Clin Endosc.
2021 May;54(3):413-419. 10.5946/ce.2020.126.
Novel Ablation Therapy Using Endoscopic Irreversible Electroporation in the Bile Duct: A Pilot Animal Study
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea
- 3Department of Biosystems and Biomaterials Science and Engineering, Seoul National University, Seoul, Korea
- KMID: 2516322
- DOI: http://doi.org/10.5946/ce.2020.126
Abstract
- Background/Aims
Irreversible electroporation (IRE) is a relatively new ablation method. However, the application of IRE ablation in the treatment of biliary disease has not been attempted. A minimally invasive approach using endoscopic retrograde cholangiopancreatography (ERCP) can be a novel therapeutic modality for IRE ablation. In this study, we aimed to investigate the feasibility of endoscopic IRE for the biliary tract using an animal model.
Methods
A new catheter-type electrode was developed for endoscopic IRE ablation of the biliary tract. We performed ERCP and endoscopic IRE ablations in the normal common bile duct of Yorkshire pigs. The experimental setting of IRE was 500 V/cm (50 pulses, 100-µs length). The animals were sacrificed after 24 hr, and the ablated bile duct was examined.
Results
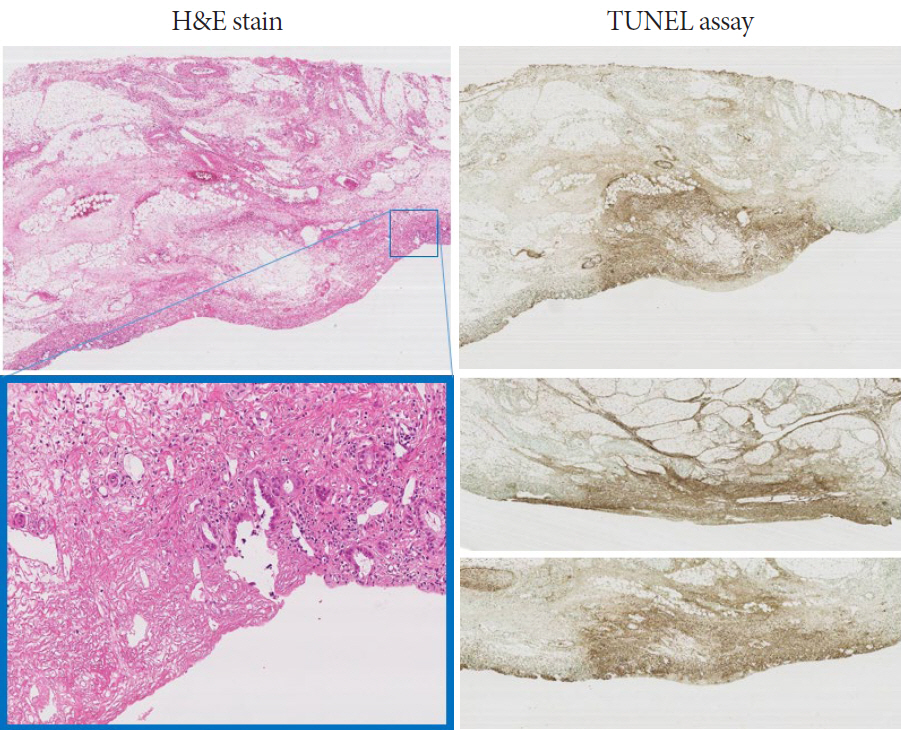
Well-demarcated focal color changes were observed on the mucosa of the common bile duct. The depth of change after IRE was confined to the mucosal and submucosal layers. Apoptotic changes in the bile duct were observed only around the IRE ablation area. Immunohistochemistry assay showed cell death in the bile duct along the electrode.
Conclusions
Endoscopic IRE ablation using ERCP was successfully performed in the common bile duct. It can be a potential option for the treatment of biliary tumors.
Keyword
Figure
Cited by 1 articles
-
Large Animal Models in Pancreas and Biliary Disease
Seok Jeong, Jin-Seok Park, Don Haeng Lee
Korean J Gastroenterol. 2021;77(3):99-103. doi: 10.4166/kjg.2021.031.
Reference
-
1. Murakami Y, Uemura K, Sudo T, et al. Prognostic factors after surgical resection for intrahepatic, hilar, and distal cholangiocarcinoma. Ann Surg Oncol. 2011; 18:651–658.
Article2. Koch C, Franzke C, Bechstein WO, et al. Poor prognosis of advanced cholangiocarcinoma: real-world data from a tertiary referral center. Digestion. 2020; 101:458–465.
Article3. Aljiffry M, Walsh MJ, Molinari M. Advances in diagnosis, treatment and palliation of cholangiocarcinoma: 1990-2009. World J Gastroenterol. 2009; 15:4240–4262.
