Increased Prevalence of Thalassemia in Young People in Korea: Impact of Increasing Immigration
- Affiliations
-
- 1Department of Laboratory Medicine, Pusan National University School of Medicine, Busan, Korea. hhkim@pusan.ac.kr
- 2Department of BioMedical Informatics Unit, Pusan National University School of Medicine, Busan, Korea.
- 3Department of Pediatrics, Pusan National University School of Medicine, Busan, Korea.
- 4Division of Human Blood Safety Surveillance, Korea Centers for Disease Control and Prevention, Cheongju, Korea.
- 5Division of Infectious Disease Surveillance, Korea Centers for Disease Control and Prevention, Cheongju, Korea.
- 6Division of Laboratory Diagnosis Management, Korea Centers for Disease Control and Prevention, Cheongju, Korea.
- 7Department of Laboratory Medicine, Chonnam National University Medical School, Gwangju, Korea.
- 8Department of Laboratory Medicine, Chonbuk National University Hospital, Jeonju, Korea.
- 9Department of Pediatrics, Chonbuk National University Hospital, Jeonju, Korea.
- 10Department of Laboratory Medicine, Dong-A University College of Medicine, Busan, Korea.
- 11Department of Laboratory Medicine, Kosin University College of Medicine, Busan, Korea.
- 12Department of Pediatrics, Kosin University College of Medicine, Busan, Korea.
- 13Department of Pediatrics, Busan St. Mary Hospital, Busan, Korea.
- 14Department of Laboratory Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2425968
- DOI: http://doi.org/10.3343/alm.2019.39.2.133
Abstract
- BACKGROUND
Thalassemia is highly prevalent in Southeast Asia but is rare in Korea; however, Southeast Asian immigrant population is recently rising in Korea. We investigated the prevalence of thalassemia in Korea in the context of increasing immigration.
METHODS
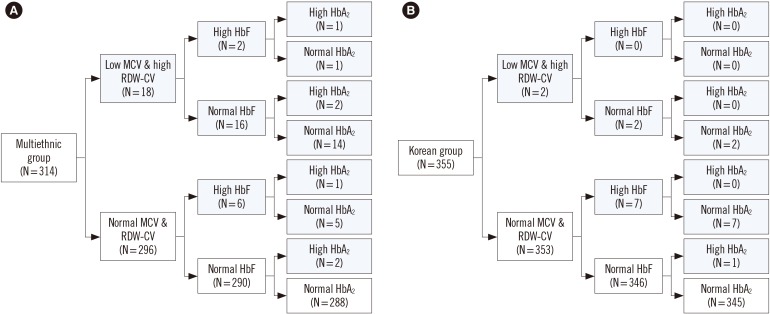
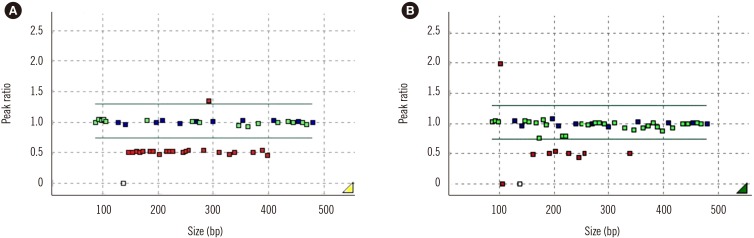
This prospective, observational, multicenter study was conducted between September 2015 and August 2017. A total of 669 subjects < 30 years living in Korea were grouped into the multiethnic (N=314) and Korean (N=355) groups. Hb electrophoresis and complete blood count (CBC) were performed. If low mean corpuscular volume with high red blood cell distribution width coefficient of variation or a high fetal Hb (HbF) or Hb alpha 2 (HbA2) level was observed, genetic testing of the α- and β-globin genes was performed. In addition, the number of potential thalassemia carriers in Korea was estimated by multiplying the prevalence of thalassemia in a specific ethnicity by the number of immigrants of that ethnicity.
