Cancer Res Treat.
2023 Jan;55(1):258-269. 10.4143/crt.2022.418.
Image-Guided Versus Conventional Brachytherapy for Locally Advanced Cervical Cancer: Experience of Single Institution with the Same Practitioner and Time Period
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 2Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea
- 3Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 4Institute of Radiation Medicine, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Korea
- 6Department of Radiation Oncology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 7Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul, Korea
- KMID: 2538009
- DOI: http://doi.org/10.4143/crt.2022.418
Abstract
- Purpose
This study aimed to compare treatment outcomes and toxicity profile between imaged-guided brachytherapy (IGBT) versus conventional brachytherapy (CBT) performed by the same practitioner during the same time period.
Materials and Methods
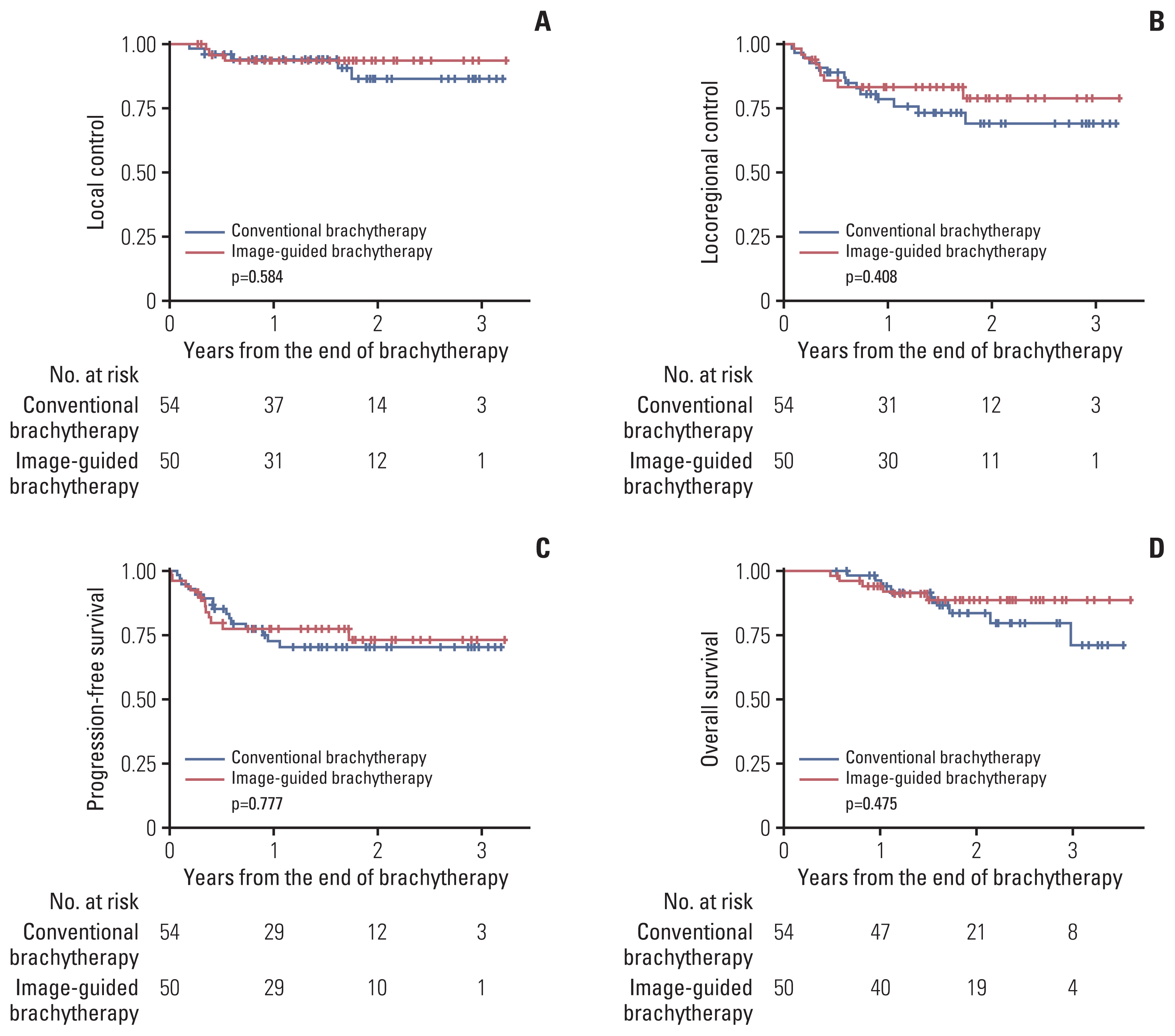
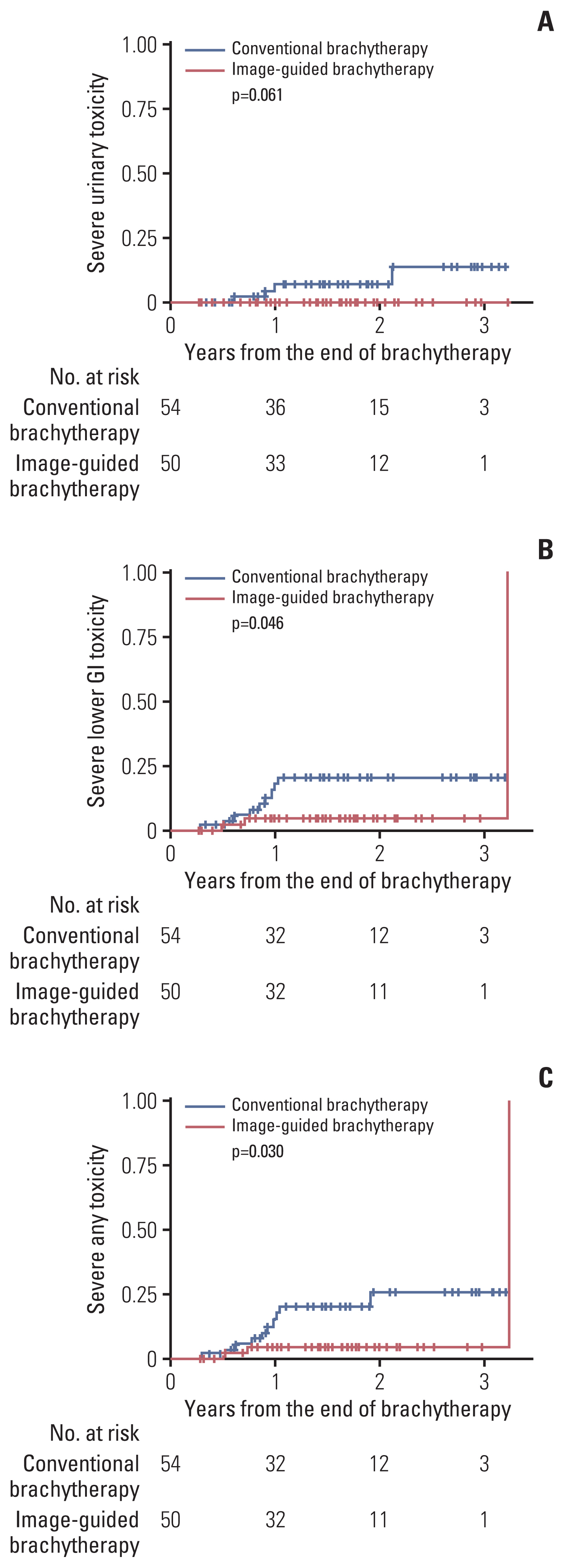
Medical records of 104 eligible patients who underwent brachytherapy for locally advanced cervical cancer were retrospectively reviewed. Fifty patients (48.1%) underwent IGBT, and 54 (51.9%) patients underwent CBT. All