Korean J Radiol.
2019 Feb;20(2):275-282. 10.3348/kjr.2018.0300.
Evaluation of Tumor Blood Flow Using Alternate Ascending/Descending Directional Navigation in Primary Brain Tumors: A Comparison Study with Dynamic Susceptibility Contrast Magnetic Resonance Imaging
- Affiliations
-
- 1Department of Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 2Magnetic Resonance Imaging Laboratory, Department of Bio and Brain Engineering, Korea Advanced Institute of Science and Technology, Daejeon, Korea.
- 3Department of Radiology, Seoul National University Hospital, Seoul, Korea. verocay@snuh.org
- 4Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 5Center for Nanoparticle Research, Institute for Basic Science (IBS), Seoul, Korea.
- KMID: 2438258
- DOI: http://doi.org/10.3348/kjr.2018.0300
Abstract
OBJECTIVE
Alternate ascending/descending directional navigation (ALADDIN) is a novel arterial spin labeling technique that does not require a separate spin preparation pulse. We sought to compare the normalized cerebral blood flow (nCBF) values obtained by ALADDIN and dynamic susceptibility contrast (DSC) perfusion magnetic resonance imaging (MRI) in patients with primary brain tumors.
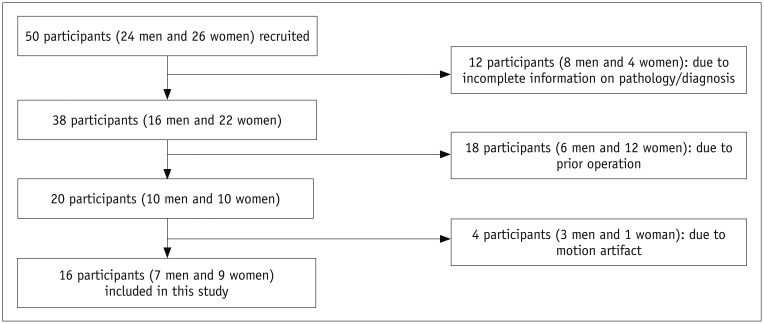
MATERIALS AND METHODS
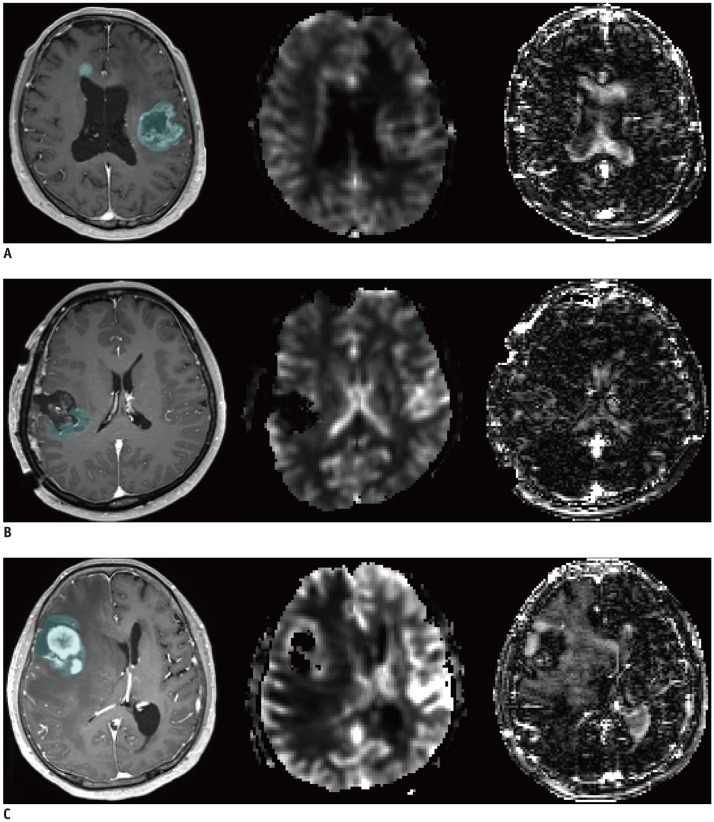
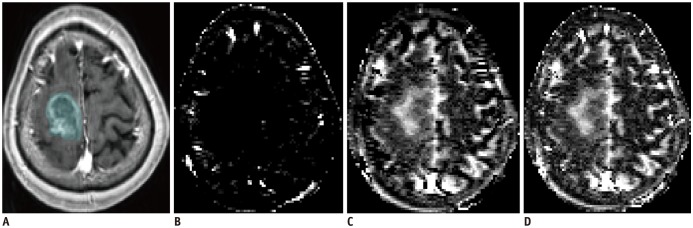
Sixteen patients with primary brain tumors underwent MRI scans including contrast-enhanced T1-weighted imaging, DSC perfusion MRI, and ALADDIN. The nCBF values of normal gray matter (GM) and tumor areas were measured by both DSC perfusion MRI and ALADDIN, which were compared by the Wilcoxon signed rank test. Subgroup analyses according to pathology were performed with the Wilcoxon signed rank test.