RESULTS
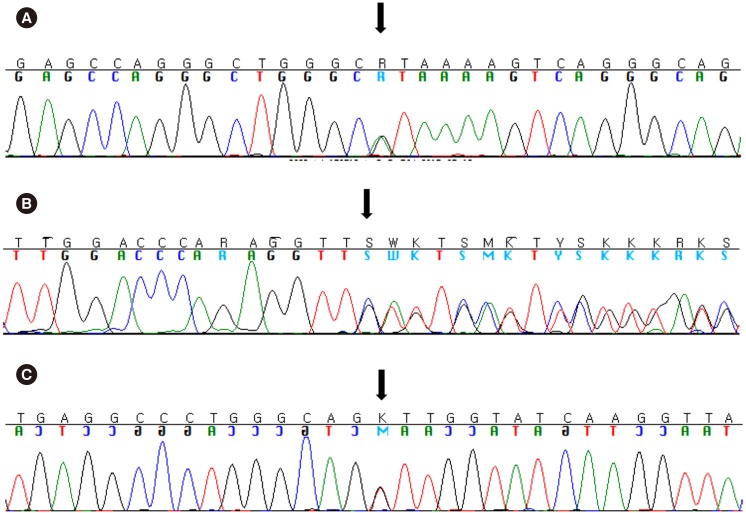
Twenty-six multiethnic and 10 Korean subjects showed abnormal results for Hb electrophoresis and CBC. Eighteen multiethnic subjects and four Korean subjects were tested for α-globin and β-globin gene mutations. Within the multiethnic group, five subjects (1.5%) were α-thalassemia carriers, and six (1.9%) were β-thalassemia minor. The SEA deletion in HBA1 and HBA2, and c. 126_129delCTTT (p.Phe42Leufs*19) mutation of HBB were the dominant inherited mutations.
CONCLUSIONS
The prevalence of thalassemia in young people in Korea is increasing due to the increasing number of Southeast Asian immigrants.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Epidemiological Study of Hereditary Hemolytic Anemia in the Korean Pediatric Population during 1997–2016: a Nationwide Retrospective Cohort Study
Ye Jee Shim, Hye Lim Jung, Hee Young Shin, Hyoung Jin Kang, Jung Yoon Choi, Jeong Ok Hah, Jae Min Lee, Young Tak Lim, Eu Jeen Yang, Hee Jo Baek, Hyoung Soo Choi, Keon Hee Yoo, Jun Eun Park, Seongkoo Kim, Ji Yoon Kim, Eun Sil Park, Ho Joon Im, Hee Won Chueh, Soon Ki Kim, Jae Hee Lee, Eun Sun Yoo, Hyeon Jin Park, Jun Ah Lee, Meerim Park, Hyun Sik Kang, Ji Kyoung Park, Na Hee Lee, Sang Kyu Park, Young-Ho Lee, Seong Wook Lee, Eun Jin Choi, Seom Gim Kong,
J Korean Med Sci. 2020;35(33):e279. doi: 10.3346/jkms.2020.35.e279.Korean clinical practice guidelines for the diagnosis of hereditary hemolytic anemia
Hee Won Chueh, Sang Mee Hwang, Ye Jee Shim, Jae Min Lee, Hee Sue Park, Joon Hee Lee, Youngwon Nam, Namhee Kim, Hye Lim Jung, Hyoung Soo Choi, on behalf of Korean RBC Disorder Working Party
Blood Res. 2022;57(2):86-94. doi: 10.5045/br.2022.2021224.Beta Thalassemia Presenting with Neonatal Cholestasis and Extensive Hemosiderosis: A Case Report
Chung Gang Jung, Jang Hoon Lee, Yu Bin Kim
Neonatal Med. 2023;30(4):102-107. doi: 10.5385/nm.2023.30.4.102.
