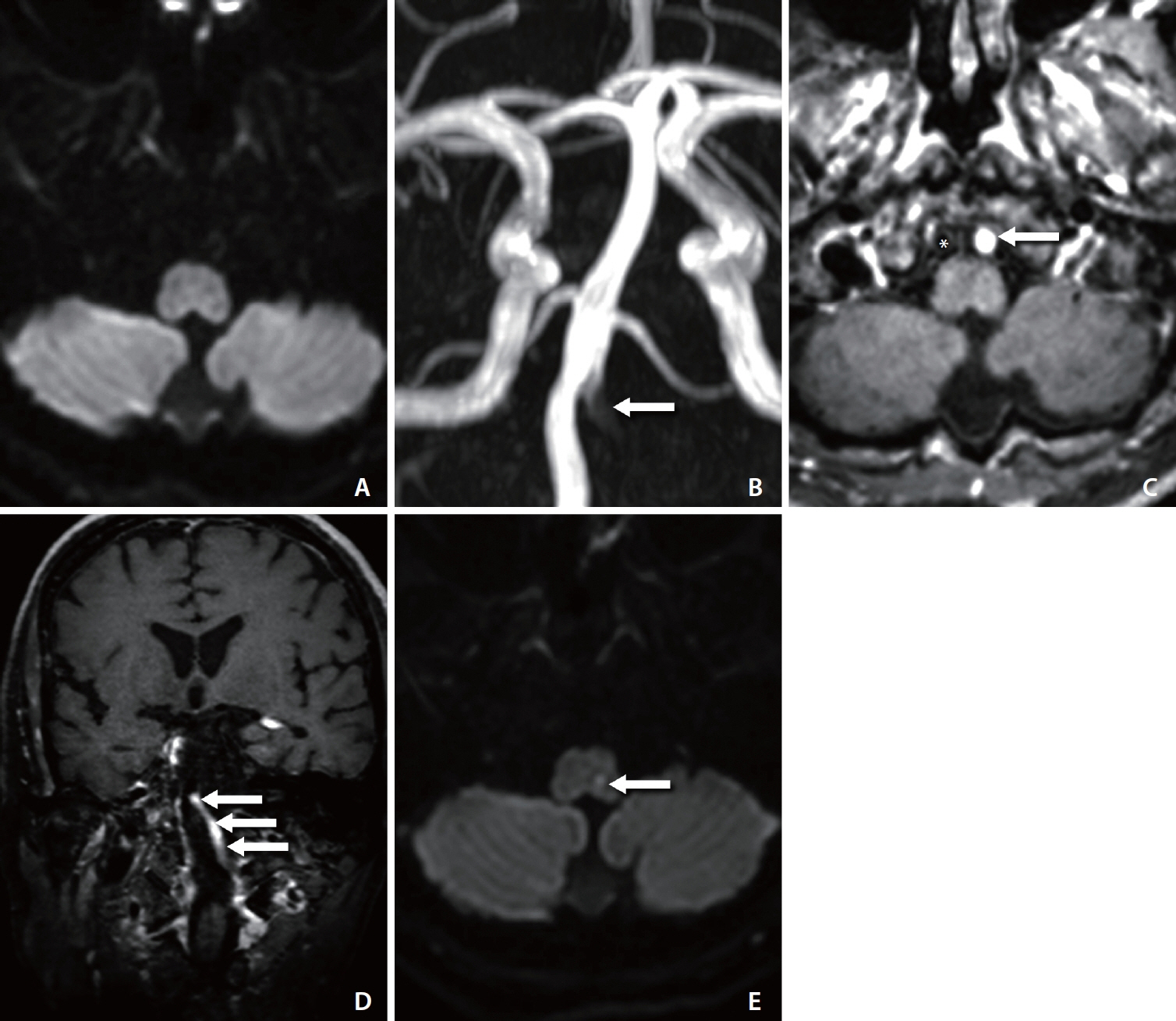
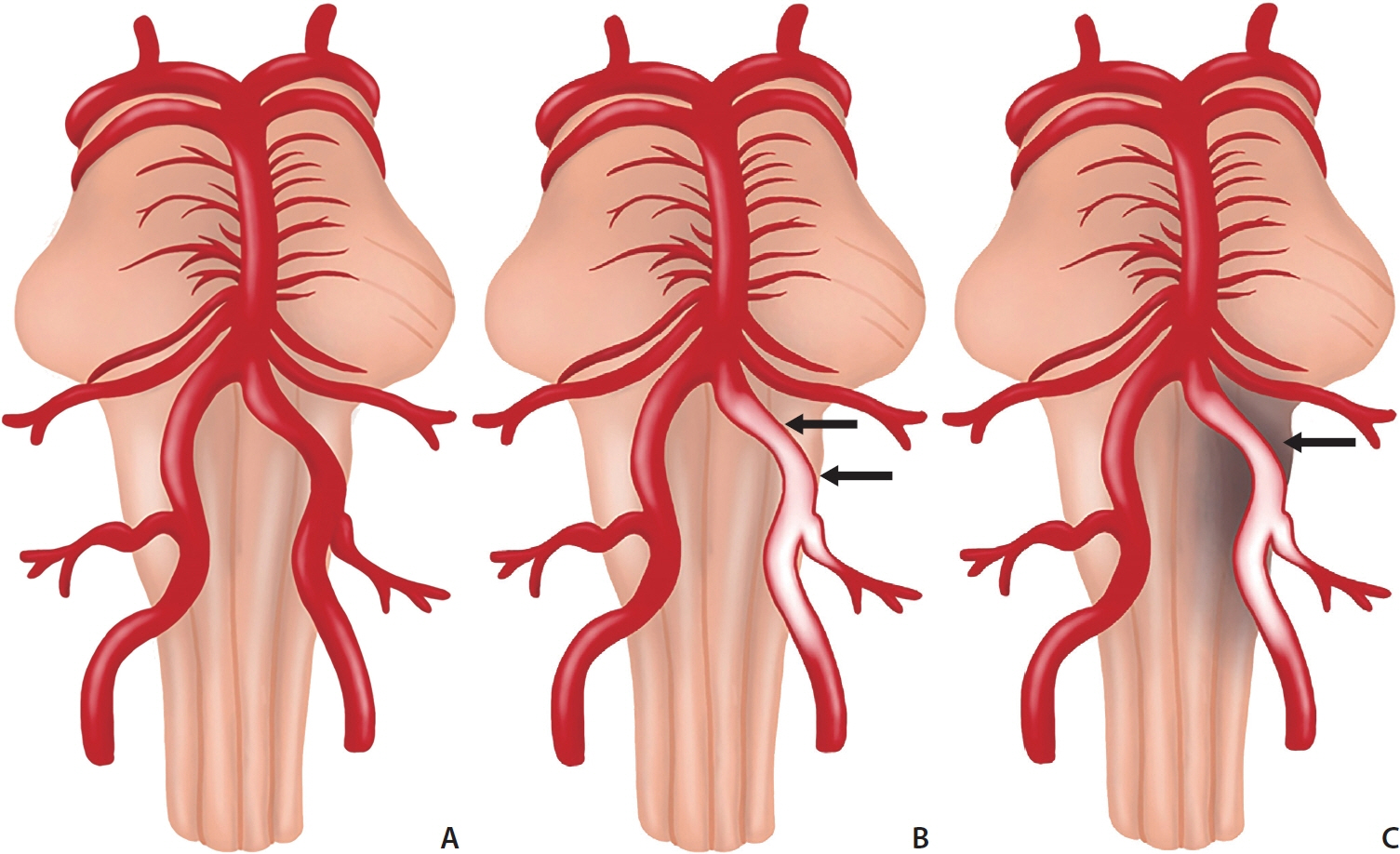
From January 2020 to August 2021, we retrospectively analyzed stroke 3D BB contrast-enhanced magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) findings of patients visiting the emergency room for symptom evaluation of acute medulla infarction. In total, 28 patients with acute medulla infarction were enrolled in this study. Four types of 3D BB contrast-enhanced MRI and MRA were classified as follows: 1=unilateral contrast-enhanced vertebral artery (VA)+no visualization of VA on MRA; 2=unilateral enhanced VA+hypoplastic VA; 3=no enhanced VA+unilateral complete occlusion of VA; 4=no enhanced VA+normal VA (including hypoplasia) on MRA.
Results
Of the 28 patients with acute medulla infarction, 7 (25.0%) showed delayed positive findings after 24 hours on diffusion-weighted imaging (DWI). Of these patients, 19 (67.9%) showed CE of the unilateral VA on 3D BB contrast-enhanced MRI (type 1 and 2). Of the 19 patients with CE of VA on 3D BB contrast-enhanced MRI, 18 showed no visualization of enhanced VA on MRA (type 1), and 1 showed hypoplastic VA. Of the 7 patients with delayed positive findings on DWI, 5 showed CE of the unilateral VA and no visualization of the enhanced VA on MRA (type 1). Symptom onset to door time or initial MR check time was significantly shorter in the groups with delayed positive findings on DWI (P<0.05).
Conclusion
Unilateral CE on 3D BB contrast-enhanced MRI and no visualization of the VA on MRA are related to the recent occlusion of the distal VA. These findings suggest that the recent occlusion of the distal VA is related to acute medulla infarction, including delayed visualization on DWI.
Keyword
Figure
Reference
-
1. Sparaco M, Ciolli L, Zini A. Posterior circulation ischaemic stroke-a review part I: anatomy, aetiology and clinical presentations. Neurol Sci. 2019; 40:1995–2006.
Article2. Ortiz de Mendivil A, Alcalá-Galiano A, Ochoa M, Salvador E, Millán JM. Brainstem stroke: anatomy, clinical and radiological findings. Semin Ultrasound CT MR. 2013; 34:131–141.
