Chonnam Med J.
2020 Jan;56(1):27-35. 10.4068/cmj.2020.56.1.27.
Impacts of Coronary Artery Calcification on Intradialytic Blood Pressure Patterns in Patients Receiving Maintenance Hemodialysis
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea. junghoshin@cau.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2468143
- DOI: http://doi.org/10.4068/cmj.2020.56.1.27
Abstract
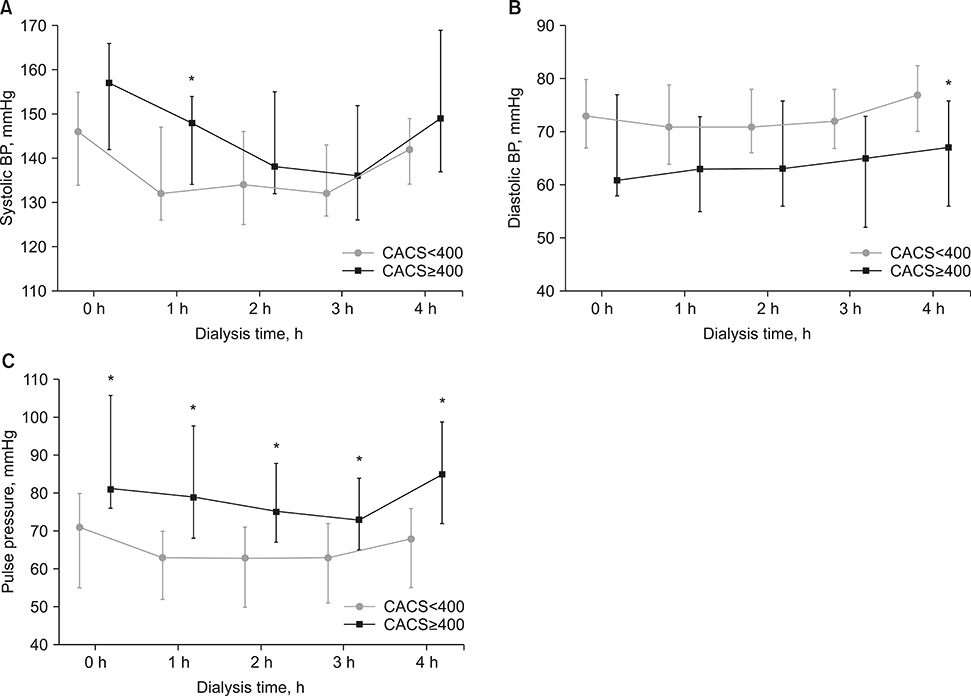
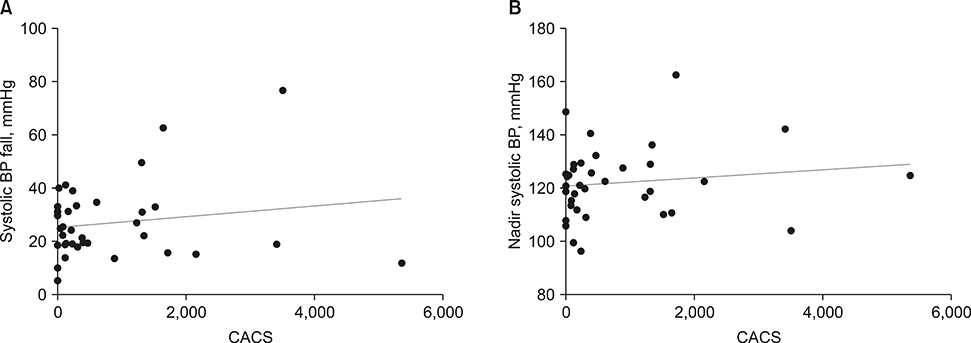
- Intradialytic blood pressure abnormalities are associated with adverse outcomes in patients with end-stage renal disease on dialysis. Vascular calcification is a common complicating feature, but whether this complication results in intradialytic blood pressure abnormalities remains uncertain. Therefore, this study investigated the relationship between coronary artery calcium score and intradialytic blood pressure abnormalities in patients with end-stage renal disease on maintenance hemodialysis. Thirty-six patients who received nongated chest computed tomography scans were included. Intradialytic hypotension was defined as a minimum intradialytic systolic blood pressure of <100 mmHg or a pre-dialysis blood pressure - minimum intradialytic systolic blood pressure >30 mmHg. Intradialytic hypertension was defined as >10 mmHg increase in systolic blood pressure (pre- to post-dialysis). Patients were classified as 22 (61.1%) with coronary artery calcium score <400 and 14 (38.9%) with coronary artery calcium score ≥400. Median systolic and diastolic blood pressures were equivalent, but median pulse pressure was higher in patients with coronary artery calcium score ≥400 than in those with scores <400. Coronary artery calcium score was comparable according to both intradialytic hypotension and hypertension, and had no correlation with systolic blood pressure fall and nadir systolic blood pressure. Coronary artery calcium score predicted the occurrence of cardiovascular events and all-cause mortality (hazard ratio 1.001 and 1.001; p=0.058 and 0.010). Coronary vascular calcification could be irrelevant to intradialytic blood pressure abnormalities in patients with end-stage renal disease on dialysis.
MeSH Terms
Figure
Reference
-
1. Dinesh K, Kunaparaju S, Cape K, Flythe JE, Feldman HI, Brunelli SM. A model of systolic blood pressure during the course of dialysis and clinical factors associated with various blood pressure behaviors. Am J Kidney Dis. 2011; 58:794–803.
