Pediatr Infect Vaccine.
2019 Apr;26(1):71-79. 10.14776/piv.2019.26.e9.
A Child of Severe Mycoplasma pneumoniae pneumonia with Multiple Organ Failure Treated with ECMO and CRRT
- Affiliations
-
- 1Department of Pediatrics, Chungnam National University School of Medicine, Daejeon, the Republic of Korea. ehchung@cnu.ac.kr
- 2Department of Thoracic and Cardiovascular Surgery, Chungnam National University School of Medicine, Daejeon, the Republic of Korea.
- KMID: 2443168
- DOI: http://doi.org/10.14776/piv.2019.26.e9
Abstract
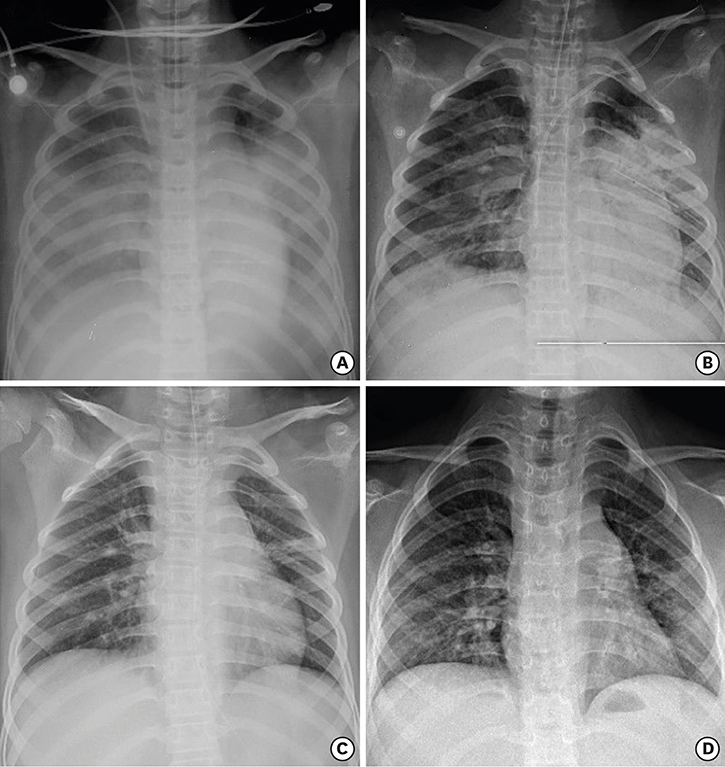
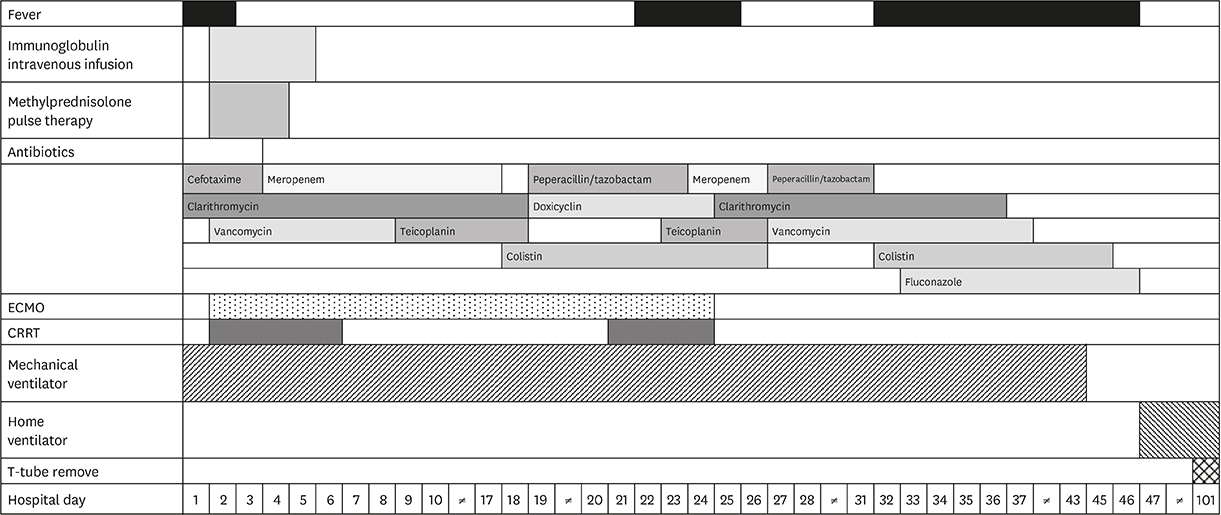
- Mycoplasma pneumoniae (MP) is the most common causative agent of community-acquired pneumonia in school-aged children. An 8-year-old boy who had been diagnosed with autism looked severely ill when he presented to our hospital due to dyspnea and lethargy. He had fever and cough 7 days prior to hospitalization. He had signs and symptoms of severe respiratory distress. The percutaneous oxygen saturation was 88% at high oxygen supply. Chest radiography showed diffusely increased opacity with moderate pleural effusion. He was intubated immediately and admitted to the intensive care unit. Under the clinical impression of mycoplasmal pneumonia, intravenous clarithromycin was started. Laboratory findings showed leukocytosis, hepatitis, decreased renal function, and presence of serum MP immunoglobulin (Ig) M (+) IgG (+) and sputum MP polymerase chain reaction (+). On hospital day 2, the patient developed multiple organ failure with acute respiratory distress syndrome (ARDS). Veno-venous extracorporeal membrane oxygenation (ECMO) was performed with continuous renal replacement therapy (CRRT) and was weaned successfully. This is the first reported case of an ARDS due to MP infection complicated by multiple organ failure that was successfully treated with ECMO and CRRT in South Korea.
