J Pathol Transl Med.
2018 Jul;52(4):211-218. 10.4132/jptm.2018.04.27.
Pulmonary Nodular Lymphoid Hyperplasia with Mass-Formation: Clinicopathologic Characteristics of Nine Cases and Review of the Literature
- Affiliations
-
- 1Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hanjho@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2417804
- DOI: http://doi.org/10.4132/jptm.2018.04.27
Abstract
- BACKGROUND
Pulmonary nodular lymphoid hyperplasia (PNLH) is a non-neoplastic pulmonary lymphoid disorder that can be mistaken for malignancy on radiography. Herein, we present nine cases of PNLH, emphasizing clinicoradiological findings and histological features.
METHODS
We analyzed radiological and clinicopathological features from the electronic medical records of nine patients (eight females and one male) diagnosed with PNLH. IgG and IgG4 immunohistochemical staining was performed in three patients.
RESULTS
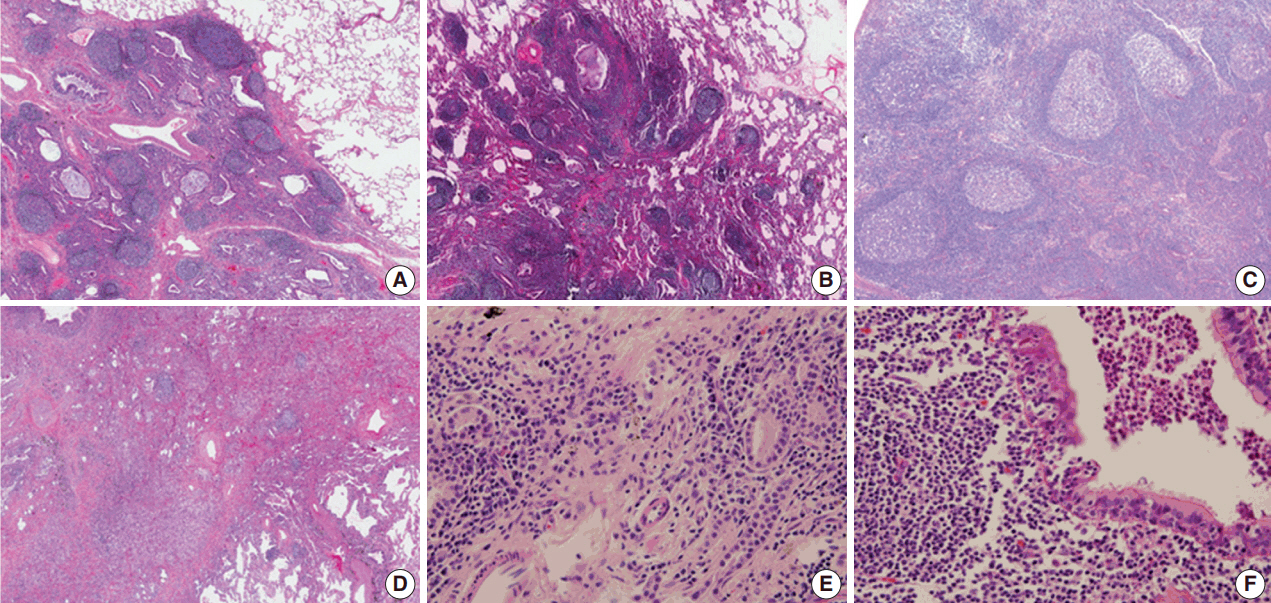
Two of the nine patients had experienced tuberculosis 40 and 30 years prior, respectively. Interestingly, none were current smokers, although two were ex-smokers. Three patients complaining of persistent cough underwent computed tomography of the chest. PNLH was incidentally discovered in five patients during examination for other reasons. The remaining patient was diagnosed with the disease following treatment for pneumonia. Imaging studies revealed consolidation or a mass-like lesion in eight patients. First impressions included invasive adenocarcinoma and mucosal-associated lymphoid tissue"’type lymphoma. Aspergillosis was suspected in the remaining patient based on radiological images. Resection was performed in all patients. Microscopically, the lesions consisted of nodular proliferation of reactive germinal centers accompanied by infiltration of neutrophils and macrophages in various degrees and surrounding fibrosis. Ultimately, all nine patients were diagnosed with PNLH and showed no evidence of recurrence on follow-up.
