Cancer Res Treat.
2019 Jul;51(3):1041-1051. 10.4143/crt.2018.424.
Comparison of Breast Conserving Surgery Followed by Radiation Therapy with Mastectomy Alone for Pathologic N1 Breast Cancer Patients in the Era of Anthracycline Plus Taxane-Based Chemotherapy: A Multicenter Retrospective Study (KROG 1418)
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wonro.park@samsung.com
- 2Center for Breast Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 3Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. wonro. radiat@snu.ac.kr
- 4Department of Radiation Oncology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 5Department of Radiation Oncology, Kosin University Gospel Hospital, Busan, Korea.
- 6Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea.
- 7Department of Radiation Oncology, Chonnam National University Medical School, Gwangju, Korea.
- 8Department of Radiation Oncology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- 9Department of Radiation Oncology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 10Department of Radiation Oncology, Ajou University School of Medicine, Suwon, Korea.
- 11Department of Radiation Oncology, Dong-A University Hospital, Dong-A University School of Medicine, Busan, Korea.
- 12Department of Radiation Oncology, Chonbuk National University Medical School, Jeonju, Korea.
- 13Department of Radiation Oncology, Wonju Severance Christian Hospital, Wonju, Korea.
- KMID: 2454296
- DOI: http://doi.org/10.4143/crt.2018.424
Abstract
- PURPOSE
We compared the oncologic outcomes of breast-conserving surgery plus radiation therapy (BCS+RT) and modified radical mastectomy (MRM) under anthracycline plus taxane-based (AT) regimens and investigated the role of adjuvant radiation therapy (RT) in patients with pathologic N1 (pN1) breast cancer treated by mastectomy.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of 2,011 patients with pN1 breast cancer who underwent BCS+RT or MRM alone at 12 institutions between January 2006 and December 2010. Two-to-one propensity score matching was performed for balances in variables between the groups.
RESULTS
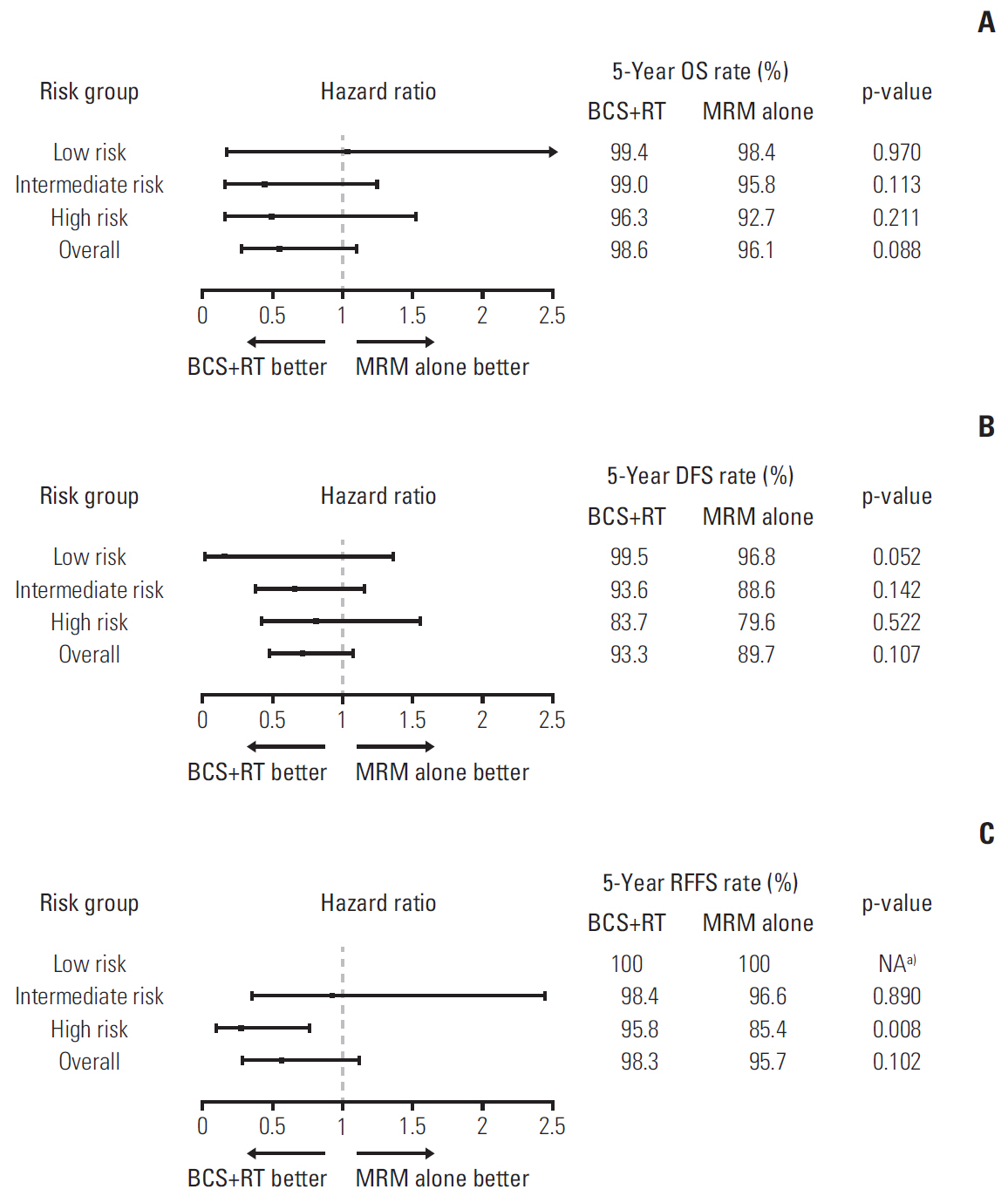
The median follow-up duration for the total cohort was 69 months (range, 1 to 114 months). After propensity score matching, 1,074 patients (676 in the BCS+RT group and 398 in the MRM-alone group) were analyzed finally. The overall survival, disease-free survival, locoregional failure-free survival, and regional failure-free survival (RFFS) curves of the BCS+RT group vs. MRM-alone group were not significantly different. The subgroup analysis revealed that in the group with both lymphovascular invasion (LVI) and histologic grade (HG) III, the BCS+RT showed significantly superior RFFS (p=0.008). Lymphedema (p=0.007) and radiation pneumonitis (p=0.031) occurred more frequently in the BCS+RT group than in the MRM-alone group, significantly.