patients underwent concurrent chemoradiation with cisplatin. High-dose-rate intracavitary brachytherapy with dose prescription of 25-30 Gy in 4-6 fractions was performed for all patients. Late lower gastrointestinal (GI) and urinary toxicities occurred more than 3 months after the end of brachytherapy were included for comparative and dosimetric analyses.
Results
The median follow-up period was 18.33 months (range, 3.25 to 38.43 months). There were no differences in oncologic outcomes between the two groups. The IGBT group had lower rate of actuarial grade ≥ 3 toxicity than the CBT group (2-year, 4.5% vs. 25.7%; p=0.030). Cumulative equieffective D2cc of sigmoid colon was significantly correlated with grade ≥ 2 lower GI toxicity (p=0.033), while equieffective D2cc of rectum (p=0.055) and bladder (p=0.069) showed marginal significance with corresponding grade ≥ 2 toxicities in the IGBT group. Half of grade ≥ 3 lower GI toxicities impacted GI tract above the rectum. Optimal thresholds of cumulative D2cc of sigmoid colon and rectum were 69.7 Gy and 70.8 Gy, respectively, for grade ≥ 2 lower GI toxicity.
Conclusion
IGBT showed superior toxicity profile to CBT. Evaluating the dose to the GI tract above rectum by IGBT might prevent some toxicities.