Article3. Kim K, Lee HS, Jung YH, Kim YD, Nam HS, Nam CM, et al. Mechanism of medullary infarction based on arterial territory involvement. J Clin Neurol. 2012; 8:116–122.
Article4. Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007; 369:293–298.
Article5. Oppenheim C, Stanescu R, Dormont D, Crozier S, Marro B, Samson Y, et al. False-negative diffusion-weighted MR findings in acute ischemic stroke. AJNR Am J Neuroradiol. 2000; 21:1434–1440.6. Al-Smadi AS, Abdalla RN, Elmokadem AH, Shaibani A, Hurley MC, Potts MB, et al. Diagnostic accuracy of high-resolution black-blood MRI in the evaluation of intracranial large-vessel arterial occlusions. AJNR Am J Neuroradiol. 2019; 40:954–959.
Article7. Fayad ZA, Fuster V, Fallon JT, Jayasundera T, Worthley SG, Helft G, et al. Noninvasive in vivo human coronary artery lumen and wall imaging using black-blood magnetic resonance imaging. Circulation. 2000; 102:506–510.
Article8. Jang W, Kwak HS, Chung GH, Hwang SB. Three-dimensional black-blood contrast-enhanced MRI improves detection of intraluminal thrombi in patients with acute ischaemic stroke. Eur Radiol. 2018; 28:3840–3847.
Article9. Yang H, Zhu Y, Geng Z, Li C, Zhou L, Liu QI. Clinical value of black-blood high-resolution magnetic resonance imaging for intracranial atherosclerotic plaques. Exp Ther Med. 2015; 10:231–236.
Article10. Baik SH, Kwak HS, Hwang SB, Chung GH. Three-dimensional black blood contrast enhanced magnetic resonance imaging in patients with acute ischemic stroke and negative susceptibility vessel sign. Eur J Radiol. 2018; 102:188–194.
Article11. Chung GH, Hwang SB, Kwak HS. Use of 3-dimensional, blackblood, contrast-enhanced, T1-weighted magnetic resonance imaging to identify vascular occlusion in the posterior circulation after acute ischemic stroke. J Stroke Cerebrovasc Dis. 2019; 28:104373.
Article12. Wang J, Gerretsen SC, Maki JH, Jaarsma C, Kooi ME, Herzka D, et al. Time-efficient black blood RCA wall imaging at 3T using improved motion sensitized driven equilibrium (iMSDE): feasibility and reproducibility. PLoS One. 2011; 6:e26567.
Article13. Wang J, Yarnykh VL, Yuan C. Enhanced image quality in blackblood MRI using the improved motion-sensitized driven-equilibrium (iMSDE) sequence. J Magn Reson Imaging. 2010; 31:1256–1263.
Article14. Head T, Daunert S, Goldschmidt-Clermont PJ. The aging risk and atherosclerosis: a fresh look at arterial homeostasis. Front Genet. 2017; 8:216.
Article15. Gang M, Lee H, Kwak HS, Hwang SB, Chung GH. Strong enhancement on three-dimensional black-blood enhanced magnetic resonance imaging: comparison intracranial stenosis and complete occlusion. Eur J Radiol. 2021; 137:109580.
Article16. Lee KY, Suh SH, Ahn SJ. Significance of hyperintense arteries on Gd-enhanced 3D T1W black-blood imaging in acute stroke. Eur Radiol. 2019; 29:1329–1337.
Article17. Mercier PH, Brassier G, Fournier HD, Picquet J, Papon X, Lasjaunias P. Vascular microanatomy of the pontomedullary junction, posterior inferior cerebellar arteries, and the lateral spinal arteries. Interv Neuroradiol. 2008; 14:49–58.
Article18. Kim JS, Lee JH, Choi CG. Patterns of lateral medullary infarction: vascular lesion-magnetic resonance imaging correlation of 34 cases. Stroke. 1998; 29:645–652.19. Bhin J, Kwak HS, Hwang SB, Chung GH. Comparison of imaging findings on three-dimensional black-blood enhanced MR imaging between intracranial atherosclerotic occlusion and thrombotic occlusion. J Stroke Cerebrovasc Dis. 2023; 32:106877.
Article20. Lövblad KO, Laubach HJ, Baird AE, Curtin F, Schlaug G, Edelman RR, et al. Clinical experience with diffusion-weighted MR in patients with acute stroke. AJNR Am J Neuroradiol. 1998; 19:1061–1066.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ipsilateral Hemiparesis in Lateral Medullary Infarction: As a Warning Sign of Acute Progression of Vertebral Artery Thrombosis
- Ipsilateral Posterior Spinal Artery Infarction on Lower Medulla and Upper Cervical Spinal Cord: A case report
- Cervical Spinal Cord Infarction Presenting as Chest Pain in Patients with Acute Cerebellar Infarction
- Selective Spinal Cord Infarction on Gray Matter in a Child with Injured Unilateral Vertebral Artery: A case report
- Ipsilateral Axial Lateropulsion as an Initial Symptom of Lateral Medullary Infarction: a Case Report