CONCLUSIONS
PNLH is an uncommon but distinct entity with a benign nature, and understanding the radiological and clinicopathological characteristics of PNLH is important.
MeSH Terms
Figure
Cited by 1 articles
-
Utilizing Immunoglobulin G4 Immunohistochemistry for Risk Stratification in Patients with Papillary Thyroid Carcinoma Associated with Hashimoto Thyroiditis
Faridul Haq, Gyeongsin Park, Sora Jeon, Mitsuyoshi Hirokawa, Chan Kwon Jung
Endocrinol Metab. 2024;39(3):468-478. doi: 10.3803/EnM.2024.1923.
Reference
-
1. Travis WD, Galvin JR. Non-neoplastic pulmonary lymphoid lesions. Thorax. 2001; 56:964–71.2. Guinee DG Jr. Update on nonneoplastic pulmonary lymphoproliferative disorders and related entities. Arch Pathol Lab Med. 2010; 134:691–701.
Article3. Yi E, Aubry MC. Pulmonary pseudoneoplasms. Arch Pathol Lab Med. 2010; 134:417–26.
Article4. Saltzstein SL. Pulmonary malignant lymphomas and pseudolymphomas: classification, therapy, and prognosis. Cancer. 1963; 16:928–55.
Article5. Kradin RL, Mark EJ. Benign lymphoid disorders of the lung, with a theory regarding their development. Hum Pathol. 1983; 14:857–67.
Article6. Abbondanzo SL, Rush W, Bijwaard KE, Koss MN. Nodular lymphoid hyperplasia of the lung: a clinicopathologic study of 14 cases. Am J Surg Pathol. 2000; 24:587–97.7. Sirajuddin A, Raparia K, Lewis VA, et al. Primary pulmonary lymphoid lesions: radiologic and pathologic findings. Radiographics. 2016; 36:53–70.
Article8. Poletti V, Ravaglia C, Tomassetti S, et al. Lymphoproliferative lung disorders: clinicopathological aspects. Eur Respir Rev. 2013; 22:427–36.
Article9. Arcadu A, Moua T, Yi ES, Ryu JH. Lymphoid interstitial pneumonia and other benign lymphoid disorders. Semin Respir Crit Care Med. 2016; 37:406–20.
Article10. Begueret H, Vergier B, Parrens M, et al. Primary lung small B-cell lymphoma versus lymphoid hyperplasia: evaluation of diagnostic criteria in 26 cases. Am J Surg Pathol. 2002; 26:76–81.11. Tashtoush B, Okafor NC, Ramirez JF, Smolley L. Follicular bronchiolitis: a literature review. J Clin Diagn Res. 2015; 9:OE01–5.
Article12. Guinee DG Jr, Franks TJ, Gerbino AJ, Murakami SS, Acree SC, Koss MN. Pulmonary nodular lymphoid hyperplasia (pulmonary pseudolymphoma): the significance of increased numbers of IgG4-positive plasma cells. Am J Surg Pathol. 2013; 37:699–709.13. Bois MC, Sekiguchi H, Ryu JH, Yi ES. No definite clinical features of immunoglobulin G4-related disease in patients with pulmonary nodular lymphoid hyperplasia. Hum Pathol. 2017; 59:80–6.
Article14. Atzeni F, Gerardi MC, Barilaro G, Masala IF, Benucci M, Sarzi-Puttini P. Interstitial lung disease in systemic autoimmune rheumatic diseases: a comprehensive review. Expert Rev Clin Immunol. 2018; 14:69–82.
Article15. Mittoo S, Gelber AC, Christopher-Stine L, Horton MR, Lechtzin N, Danoff SK. Ascertainment of collagen vascular disease in patients presenting with interstitial lung disease. Respir Med. 2009; 103:1152–8.
Article16. Song MK, Seol YM, Park YE, et al. Pulmonary nodular lymphoid hyperplasia associated with Sjogren's syndrome. Korean J Intern Med. 2007; 22:192–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Small Intestinal Nodular Lymphoid Hyperplasia
- A Case of Primary Jejunal Malignant Lymphoma Associated with Nodular Lymphoid Hyperplasia
- Surgical Treatment of the Pulmonary Nodular Lymphoid Hyperplasia: A case report
- Pulmonary Nodular Lymphoid Hyperplasia in a 33-Year-Old Woman
- Pulmonary Nodular Lymphoid Hyperplasia Associated with Sj?gren's Syndrome