Figure
Reference
-
References
1. Han K, Milosevic M, Fyles A, Pintilie M, Viswanathan AN. Trends in the utilization of brachytherapy in cervical cancer in the United States. Int J Radiat Oncol Biol Phys. 2013; 87:111–9.
Article2. Lee TH, Song C, Kim IA, Kim JS, Kim YB, Kim K, et al. Stereotactic ablative body radiotherapy boost for cervical cancer when brachytherapy boost is not feasible. Radiat Oncol. 2021; 16:148.3. Viswanathan AN, Erickson BA. Seeing is saving: the benefit of 3D imaging in gynecologic brachytherapy. Gynecol Oncol. 2015; 138:207–15.
Article4. Potter R, Tanderup K, Schmid MP, Jurgenliemk-Schulz I, Haie-Meder C, Fokdal LU, et al. MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): a multicentre prospective cohort study. Lancet Oncol. 2021; 22:538–47.5. Ohno T, Toita T, Tsujino K, Uchida N, Hatano K, Nishimura T, et al. A questionnaire-based survey on 3D image-guided brachytherapy for cervical cancer in Japan: advances and obstacles. J Radiat Res. 2015; 56:897–903.6. Kim H, Kim JY, Kim J, Park W, Kim YS, Kim HJ, et al. Current status of brachytherapy in Korea: a national survey of radiation oncologists. J Gynecol Oncol. 2016; 27:e33.7. Ha IB, Jeong BK, Kang KM, Jeong H, Lee YH, Choi HS, et al. Who really benefits from 3D-based planning of brachytherapy for cervical cancer? J Korean Med Sci. 2018; 33:e135.8. Rijkmans EC, Nout RA, Rutten IH, Ketelaars M, Neelis KJ, Laman MS, et al. Improved survival of patients with cervical cancer treated with image-guided brachytherapy compared with conventional brachytherapy. Gynecol Oncol. 2014; 135:231–8.
Article9. Thomas KM, Maquilan G, Stojadinovic S, Medin P, Folkert MR, Albuquerque K. Reduced toxicity with equivalent outcomes using three-dimensional volumetric (3DV) image-based versus nonvolumetric point-based (NV) brachytherapy in a cervical cancer population. Brachytherapy. 2017; 16:943–8.
Article10. Derks K, Steenhuijsen JL, van den Berg HA, Houterman S, Cnossen J, van Haaren P, et al. Impact of brachytherapy technique (2D versus 3D) on outcome following radiotherapy of cervical cancer. J Contemp Brachytherapy. 2018; 10:17–25.
Article11. Lim K, Small W Jr, Portelance L, Creutzberg C, Jurgenliemk-Schulz IM, Mundt A, et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy for the definitive treatment of cervix cancer. Int J Radiat Oncol Biol Phys. 2011; 79:348–55.
Article12. Mayadev J, Nunes AT, Li M, Marcovitz M, Lanasa MC, Monk BJ. CALLA: Efficacy and safety of concurrent and adjuvant durvalumab with chemoradiotherapy versus chemoradiotherapy alone in women with locally advanced cervical cancer: a phase III, randomized, double-blind, multicenter study. Int J Gynecol Cancer. 2020; 30:1065–70.
Article13. ICRU Report 38 Dose and volume specification for reporting intracavitary therapy in gynaecology. Bethesda, MD: International Commission on Radiation Units and Measurements;1985.14. Haie-Meder C, Potter R, Van Limbergen E, Briot E, De Brabandere M, Dimopoulos J, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005; 74:235–45.
Article15. Common Terminology Criteria for Adverse Events (CTCAE) v5.0 [Internet]. Bethesda, MD: National Cancer Institute;c2017. [cited 2022 Aug 1]. Available from: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm .16. Kim YJ, Kang HC, Kim YS. Impact of intracavitary brachytherapy technique (2D versus 3D) on outcomes of cervical cancer: a systematic review and meta-analysis. Strahlenther Onkol. 2020; 196:973–82.
Article17. Suzumura EA, Gama LM, Jahn B, Campolina AG, Carvalho HA, de Soarez PC. Effects of 3D image-guided brachytherapy compared to 2D conventional brachytherapy on clinical outcomes in patients with cervical cancer: a systematic review and meta-analyses. Brachytherapy. 2021; 20:710–37.
Article18. Lindegaard JC, Fokdal LU, Nielsen SK, Juul-Christensen J, Tanderup K. MRI-guided adaptive radiotherapy in locally advanced cervical cancer from a Nordic perspective. Acta Oncol. 2013; 52:1510–9.