Reference
-
1. Li CK. New trend in the epidemiology of thalassaemia. Best Pract Res Clin Obstet Gynaecol. 2017; 39:16–26. PMID: 27847257.2. De Sanctis V, Kattamis C, Canatan D, Soliman AT, Elsedfy H, Karimi M, et al. β-Thalassemia distribution in the Old World: an ancient disease seen from a historical standpoint. Mediterr J Hematol Infect Dis. 2017; 9:e2017018. PMID: 28293406.3. Hossain MS, Raheem E, Sultana TA, Ferdous S, Nahar N, Islam S, et al. Thalassemias in South Asia: clinical lessons learnt from Bangladesh. Orphanet J Rare Dis. 2017; 12:93. PMID: 28521805.4. Lai K, Huang G, Su L, He Y. The prevalence of thalassemia in mainland China: evidence from epidemiological surveys. Sci Rep. 2017; 7:920. PMID: 28424478.5. Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008; 86:480–487. PMID: 18568278.6. Park ES, Jung HL, Kim HJ, Park SS, Bae SH, Shin HY, et al. Hereditary hemolytic anemia in Korea from 2007 to 2011: a study by the Korean Hereditary Hemolytic Anemia Working Party of the Korean Society of Hematology. Blood Res. 2013; 48:211–216. PMID: 24086942.7. Korean Ministry of Justice. Statistical yearbook of foreign policy on immigration in 2017. Updated on Jun 2018. http://www.moj.go.kr.8. Mosca A, Paleari R, Leone D, Ivaldi G. The relevance of hemoglobin F measurement in the diagnosis of thalassemias and related hemoglobinopathies. Clin Biochem. 2009; 42:1797–1801. PMID: 19580798.9. Patrinos GP, Giardine B, Riemer C, Miller W, Chui DH, Anagnou NP, et al. Improvements in the HbVar database of human hemoglobin variants and thalassemia mutations for population and sequence variation studies. Nucleic Acids Res. 2004; 32:D537–D541. PMID: 14681476.10. O’Riordan S, Hien TT, Miles K, Allen A, Quyen NN, Hung NQ, et al. Large scale screening for haemoglobin disorders in southern Vietnam: implications for avoidance and management. Br J Haematol. 2010; 150:359–364. PMID: 20497177.11. Nuinoon M, Kruachan K, Sengking W, Horpet D, Sungyuan U. Thalassemia and hemoglobin E in Southern Thai blood donors. Adv Hematol. 2014; 2014:932306. PMID: 25050123.12. Kohne E. Hemoglobinopathies: clinical manifestations, diagnosis, and treatment. Dtsch Arztebl Int. 2011; 108:532–540. PMID: 21886666.13. Sayani FA, Kwiatkowski JL. Increasing prevalence of thalassemia in America: implications for primary care. Ann Med. 2015; 47:592–604. PMID: 26541064.14. Mettananda S, Higgs DR. Molecular basis and genetic modifiers of thalassemia. Hematol Oncol Clin North Am. 2018; 32:177–191. PMID: 29458725.15. Lithanatudom P, Khampan P, Smith DR, Svasti S, Fucharoen S, Kangwanpong D, et al. The prevalence of alpha-thalassemia amongst Tai and Mon-Khmer ethnic groups residing in northern Thailand: a population-based study. Hematology. 2016; 21:480–485. PMID: 27077764.16. Yamashiro Y, Hattori Y. Hemoglobinopathies in Japan: characteristics and comparison with those of other ethnic groups. Rinsho Ketsueki. 2015; 56:752–759. PMID: 26251137.17. Hong CR, Kang HJ, Lee JW, Kim H, Kim NH, Park KD, et al. Clinical characteristics of pediatric thalassemia in Korea: a single institute experience. J Korean Med Sci. 2013; 28:1645–1649. PMID: 24265529.18. Torcharus K, Sriphaisal T, Krutvecho T, Ketupanya A, Vuthiwong C, Suwanasophon C, et al. Prenatal diagnosis of Hb Bart’s hydrops fetalis by PCR technique: Pramongkutklao experience. Southeast Asian J Trop Med Public Health. 1995; 26 Suppl 1:287–290. PMID: 8629126.19. Filon D, Oppenheim A, Rachmilewitz EA, Kot R, Truc DB. Molecular analysis of beta-thalassemia in Vietnam. Hemoglobin. 