Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):39-45. 10.14701/ahbps.2021.25.1.39.
Clinical usefulness of T1-weighted MR cholangiography with Gd-EOB-DTPA for the evaluation of biliary complication after liver transplantation
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2513174
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.39
Abstract
- Backgrounds/Aims
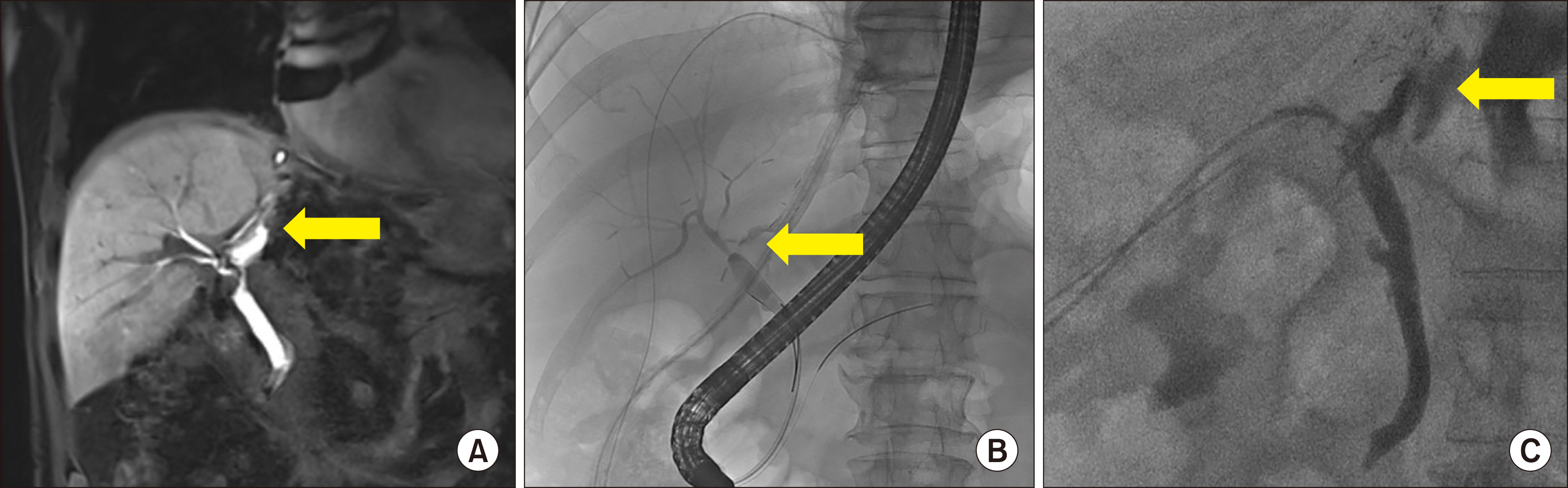
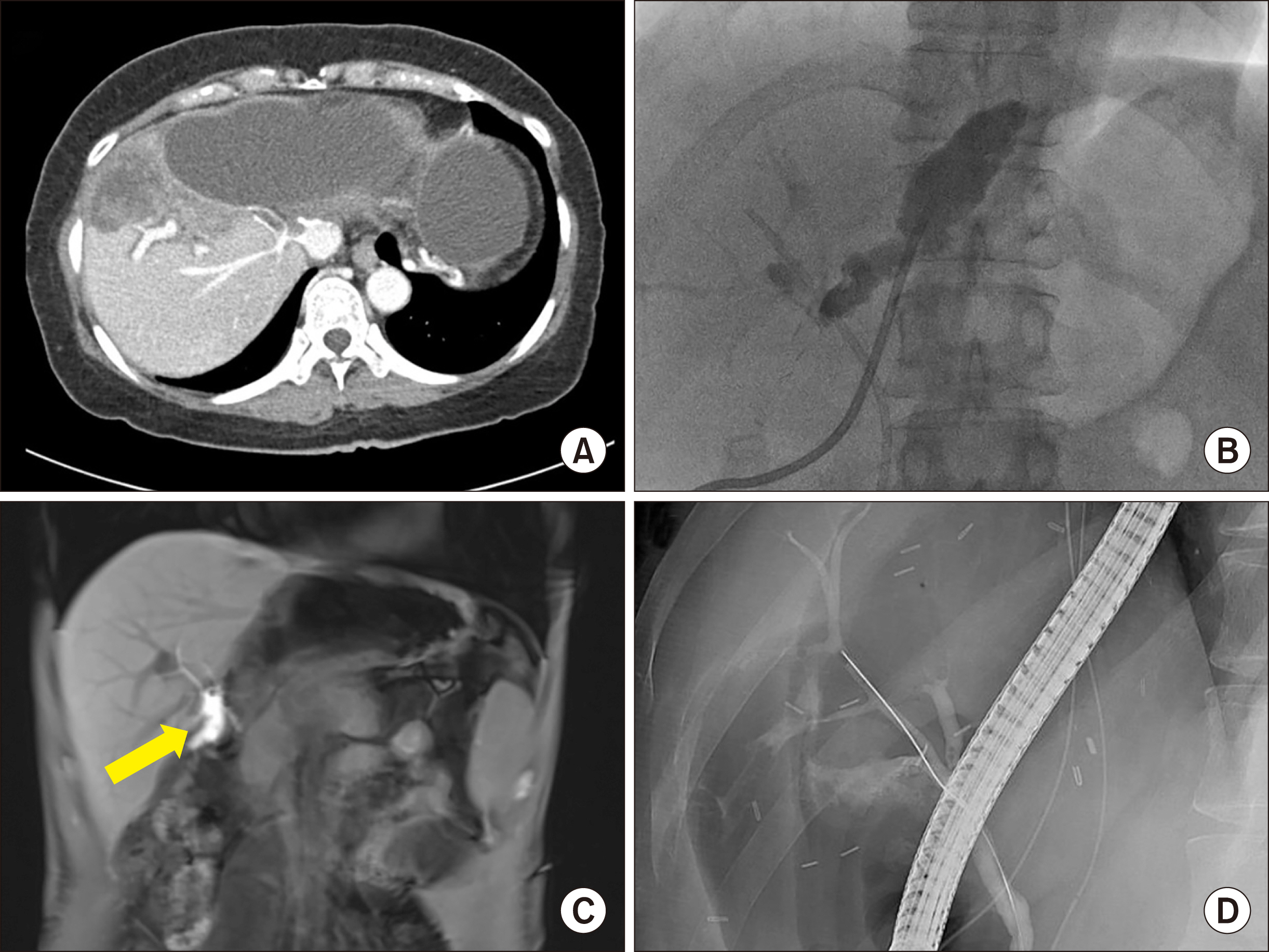
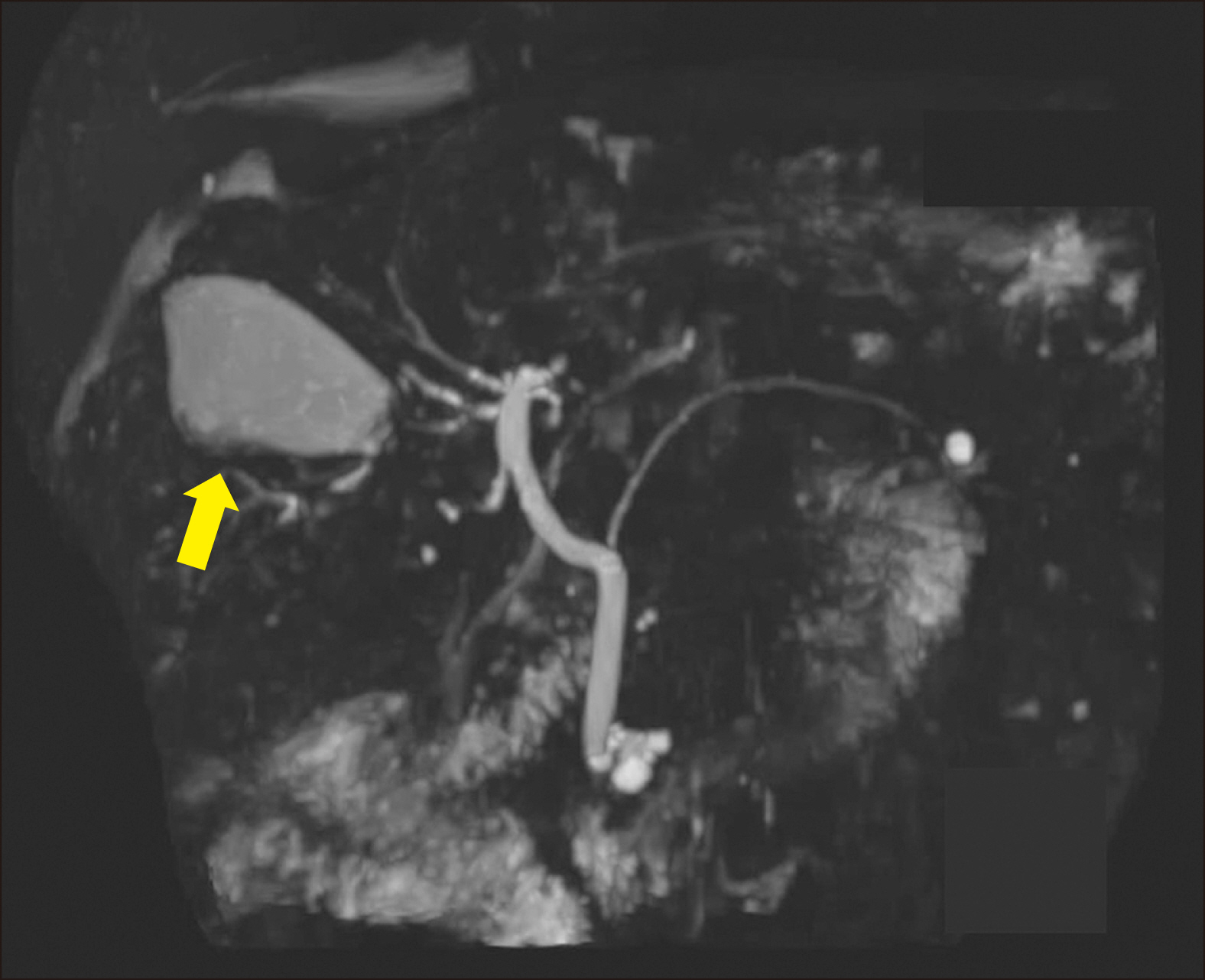
Biliary complications continue to be the major morbidity and mortality causes following living donor liver transplantation (LT). Endoscopic retrograde cholangiopancreatography (ERCP) has been performed to identify the biliary leakage source. However, this can lead to retrograde cholangitis and pancreatitis, and is not sufficient to diagnose bile leakage from cuts’ surface. This study aimed to describe the use of T1-Weighted Magnetic Resonance (MR) Cholangiography with Gd-EOB-DTPA (Primovist) examination for evaluating the bile duct complication following LT.
Methods