CONCLUSION
There are no differences in oncologic outcomes between BCS+RT and MRM-alone groups under the AT chemotherapy regimens for pN1 breast cancer. However, BCS+RT group showed superior RFFS to MRM-alone group in the patients with LVI and HG III. Adjuvant RT might be considerable for pN1 breast cancer patients with LVI and HG III.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Arriagada R, Le MG, Rochard F, Contesso G. Conservative treatment versus mastectomy in early breast cancer: patterns of failure with 15 years of follow-up data. Institut Gustave-Roussy Breast Cancer Group. J Clin Oncol. 1996; 14:1558–64.
Article2. van Dongen JA, Voogd AC, Fentiman IS, Legrand C, Sylvester RJ, Tong D, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000; 92:1143–50.
Article3. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347:1227–32.
Article4. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–41.
Article5. Poggi MM, Danforth DN, Sciuto LC, Smith SL, Steinberg SM, Liewehr DJ, et al. Eighteen-year results in the treatment of early breast carcinoma with mastectomy versus breast conservation therapy: the National Cancer Institute Randomized Trial. Cancer. 2003; 98:697–702.6. Blichert-Toft M, Rose C, Andersen JA, Overgaard M, Axelsson CK, Andersen KW, et al. Danish randomized trial comparing breast conservation therapy with mastectomy: six years of life-table analysis. Danish Breast Cancer Cooperative Group. J Natl Cancer Inst Monogr. 1992; (11):19–25.7. Agarwal S, Pappas L, Neumayer L, Kokeny K, Agarwal J. Effect of breast conservation therapy vs mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg. 2014; 149:267–74.
Article8. Chen K, Liu J, Zhu L, Su F, Song E, Jacobs LK. Comparative effectiveness study of breast-conserving surgery and mastectomy in the general population: A NCDB analysis. Oncotarget. 2015; 6:40127–40.
Article9. Pyfer B, Chatterjee A, Chen L, Nigriny J, Czerniecki B, Tchou J, et al. Early postoperative outcomes in breast conservation surgery versus simple mastectomy with implant reconstruction: a NSQIP analysis of 11,645 patients. Ann Surg Oncol. 2016; 23:92–8.
Article10. Onitilo AA, Engel JM, Stankowski RV, Doi SA. Survival comparisons for breast conserving surgery and mastectomy revisited: community experience and the role of radiation therapy. Clin Med Res. 2015; 13:65–73.