Keyword
MeSH Terms
-
Autistic Disorder
Child*
Clarithromycin
Cough
Dyspnea
Extracorporeal Membrane Oxygenation*
Fever
Hepatitis
Hospitalization
Humans
Immunoglobulin G
Immunoglobulins
Intensive Care Units
Korea
Lethargy
Leukocytosis
Male
Multiple Organ Failure*
Mycoplasma pneumoniae*
Mycoplasma*
Oxygen
Pleural Effusion
Pneumonia*
Pneumonia, Mycoplasma*
Polymerase Chain Reaction
Radiography
Renal Replacement Therapy
Respiratory Distress Syndrome, Adult
Sputum
Thorax
Clarithromycin
Immunoglobulin G
Immunoglobulins
Oxygen
Figure
Reference
-
1. Garo B, Garré M, Quiot JJ, Boles JM, Becq-Giraudon B, Chennebault JM, et al. Mycoplasma pneumoniae infections. A multicenter retrospective study of 182 cases. Presse Med. 1988; 17:1475–1478.2. Marrie TJ. Mycoplasma pneumoniae pneumonia requiring hospitalization, with emphasis on infection in the elderly. Arch Intern Med. 1993; 153:488–494.
Article3. Yoshida T, Asato Y, Kukita I, Ooshiro M, Takara I, Iha H, et al. A 7-year-old boy with mycoplasmal infection requiring extracorporeal membrane oxygenation. Eur J Pediatr. 2003; 162:44–46.
Article4. Van Bever HP, Van Doorn JW, Demey HE. Adult respiratory distress syndrome associated with Mycoplasma pneumoniae infection. Eur J Pediatr. 1992; 151:227–228.
Article5. Kwon JE, Ahn KY, Choi BS. Two patients with Mycoplasma pneumoniae pneumonia progressing to acute respiratory distress syndrome. Allergy Asthma Respir Dis. 2017; 5:169–174.
Article6. Park SJ, Pai KS, Kim AR, Lee JH, Shin JI, Lee SY. Fulminant and fatal multiple organ failure in a 12-year-old boy with Mycoplasma pneumoniae infection. Allergy Asthma Immunol Res. 2012; 4:55–57.