RESULTS
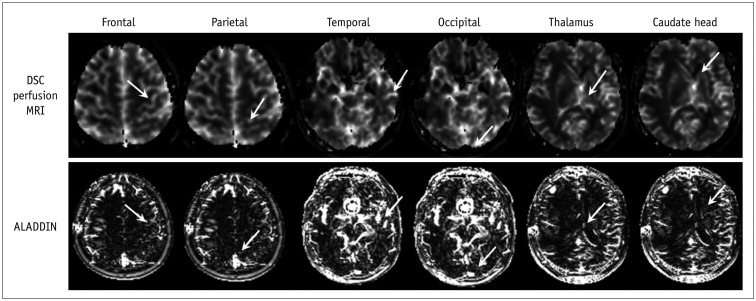
Higher mean nCBF values of GM regions in the bilateral frontal lobe, temporal lobe, and caudate were detected by ALADDIN than by DSC perfusion MRI (p <0.05). In terms of the mean or median nCBF values and the mean of the top 10% nCBF values from tumors, DSC perfusion MRI and ALADDIN did not statistically significantly differ either overall or in each tumor group.
CONCLUSION
ALADDIN tended to detect higher nCBF values in normal GM, as well as higher perfusion portions of primary brain tumors, than did DSC perfusion MRI. We believe that the high perfusion signal on ALADDIN can be beneficial in lesion detection and characterization.
Keyword
MeSH Terms
Figure
Reference
-
1. Jahng GH, Li KL, Ostergaard L, Calamante F. Perfusion magnetic resonance imaging: a comprehensive update on principles and techniques. Korean J Radiol. 2014; 15:554–577. PMID: 25246817.
Article2. Järnum H, Steffensen EG, Knutsson L, Fründ ET, Simonsen CW, Lundbye-Christensen S, et al. Perfusion MRI of brain tumours: a comparative study of pseudo-continuous arterial spin labelling and dynamic susceptibility contrast imaging. Neuroradiology. 2010; 52:307–317. PMID: 19841916.
Article3. Cha S. Perfusion MR imaging: basic principles and clinical applications. Magn Reson Imaging Clin N Am. 2003; 11:403–413. PMID: 14768726.
Article4. Lee EK, Choi SH, Yun TJ, Kang KM, Kim TM, Lee SH, et al. Prediction of response to concurrent chemoradiotherapy with temozolomide in glioblastoma: application of immediate post-operative dynamic susceptibility contrast and diffusion-weighted MR imaging. Korean J Radiol. 2015; 16:1341–1348. PMID: 26576125.
Article5. Petcharunpaisan S, Ramalho J, Castillo M. Arterial spin labeling in neuroimaging. World J Radiol. 2010; 2:384–398. PMID: 21161024.
Article6. Wong AM, Yan FX, Liu HL. Comparison of three-dimensional pseudo-continuous arterial spin labeling perfusion imaging with gradient-echo and spin-echo dynamic susceptibility contrast MRI. J Magn Reson Imaging. 2014; 39:427–433. PMID: 23677620.
Article7. Rogosnitzky M, Branch S. Gadolinium-based contrast agent toxicity: a review of known and proposed mechanisms. Biometals. 2016; 29:365–376. PMID: 27053146.
Article8. Park SH, Duong TQ. Brain MR perfusion-weighted imaging with alternate ascending/descending directional navigation. Magn Reson Med. 2011; 65:1578–1591. PMID: 20860002.
Article9. Park SH, Han PK, Choi SH. Physiological and functional magnetic resonance imaging using balanced steady-state free precession. Korean J Radiol. 2015; 16:550–559. PMID: 25995684.
Article10. Park SH, Do WJ, Choi SH, Zhao T, Bae KT. Mapping blood flow directionality in the human brain. Magn Reson Imaging. 2016; 34:754–764. PMID: 26968145.
Article11. Kim KH, Choi SH, Park SH. Feasibility of quantifying arterial cerebral blood volume using multiphase alternate ascending/descending directional navigation (ALADDIN). PLoS One. 2016; 11:e0156687. PMID: 27257674.
Article12. Han PK, Choi SH, Park SH. Investigation of control scans in pseudo-continuous arterial spin labeling (pCASL): strategies for improving sensitivity and reliability of pCASL. Magn Reson Med. 2017; 78:917–929. PMID: 27690322.
Article13. Han PK, Barker JW, Kim KH, Choi SH, Bae KT, Park SH. Inter-slice blood flow and magnetization transfer effects as a new simultaneous imaging strategy. PLoS One. 2015; 10:e0140560. PMID: 26466316.
Article14. Rosen BR, Belliveau JW, Vevea JM, Brady TJ. Perfusion imaging with NMR contrast agents. Magn Reson Med. 1990; 14:249–265. PMID: 2345506.
Article15. Ostergaard L, Weisskoff RM, Chesler DA, Gyldensted C, Rosen BR. High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part I: mathematical approach and statistical analysis. Magn Reson Med. 1996; 36:715–772. PMID: 8916022.16. Boxerman JL, Schmainda KM, Weisskoff RM. Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol. 2006; 27:859–867. PMID: 16611779.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Study of Dynamic Susceptibility Contrast Perfusion MR Images between Warthin's Tumor and Malignant Parotid Tumors
- Advanced Magnetic Resonance Imaging for Pediatric Brain Tumors: Current Imaging Techniques and Interpretation Algorithms
- Blood Volume of Intraaxial Brain Tumor: Evaluation with Dynamic Contrast-Enhanced T2*-Weighted MR Imaging
- Assessment of Non-permeability of Gd-DTPA for Dynamic Susceptibility Contrast in Human Brain: A Preliminary Study Using Non-linear Curve Fitting
- Advances in magnetic resonance technique for tumor imaging