Article11. van Maaren MC, de Munck L, de Bock GH, Jobsen JJ, van Dalen T, Linn SC, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol. 2016; 17:1158–70.
Article12. Ragaz J, Olivotto IA, Spinelli JJ, Phillips N, Jackson SM, Wilson KS, et al. Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst. 2005; 97:116–26.
Article13. Overgaard M, Nielsen HM, Overgaard J. Is the benefit of postmastectomy irradiation limited to patients with four or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG 82 b&c randomized trials. Radiother Oncol. 2007; 82:247–53.14. EBCTCG (Early Breast Cancer Trialists' Collaborative Group), McGale P, Taylor C, Correa C, Cutter D, Duane F, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014; 383:2127–35.15. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: breast cancer, version 2. Fort Washington, PA: National Comprehensive Cancer Network;2017.16. Mackey JR, Martin M, Pienkowski T, Rolski J, Guastalla JP, Sami A, et al. Adjuvant docetaxel, doxorubicin, and cyclophosphamide in node-positive breast cancer: 10-year follow-up of the phase 3 randomised BCIRG 001 trial. Lancet Oncol. 2013; 14:72–80.
Article17. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005; 365:1687–717.18. Early Breast Cancer Trialists' Collaborative Group (EBCTCG), Peto R, Davies C, Godwin J, Gray R, Pan HC, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012; 379:432–44.19. Verrill M. Chemotherapy for early-stage breast cancer: a brief history. Br J Cancer. 2009; 101 Suppl 1:S2–5.
Article20. Kim YJ, Park W, Ha B, Park B, Joo J, Kim TH, et al. Postmastectomy radiotherapy in patients with pT1-2N1 breast cancer treated with taxane-based chemotherapy: a retrospective multicenter analysis (KROG 1418). Cancer Res Treat. 2017; 49:927–36.
Article21. Kim J, Kim JH, Kim OB, Oh YK, Park SG. Clinical significance of the lymph node ratio in N1 breast cancer. Radiat Oncol J. 2017; 35:227–32.
Article22. Poortmans P, Aznar M, Bartelink H. Quality indicators for breast cancer: revisiting historical evidence in the context of technology changes. Semin Radiat Oncol. 2012; 22:29–39.
Article23. Hershman DL, Wright JD. Comparative effectiveness research in oncology methodology: observational data. J Clin Oncol. 2012; 30:4215–22.
Article24. Lai SF, Chen YH, Kuo WH, Lien HC, Wang MY, Lu YS, et al. Locoregional recurrence risk for postmastectomy breast cancer patients with T1-2 and one to three positive lymph nodes receiving modern systemic treatment without radiotherapy. Ann Surg Oncol. 2016; 23:3860–9.
Article25. Miyashita M, Tada H, Suzuki A, Watanabe G, Hirakawa H, Amari M, et al. Minimal impact of postmastectomy radiation therapy on locoregional recurrence for breast cancer patients with 1 to 3 positive lymph nodes in the modern treatment era. Surg Oncol. 2017; 26:163–70.
Article26. Yu JI, Park W, Choi DH, Huh SJ, Nam SJ, Kim SW, et al. Prognostic modeling in pathologic N1 breast cancer without elective nodal irradiation after current standard systemic management. Clin Breast Cancer. 2015; 15:e197–204.
Article27. Yu JI, Park W, Huh SJ, Choi DH, Lim YH, Ahn JS, et al. Determining which patients require irradiation of the supraclavicular nodal area after surgery for N1 breast cancer. Int J Radiat Oncol Biol Phys. 2010; 78:1135–41.
Article28. Ahn KJ, Park J, Choi Y. Lymphovascular invasion as a negative prognostic factor for triple-negative breast cancer after surgery. Radiat Oncol J. 2017; 35:332–9.
Article29. Cuzick J. Statistical controversies in clinical research: long-term follow-up of clinical trials in cancer. Ann Oncol. 2015; 26:2363–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Psychiatric Symptoms between Total Mastectomy and Breast Conserving Surgery in Breast Cancer Patients
- Breast-Conserving Surgery With or Without Radiation Therapy for Early Breast Cancer
- Treatment with Cisplatin and Etoposide Chemotherapy in Patient with Metastatic Breast Cancer
- Prognostic Impact of Elective Supraclavicular Nodal Irradiation for Patients with N1 Breast Cancer after Lumpectomy and Anthracycline Plus Taxane-Based Chemotherapy (KROG 1418): A Multicenter Case-Controlled Study
- Chemotherapy in Breast Cancer