Article7. Koletsky RJ, Weinstein AJ. Fulminant Mycoplasma pneumoniae infection. Report of a fatal case, and a review of the literature. Am Rev Respir Dis. 1980; 122:491–496.8. Chan ED, Welsh CH. Fulminant Mycoplasma pneumoniae pneumonia. West J Med. 1995; 162:133–142.9. Miyashita N, Obase Y, Ouchi K, Kawasaki K, Kawai Y, Kobashi Y, et al. Clinical features of severe Mycoplasma pneumoniae pneumonia in adults admitted to an intensive care unit. J Med Microbiol. 2007; 56:1625–1629.
Article10. Noriega ER, Simberkoff MS, Gilroy FJ, Rahal JJ Jr. Life-threatening Mycoplasma pneumoniae pneumonia. JAMA. 1974; 229:1471–1472.11. Izumikawa K, Izumikawa K, Takazono T, Kosai K, Morinaga Y, Nakamura S, et al. Clinical features, risk factors and treatment of fulminant Mycoplasma pneumoniae pneumonia: a review of the Japanese literature. J Infect Chemother. 2014; 20:181–185.
Article12. Chung EH. Serological diagnosis of Mycoplasma pneumoniae infections. Korean J Pediatr Infect Dis. 2006; 13:21–30.
Article13. Radisic M, Torn A, Gutierrez P, Defranchi HA, Pardo P. Severe acute lung injury caused by Mycoplasma pneumoniae: potential role for steroid pulses in treatment. Clin Infect Dis. 2000; 31:1507–1511.
Article14. Lee KY, Lee HS, Hong JH, Lee MH, Lee JS, Burgner D, et al. Role of prednisolone treatment in severe Mycoplasma pneumoniae pneumonia in children. Pediatr Pulmonol. 2006; 41:263–268.
Article15. Tagliabue C, Salvatore CM, Techasaensiri C, Mejias A, Torres JP, Katz K, et al. The impact of steroids given with macrolide therapy on experimental Mycoplasma pneumoniae respiratory infection. J Infect Dis. 2008; 198:1180–1188.
Article16. Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1998; 280:159–165.
Article17. Priestley MA, Helfaer MA. Approaches in the management of acute respiratory failure in children. Curr Opin Pediatr. 2004; 16:293–298.
Article18. Meuers KV, Lally KP, Peek G, Zwischenberger JB. ECMO: extracorporeal cardiopulmonary support in critical care. 3rd ed. Ann Arbor, Michigan: Extracorporeal Life Support Organization;2005.19. Green TP, Timmons OD, Fackler JC, Moler FW, Thompson AE, Sweeney MF. The impact of extracorporeal membrane oxygenation on survival in pediatric patients with acute respiratory failure. Pediatric Critical Care Study Group. Crit Care Med. 1996; 24:323–329.
Article20. Park JM. Continuous renal replacement therapy in children. J Korean Soc Pediatr Nephrol. 2009; 13:118–129.
Article21. Paden ML, Warshaw BL, Heard ML, Fortenberry JD. Recovery of renal function and survival after continuous renal replacement therapy during extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2011; 12:153–158.
Article22. Mansel JK, Rosenow EC 3rd, Smith TF, Martin JW Jr. Mycoplasma pneumoniae pneumonia. Chest. 1989; 95:639–646.23. Kim CK, Chung CY, Kim JS, Kim WS, Park Y, Koh YY. Late abnormal findings on high-resolution computed tomography after Mycoplasma pneumonia. Pediatrics. 2000; 105:372–378.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycoplasma pneumoniae Pneumonia with a Fulminant Course in a Previously Healthy Boy
- Mycoplasma pneumoniae Pneumonia in Children
- Clinical Observation on Pneumonia due to Mycoplasma Pneumoniae in Children
- Study of mixed infection with mycoplasma pneumoniae and adenovirus in hospitalized children with pneumonia
- A clinical study of mycoplasma pneumonia in children during recent 5 years