Article2. Assimon MM, Flythe JE. Intradialytic blood pressure abnormalities: the highs, the lows and all that lies between. Am J Nephrol. 2015; 42:337–350.
Article3. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004; 351:1296–1305.
Article4. Stenvinkel P, Carrero JJ, Axelsson J, Lindholm B, Heimbürger O, Massy Z. Emerging biomarkers for evaluating cardiovascular risk in the chronic kidney disease patient: how do new pieces fit into the uremic puzzle? Clin J Am Soc Nephrol. 2008; 3:505–521.
Article5. Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000; 342:1478–1483.
Article6. Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension. 2001; 38:938–942.
Article7. Okuno S, Ishimura E, Kitatani K, Fujino Y, Kohno K, Maeno Y, et al. Presence of abdominal aortic calcification is significantly associated with all-cause and cardiovascular mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2007; 49:417–425.
Article8. Kim SY, Hong YA, Yoon HE, Chang YK, Yang CW, Kim SY, et al. Vascular calcification and intradialytic hypotension in hemodialysis patients: clinical relevance and impact on morbidity and mortality. Int J Cardiol. 2016; 217:156–160.
Article9. Cho A, Lee YK, Oh J, Yoon JW, Shin DH, Jeon HJ, et al. The relationship between intradialytic hypotension and vascular calcification in hemodialysis patients. PLoS One. 2017; 12:e0185846.
Article10. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832.
Article11. Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM. Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol. 2015; 26:724–734.
Article12. Inrig JK, Patel UD, Toto RD, Szczech LA. Association of blood pressure increases during hemodialysis with 2-year mortality in incident hemodialysis patients: a secondary analysis of the Dialysis Morbidity and Mortality Wave 2 Study. Am J Kidney Dis. 2009; 54:881–890.
Article13. Davies SJ, Davenport A. The role of bioimpedance and biomarkers in helping to aid clinical decision-making of volume assessments in dialysis patients. Kidney Int. 2014; 86:489–496.
Article14. Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med. 2000; 108:609–613.
Article15. Depner TA, Daugirdas JT. Equations for normalized protein catabolic rate based on two-point modeling of hemodialysis urea kinetics. J Am Soc Nephrol. 1996; 7:780–785.
Article16. Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010; 303:1610–1616.