From March 2012 to December 2018, 869 adult LT were performed at the Seoul National University Hospital.Forty-three recipients had undergone MR Cholangiography with Gd-EOB-DTPA. We reviewed these cases with their clinical outcomes and described the utility of the MR cholangiography with Gd-EOB-DTPA.
Results
In radiologic examinations performed in the patients suspected of bile duct complication, 95% had bile leakage and stricture. Cut surface leakage was diagnosed in two cases, and biliary leakage from the anastomosis site was diagnosed in the others. Most patients with leakage had undergone percutaneous drainage and ERCP, which was performed to evaluate the bile secretion function of the hepatocytes. There was no contrast-enhanced bile duct image in one case with severe rejection, and it might have been related to hepatocyte secretary dysfunction.
Conclusions
T1-Weighted MR Cholangiography with Gd-EOB-DTPA 40-minute delay examination is a feasible and safe non-invasive procedure for identifying biliary leakage sites.
Figure
Reference
-
1. Woo HY, Lee IS, Chang JH, Youn SB, Bae SH, Choi JY, et al. 2018; Outcome of donor biliary complications following living donor liver transplantation. Korean J Intern Med. 33:705–715. DOI: 10.3904/kjim.2017.264. PMID: 29529841. PMCID: PMC6030404.
Article2. Nakamura T, Iida T, Ushigome H, Osaka M, Masuda K, Matsuyama T, et al. 2017; Risk factors and management for biliary complications following adult living-donor liver transplantation. Ann Transplant. 22:671–676. DOI: 10.12659/AOT.905485. PMID: 29114099. PMCID: PMC6248092.
Article3. Chang JH, Lee I, Choi MG, Han SW. 2016; Current diagnosis and treatment of benign biliary strictures after living donor liver transplantation. World J Gastroenterol. 22:1593–1606. DOI: 10.3748/wjg.v22.i4.1593. PMID: 26819525. PMCID: PMC4721991.
Article4. Axelrod DA, Lentine KL, Xiao H, Dzebisashvilli N, Schnitzler M, Tuttle-Newhall JE, et al. 2014; National assessment of early biliary complications following liver transplantation: incidence and outcomes. Liver Transpl. 20:446–456. DOI: 10.1002/lt.23829. PMID: 24478266.
Article5. Hwang S, Lee SG, Sung KB, Park KM, Kim KH, Ahn CS, et al. 2006; Long-term incidence, risk factors, and management of biliary complications after adult living donor liver transplantation. Liver Transpl. 12:831–838. DOI: 10.1002/lt.20693. PMID: 16528711.