Article19. Lin AJ, Kidd E, Dehdashti F, Siegel BA, Mutic S, Thaker PH, et al. Intensity modulated radiation therapy and image-guided adapted brachytherapy for cervix cancer. Int J Radiat Oncol Biol Phys. 2019; 103:1088–97.20. Sturdza A, Potter R, Fokdal LU, Haie-Meder C, Tan LT, Mazeron R, et al. Image guided brachytherapy in locally advanced cervical cancer: Improved pelvic control and survival in RetroEMBRACE, a multicenter cohort study. Radiother Oncol. 2016; 120:428–33.
Article21. Viswanathan AN, Beriwal S, De Los Santos JF, Demanes DJ, Gaffney D, Hansen J, et al. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: high-dose-rate brachytherapy. Brachytherapy. 2012; 11:47–52.
Article22. Mazeron R, Fokdal LU, Kirchheiner K, Georg P, Jastaniyah N, Segedin B, et al. Dose-volume effect relationships for late rectal morbidity in patients treated with chemoradiation and MRI-guided adaptive brachytherapy for locally advanced cervical cancer: results from the prospective multicenter EMBRACE study. Radiother Oncol. 2016; 120:412–9.
Article23. Georg P, Potter R, Georg D, Lang S, Dimopoulos JC, Sturdza AE, et al. Dose effect relationship for late side effects of the rectum and urinary bladder in magnetic resonance image-guided adaptive cervix cancer brachytherapy. Int J Radiat Oncol Biol Phys. 2012; 82:653–7.
Article24. Spampinato S, Fokdal LU, Potter R, Haie-Meder C, Lindegaard JC, Schmid MP, et al. Risk factors and dose-effects for bladder fistula, bleeding and cystitis after radiotherapy with imaged-guided adaptive brachytherapy for cervical cancer: an EMBRACE analysis. Radiother Oncol. 2021; 158:312–20.
Article25. Wachter-Gerstner N, Wachter S, Reinstadler E, Fellner C, Knocke TH, Wambersie A, et al. Bladder and rectum dose defined from MRI based treatment planning for cervix cancer brachytherapy: comparison of dose-volume histograms for organ contours and organ wall, comparison with ICRU rectum and bladder reference point. Radiother Oncol. 2003; 68:269–76.
Article26. Holloway CL, Racine ML, Cormack RA, O’Farrell DA, Viswanathan AN. Sigmoid dose using 3D imaging in cervical-cancer brachytherapy. Radiother Oncol. 2009; 93:307–10.
Article27. Ko HC, Huang JY, Miller JR, Das RK, Wallace CR, De Costa AA, et al. Novel use of ViewRay MRI guidance for high-dose-rate brachytherapy in the treatment of cervical cancer. Brachytherapy. 2018; 17:680–8.
Article28. Chen X, Zou H, Li H, Lin R, Su M, Zhang W, et al. Weekly versus triweekly cisplatin-based chemotherapy concurrent with radiotherapy in the treatment of cervical cancer: a meta-analysis. Int J Gynecol Cancer. 2017; 27:344–9.
Article29. Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012; 13:e212–20.
Article30. Kemp A. Update on CALLA Phase III trial of concurrent use of Imfinzi and chemoradiotherapy in locally advanced cervical cancer [Internet]. Cambridge: AstraZeneca PLC;c2022. [cited 2022 May 26]. Available from: https://www.astrazeneca.com/media-centre/press-releases/2022/update-on-calla-phase-iii-trial-for-imfinzi.html .31. Schmid MP, Kirisits C, Nesvacil N, Dimopoulos JC, Berger D, Potter R. Local recurrences in cervical cancer patients in the setting of image-guided brachytherapy: a comparison of spatial dose distribution within a matched-pair analysis. Radiother Oncol. 2011; 100:468–72.
Article32. Mignot F, Gouy S, Schernberg A, Bockel S, Espenel S, Maulard A, et al. Comprehensive analysis of patient outcome after local recurrence of locally advanced cervical cancer treated with concomitant chemoradiation and image-guided adaptive brachytherapy. Gynecol Oncol. 2020; 157:644–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The using of megavoltage computed tomography in image-guided brachytherapy for cervical cancer: a case report
- The ideal strategies of chemotherapy for the treatment of cervical cancer
- Management for locally advanced cervical cancer: new trends and controversial issues
- Present status of worldwide clinical trials about uterine cervical cancer
- Radiation sigmoiditis mimicking sigmoid colon cancer after radiation therapy for cervical cancer: the implications of three-dimensional image-based brachytherapy planning