Article17. Kirsch J, Buitrago I, Mohammed TL, Gao T, Asher CR, Novaro GM. Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging. 2012; 28:1249–1256.
Article18. Hecht HS, Cronin P, Blaha MJ, Budoff MJ, Kazerooni EA, Narula J, et al. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: a report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J Cardiovasc Comput Tomogr. 2017; 11:74–84.
Article19. Civilibal M, Caliskan S, Kurugoglu S, Candan C, Canpolat N, Sever L, et al. Progression of coronary calcification in pediatric chronic kidney disease stage 5. Pediatr Nephrol. 2009; 24:555–563.
Article20. Xie X, Zhao Y, de Bock GH, de Jong PA, Mali WP, Oudkerk M, et al. Validation and prognosis of coronary artery calcium scoring in nontriggered thoracic computed tomography: systematic review and meta-analysis. Circ Cardiovasc Imaging. 2013; 6:514–521.
Article21. Hughes-Austin JM, Dominguez A 3rd, Allison MA, Wassel CL, Rifkin DE, Morgan CG, et al. Relationship of coronary calcium on standard chest CT scans with mortality. JACC Cardiovasc Imaging. 2016; 9:152–159.
Article22. Guérin AP, London GM, Marchais SJ, Metivier F. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant. 2000; 15:1014–1021.
Article23. Raggi P, Bellasi A, Ferramosca E, Islam T, Muntner P, Block GA. Association of pulse wave velocity with vascular and valvular calcification in hemodialysis patients. Kidney Int. 2007; 71:802–807.
Article24. Haydar AA, Covic A, Colhoun H, Rubens M, Goldsmith DJ. Coronary artery calcification and aortic pulse wave velocity in chronic kidney disease patients. Kidney Int. 2004; 65:1790–1794.
Article25. Kooman J, Basci A, Pizzarelli F, Canaud B, Haage P, Fouque D, et al. EBPG guideline on haemodynamic instability. Nephrol Dial Transplant. 2007; 22 Suppl 2:ii22–ii44.
Article26. Shin J, Yeo S, Hong JY, Hwang JH, Kim SH. Impact of intradialytic blood pressure changes on cardiovascular outcomes is independent of the volume status of maintenance hemodialysis patients. J Am Soc Hypertens. 2018; 12:779–788.
Article27. Chou KJ, Lee PT, Chen CL, Chiou CW, Hsu CY, Chung HM, et al. Physiological changes during hemodialysis in patients with intradialysis hypertension. Kidney Int. 2006; 69:1833–1838.
Article28. Vervloet M, Cozzolino M. Vascular calcification in chronic kidney disease: different bricks in the wall? Kidney Int. 2017; 91:808–817.
Article29. Georgianos PI, Mpoutsiouki F, Sabani E, Stamatiadis DN, Liakopoulos V, Balaskas EV, et al. Hemodialysis patients with intradialytic rise in blood pressure display higher baseline aortic stiffness and negligible drop in augmentation index with dialysis. Int Urol Nephrol. 2016; 48:601–608.
Article30. Raikou VD, Kyriaki D. The association between intradialytic hypertension and metabolic disorders in end stage renal disease. Int J Hypertens. 2018; 2018:1681056.
Article31. Ravenel JG, Nance JW. Coronary artery calcification in lung cancer screening. Transl Lung Cancer Res. 2018; 7:361–367.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Cool Dialysate & Sodium Profiling on Hemodynamics in Patients with Intradialytic Hypotension
- Effect of Individual Low Sodium Dialysate on Blood Pressure, Interdialytic Weight Gain, Thirst and Intradialytic Discomfort In End-Stage Renal Disease Patients
- A Case of Metastatic Calcification Occurring at Sternoclavicular Joint in a Patient Receiving Maintenance Hemodialysis
- Effect of Pre- and Post-Dialysis Exercise on Functional Capacity Using Portable Ergometer in Chronic Kidney Disease Patients
- Nonocclusive mesenteric ischemia in a patient on maintenance hemodialysis