Article6. Kim JM, Cho W, Kwon CHD, Joh JW, Park JB, Ko JS, et al. 2014; Bile duct reconstruction by a young surgeon in living donor liver transplantation using right liver graft. Medicine (Baltimore). 93:e84. DOI: 10.1097/MD.0000000000000084. PMID: 25255023. PMCID: PMC4616285.
Article7. Suh KS, Suh SW, Lee JM, Choi Y, Yi NJ, Lee KW. 2015; Recent advancements in and views on the donor operation in living donor liver transplantation: a single-center study of 886 patients over 13 years. Liver Transpl. 21:329–338. DOI: 10.1002/lt.24061. PMID: 25488794.
Article8. Eckenschwiller M, Ackermann H, Bechstein WO, Grünwald F. 2016; Accuracy of hepatobiliary scintigraphy after liver transplantation and liver resection. Int J Mol Imaging. 2016:7857849. DOI: 10.1155/2016/7857849. PMID: 27563464. PMCID: PMC4987481.
Article9. de Graaf W, Bennink RJ, Veteläinen R, van Gulik TM. 2010; Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med. 51:742–752. DOI: 10.2967/jnumed.109.069435. PMID: 20395336.
Article10. Cai L, Yeh BM, Westphalen AC, Roberts J, Wang ZJ. 2017; 3D T2-weighted and Gd-EOB-DTPA-enhanced 3D T1-weighted MR cholangiography for evaluation of biliary anatomy in living liver donors. Abdom Radiol (NY). 42:842–850. DOI: 10.1007/s00261-016-0936-z. PMID: 27714420.
Article11. Boraschi P, Donati F, Gigoni R, Filipponi F. 2016; Biliary complications following orthotopic liver transplantation: may contrast-enhanced MR Cholangiography provide additional information? Eur J Radiol Open. 3:108–116. DOI: 10.1016/j.ejro.2016.05.003. PMID: 27331082. PMCID: PMC4906040.
Article12. Xu YB, Bai YL, Min ZG, Qin SY. 2013; Magnetic resonance cholangiography in assessing biliary anatomy in living donors: a meta-analysis. World J Gastroenterol. 19:8427–8434. DOI: 10.3748/wjg.v19.i45.8427. PMID: 24363536. PMCID: PMC3857468.
Article13. Boraschi P, Donati F, Gigoni R, Volpi A, Salemi S, Filipponi F, et al. 2010; MR cholangiography in orthotopic liver transplantation: sensitivity and specificity in detecting biliary complications. Clin Transplant. 24:E82–E87. DOI: 10.1111/j.1399-0012.2009.01190.x. PMID: 20041910.
Article14. Boraschi P, Braccini G, Gigoni R, Sartoni G, Neri E, Filipponi F, et al. 2001; Detection of biliary complications after orthotopic liver transplantation with MR cholangiography. Magn Reson Imaging. 19:1097–1105. DOI: 10.1016/S0730-725X(01)00443-X. PMID: 11711234.
Article15. Kul M, Erden A, Düşünceli Atman E. 2017; Diagnostic value of Gd-EOB-DTPA-enhanced MR cholangiography in non-invasive detection of postoperative bile leakage. Br J Radiol. 90:20160847. DOI: 10.1259/bjr.20160847. PMID: 28181823. PMCID: PMC5605073.
Article16. Kim YJ, Lee KT, Jo YC, Lee KH, Lee JK, Joh JW, et al. 2011; Hepatobiliary scintigraphy for detecting biliary strictures after living donor liver transplantation. World J Gastroenterol. 17:2626–2631. DOI: 10.3748/wjg.v17.i21.2626. PMID: 21677831. PMCID: PMC3110925.
Article17. Arun S, Santhosh S, Sood A, Bhattacharya A, Mittal BR. 2013; Added value of SPECT/CT over planar Tc-99m mebrofenin hepatobiliary scintigraphy in the evaluation of bile leaks. Nucl Med Commun. 34:459–466. DOI: 10.1097/MNM.0b013e3283601098. PMID: 23503002.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Utility of Three-Dimensional of the T1-Weighted MR Cholangiography with Gd-EOB-DTPA for the Evaluation of a Common Bile Duct Obstruction
- Confident Diagnosis of Bronchobiliary Fistula Using Contrast-Enhanced Magnetic Resonance Cholangiography
- Enhancement Pattern of Liver Parenchyma during Late Dynamic Phase Imaging: Comparison between Gd-EOB-DTPA and Gd-DTPA-BMA
- Supradiaphragmatic Liver Confirmed by a Hepatocyte-specific Contrast Agent (Gd-EOB-DTPA): A Case Report
- MR Imaging of Experimentally Induced Primary Hepatic Tumors in Rats: Usefulness of Gadolinium-ethoxybenzyl-DTPA