2000; 24:99–104. PMID: 10870880.20. Svasti S, Hieu TM, Munkongdee T, Winichagoon P, Van Be T, Van Binh T, et al. Molecular analysis of beta-thalassemia in South Vietnam. Am J Hematol. 2002; 71:85–88. PMID: 12353305.21. Huang H, Xu L, Lin N, He D, Li Y, Guo D, et al. Molecular spectrum of β-thalassemia in Fujian Province, Southeastern China. Hemoglobin. 2013; 37:343–350. PMID: 23682686.22. Yu X, Yang LY, Yang HT, Liu CG, Cao DC, Shen W, et al. Molecular epidemiological investigation of thalassemia in the Chengdu region, Sichuan Province, southwest China. Hemoglobin. 2015; 39:393–397. PMID: 26290351.23. Boonyawat B, Monsereenusorn C, Traivaree C. Molecular analysis of beta-globin gene mutations among Thai beta-thalassemia children: results from a single center study. Appl Clin Genet. 2014; 7:253–258. PMID: 25525381.24. Park SS. Beta-thalassemia in the Korean population. Int J Hematol. 2002; 76 Suppl 2:93–95. PMID: 12430907.25. Origa R. Beta-thalassemia. Updated on Jan 2018. https://www.ncbi.nlm.nih.gov/books/NBK1426/.26. Origa R, Moi P. Alpha-thalassemia. Updated on Dec 2016. https://www.ncbi.nlm.nih.gov/books/NBK1435/.27. Angelucci E, Matthes-Martin S, Baronciani D, Bernaudin F, Bonanomi S, Cappellini MD, et al. Hematopoietic stem cell transplantation in thalassemia major and sickle cell disease: indications and management recommendations from an international expert panel. Haematologica. 2014; 99:811–820. PMID: 24790059.28. Algiraigri AH, Wright NAM, Paolucci EO, Kassam A. Hydroxyurea for nontransfusion-dependent β-thalassemia: a systematic review and meta-analysis. Hematol Oncol Stem Cell Ther. 2017; 10:116–125. PMID: 28408107.29. Srivastava A, Shaji RV. Cure for thalassemia major–from allogeneic hematopoietic stem cell transplantation to gene therapy. Haematologica. 2017; 102:214–223. PMID: 27909215.30. Ferrari G, Cavazzana M, Mavilio F. Gene therapy approaches to hemoglobinopathies. Hematol Oncol Clin North Am. 2017; 31:835–852. PMID: 28895851.31. de Dreuzy E, Bhukhai K, Leboulch P, Payen E. Current and future alternative therapies for beta-thalassemia major. Biomed J. 2016; 39:24–38. PMID: 27105596.32. Rachmilewitz EA. How I treat thalassemia. Blood. 2011; 118:3479–3488. PMID: 21813448.33. Neufeld EJ. Oral chelators deferasirox and deferiprone for transfusional iron overload in thalassemia major: new data, new questions. Blood. 2006; 107:3436–3441. PMID: 16627763.34. Quinn CT, St Pierre TG. MRI measurements of iron load in transfusion-dependent patients: implementation, challenges, and pitfalls. Pediatr Blood Cancer. 2016; 63:773–780. PMID: 26713769.35. Lee HJ, Shin KH, Kim HH, Kim MJ, Kim JN. A survey of the opinions of transfusion specialists on transfusion policy of thalassemia patients in Korea. Korean J Blood Transfus. 2017; 28:282–289.36. Humphreys JV. The management of sickle cell disease in a primary care setting. J Family Med Prim Care. 2012; 1:56–58. PMID: 24479003.37. Cunningham MJ. Update on thalassemia: clinical care and complications. Pediatr Clin North Am. 2008; 55:447–460. PMID: 18381095.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Altitude, Immigration and Suicide Rates: A Study from Turkey
- The Effect of ABO Blood Groups, Hemoglobinopathy, and Heme Oxygenase-1 Polymorphisms on Malaria Susceptibility and Severity
- Molecular basis and diagnosis of thalassemia
- Coexistence of Malaria and Thalassemia in Malaria Endemic Areas of Thailand
- A Survey of the Opinions of Transfusion Specialists on Transfusion Policy of Thalassemia Patients in Korea