J Korean Orthop Assoc.
2019 Feb;54(1):24-29. 10.4055/jkoa.2019.54.1.24.
Early Onset Subsequent Vertebral Compression Fracture after Percutaneous Verteroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Presbyterian Medical Center, Jeonju, Korea. docby@hanmail.net
- KMID: 2438954
- DOI: http://doi.org/10.4055/jkoa.2019.54.1.24
Abstract
- PURPOSE
To evaluate the characteristics and the risk factors of early onset subsequent vertebral compression fractures after percutaneous vertebroplasty.
MATERIALS AND METHODS
A total of 44 patients, who had a new subsequent vertebral fracture after percutaneous vertebroplasty for an osteoporotic vertebral compression fracture between January 2013 and December 2015, were recruited. The patients were divided into two groups according to the onset period of subsequent fracture. The number of patients who had a fracture within 3 months following vertebroplasty were 22 cases (Group A); after 3 months were 22 cases (Group B). Variables, including age, sex, bone mineral density (BMD), body mass index (BMI), preexisting vertebral compression fracture, location of the initial fracture, intradiscal cement leakage, injected cement volume, restoration of vertebral body height, and correction of kyphosis, in the two groups were analyzed and compared retrospectively.
RESULTS
The age, sex, BMD, BMI, preexisting vertebral compression fracture, location of the initial fracture, intradiscal cement leakage, and correction of kyphosis were similar in the two groups. Both a greater volume of bone cement injected and a greater degree of vertebral height restoration contributed significantly to the risk of fracture within 3 months.
CONCLUSION
The cement volume and degree of height restoration are risk factors for early onset fracture at the adjacent vertebrae after percutaneous vertebroplasty and close attention is needed during the follow-up period.
MeSH Terms
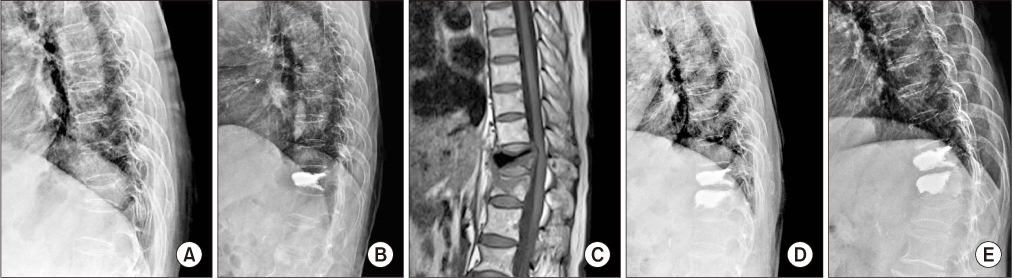
Figure
Reference
-
1. Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003; 226:119–124.
Article2. Kim CH, Hwang JK, Park JS. Adjacent vertebral compression fracture after percutaneous vertebroplasty. J Korean Soc Spine Surg. 2013; 20:163–168.
Article3. Tseng YY, Yang TC, Tu PH, Lo YL, Yang ST. Repeated and multiple new vertebral compression fractures after percutaneous transpedicular vertebroplasty. Spine (Phila Pa 1976). 2009; 34:1917–1922.
Article4. Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001; 285:320–323.
Article5. Kim SS, Lee DH, Kim JH, et al. Risk factors for subsequent vertebral compression fracture following osteoporotic compression fracture. J Korean Orthop Assoc. 2016; 51:479–485.
Article6. Cyteval C, Sarrabère MP, Roux JO, et al. Acute osteoporotic vertebral collapse: open study on percutaneous injection of acrylic surgical cement in 20 patients. AJR Am J Roentgenol. 1999; 173:1685–1690.
Article7. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000; 15:721–739.
Article8. Kim SH, Kang HS, Choi JA, Ahn JM. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol. 2004; 45:440–445.
Article9. Li YA, Lin CL, Chang MC, Liu CL, Chen TH, Lai SC. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine (Phila Pa 1976). 2012; 37:179–183.10. Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002; 96:S56–S61.
Article11. Hodler J, Peck D, Gilula LA. Midterm outcome after vertebroplasty: predictive value of technical and patient-related factors. Radiology. 2003; 227:662–668.
Article12. Kaufmann TJ, Trout AT, Kallmes DF. The effects of cement volume on clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2006; 27:1933–1937.13. Kang SK, Lee CW, Park NK, et al. Predictive risk factors for refracture after percutaneous vertebroplasty. Ann Rehabil Med. 2011; 35:844–851.
Article14. Kim MH, Lee AS, Min SH, Yoon SH. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Asian Spine J. 2011; 5:180–187.
Article15. Lin WC, Cheng TT, Lee YC, et al. New vertebral osteoporotic compression fractures after percutaneous vertebroplasty: retrospective analysis of risk factors. J Vasc Interv Radiol. 2008; 19:225–231.
Article16. Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004; 25:175–180.17. Pitton MB, Herber S, Bletz C, et al. CT-guided vertebroplasty in osteoprotic vertebral fractures: incidence of secondary fractures and impact of intradiscal cement leakages during follow-up. Eur Radiol. 2008; 18:43–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors for Subsequent Fracture after Osteoporotic Vertebral Compression Fracture
- The Proper Volume and Distribution of Cement Augmentation on Percutaneous Vertebroplasty
- Cement Leakage into Disc after Kyphoplasty: Does It Increases the Risk of New Adjacent Vertebral Fractures?
- Adjacent Vertebral Compression Fracture after Percutaneous Vertebroplasty
- Subsequent Vertebral Fracture after Percutaneous Vertebral Augmentation: Adjacent and Non-adjacent Vertebral Fractures