Article4. Wagstaff PG, Buijs M, van den Bos W, et al. Irreversible electroporation: state of the art. Onco Targets Ther. 2016; 9:2437–2446.
Article5. Curley SA, Marra P, Beaty K, et al. Early and late complications after radiofrequency ablation of malignant liver tumors in 608 patients. Ann Surg. 2004; 239:450–458.
Article6. Rubinsky B, Onik G, Mikus P. Irreversible electroporation: a new ablation modality--clinical implications. Technol Cancer Res Treat. 2007; 6:37–48.7. Weaver JC, Chizmadzhev YA. Theory of electroporation: a review. Bioelectrochem Bioenerg. 1996; 41:135–160.
Article8. Miller L, Leor J, Rubinsky B. Cancer cells ablation with irreversible electroporation. Technol Cancer Res Treat. 2005; 4:699–705.
Article9. Belfiore MP, Ronza FM, Romano F, et al. Percutaneous CT-guided irreversible electroporation followed by chemotherapy as a novel neoadjuvant protocol in locally advanced pancreatic cancer: our preliminary experience. Int J Surg. 2015; 21(Suppl 1):S34–S39.
Article10. Hsiao CY, Huang KW. Irreversible electroporation: a novel ultrasound-guided modality for non-thermal tumor ablation. J Med Ultrasound. 2017; 25:195–200.
Article11. Lee JM, Choi HS, Chun HJ, et al. EUS-guided irreversible electroporation using endoscopic needle-electrode in porcine pancreas. Surg Endosc. 2019; 33:658–662.
Article12. Lee JM, Choi HS, Kim ES, et al. Characterization of irreversible electroporation on the stomach: a feasibility study in rats. Sci Rep. 2019; 9:9094.
Article13. Davalos RV, Mir IL, Rubinsky B. Tissue ablation with irreversible electroporation. Ann Biomed Eng. 2005; 33:223–231.
Article14. Edd JF, Horowitz L, Davalos RV, Mir LM, Rubinsky B. In vivo results of a new focal tissue ablation technique: irreversible electroporation. IEEE Trans Biomed Eng. 2006; 53:1409–1415.
Article15. Jung CFM, Lavole J, Barret M, et al. Local therapy in advanced cholangiocarcinoma: a review of current endoscopic, medical, and oncologic treatment options. Oncology. 2019; 97:191–201.
Article16. Scheffer HJ, Nielsen K, de Jong MC, et al. Irreversible electroporation for nonthermal tumor ablation in the clinical setting: a systematic review of safety and efficacy. J Vasc Interv Radiol. 2014; 25:997–1011. quiz 1011.
Article17. Usman M, Moore W, Talati R, Watkins K, Bilfinger TV. Irreversible electroporation of lung neoplasm: a case series. Med Sci Monit. 2012; 18:CS43–CS47.
Article18. Moir J, White SA, French JJ, Littler P, Manas DM. Systematic review of irreversible electroporation in the treatment of advanced pancreatic cancer. Eur J Surg Oncol. 2014; 40:1598–1604.
Article19. Sutter O, Calvo J, N’Kontchou G, et al. Safety and efficacy of irreversible electroporation for the treatment of hepatocellular carcinoma not amenable to thermal ablation techniques: a retrospective single-center case series. Radiology. 2017; 284:877–886.
Article20. Murray KS, Ehdaie B, Musser J, et al. Pilot study to assess safety and clinical outcomes of irreversible electroporation for partial gland ablation in men with prostate cancer. J Urol. 2016; 196:883–890.
Article21. Luo X, Liang X, Li J, et al. The effects of irreversible electroporation on the colon in a porcine model. PLoS One. 2016; 11:e0167275.
Article22. Lee EW, Wong D, Tafti BA, et al. Irreversible electroporation in eradication of rabbit VX2 liver tumor. J Vasc Interv Radiol. 2012; 23:833–840.
Article23. Zhang W, Wang W, Chai W, et al. Breast tissue ablation with irreversible electroporation in rabbits: a safety and feasibility study. PLoS One. 2017; 12:e0181555.
Article24. Cvetković DM, Živanović MN, Milutinović MG, et al. Real-time monitoring of cytotoxic effects of electroporation on breast and colon cancer cell lines. Bioelectrochemistry. 2017; 113:85–94.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Research Status of Irreversible Electroporation for Hollow Viscus Organ of Gastrointestinal Tract
- Irreversible electroporation of hepatocellular carcinoma: the role of ultrasonography
- Irreversible Electroporation: A Novel Image-Guided Cancer Therapy
- Is electrocardiogram-gated irreversible electroporation still effective in liver ablation? A validation study in swine liver irreversible electroporation model
- Irreversible Electroporation of a Hepatocellular Carcinoma Lesion Adjacent to a Transjugular Intrahepatic Portosystemic Shunt Stent Graft