Korean J Gastroenterol.
2018 Jun;71(6):324-331. 10.4166/kjg.2018.71.6.324.
Gastrointestinal Gas and Abdominal Fat Quantity Measured by Three-Dimensional Abdominal Computed Tomography in Patients with Functional Bloating
- Affiliations
-
- 1Department of Gastroenterology, Ajou University School of Medicine, Suwon, Korea. kjleemd@hotmail.com
- 2Department of Gastroenterology, Myongji Hospital, Goyang, Korea.
- 3Department of Radiology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2414458
- DOI: http://doi.org/10.4166/kjg.2018.71.6.324
Abstract
- BACKGROUND/AIMS
The aim of this study was to assess whether increased intestinal gas or fat content in the abdominal cavity is related to abdominal bloating, using three-dimensional abdominal computed tomography scan.
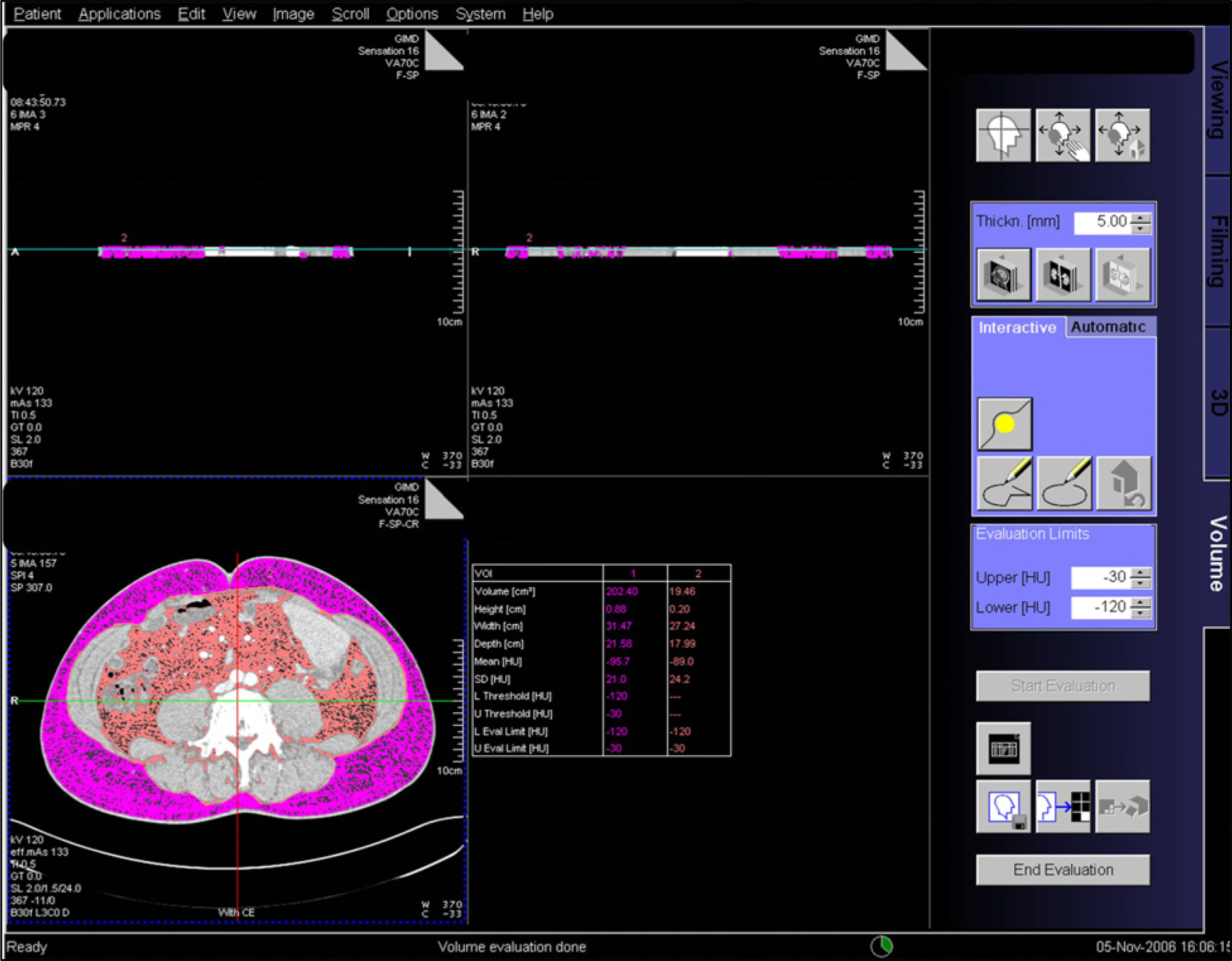
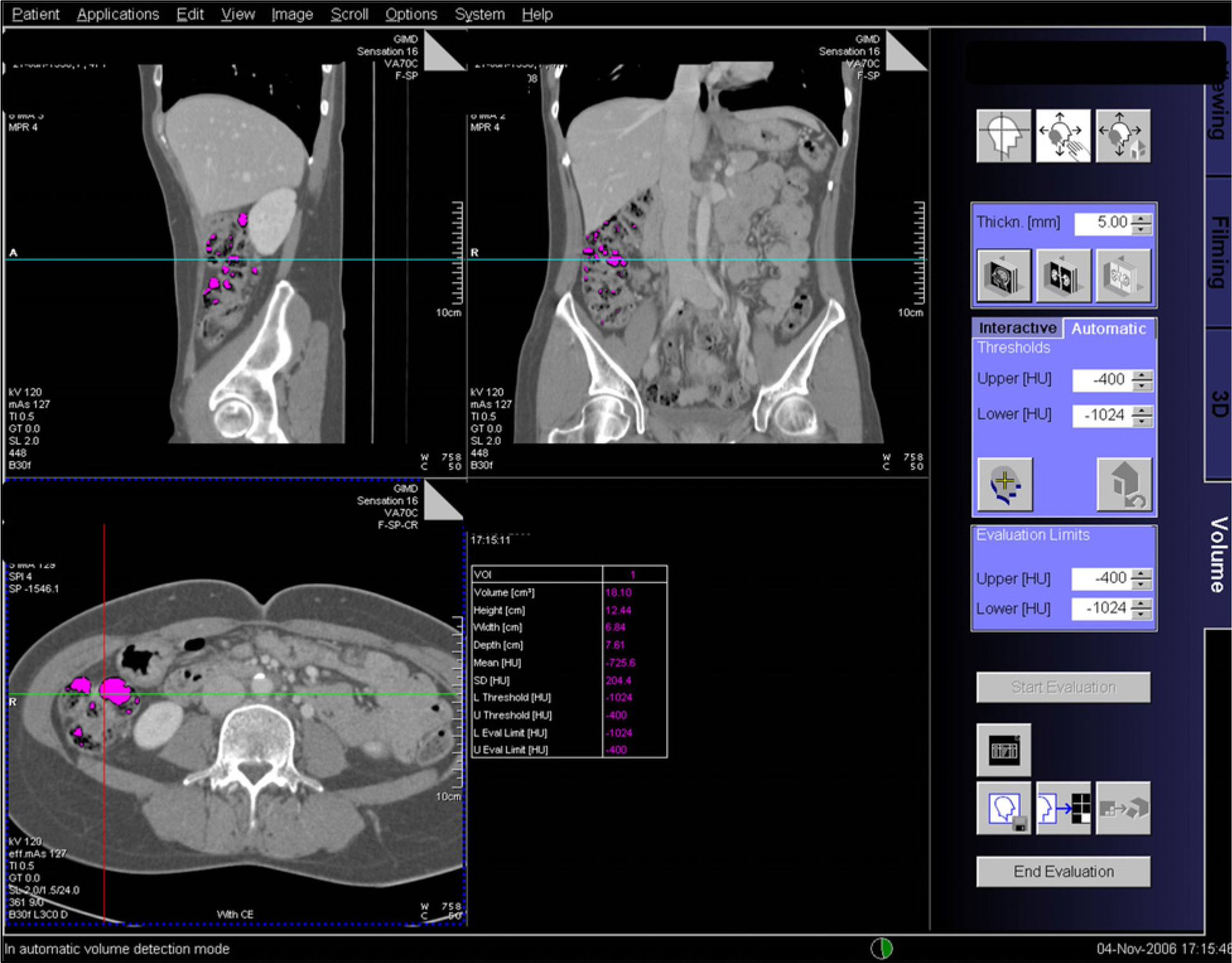
METHODS
Twenty-nine healthy individuals without abdominal bloating and organic disease (15 women; mean age, 49 years; range of age, 23-73 years) and 30 patients with chronic recurrent abdominal bloating-diagnosed with functional bloating (10 women; mean age, 53 years; range of age, 35-75 years) - participated in this study. The mean values of measured parameters were compared using independent sample t-test.
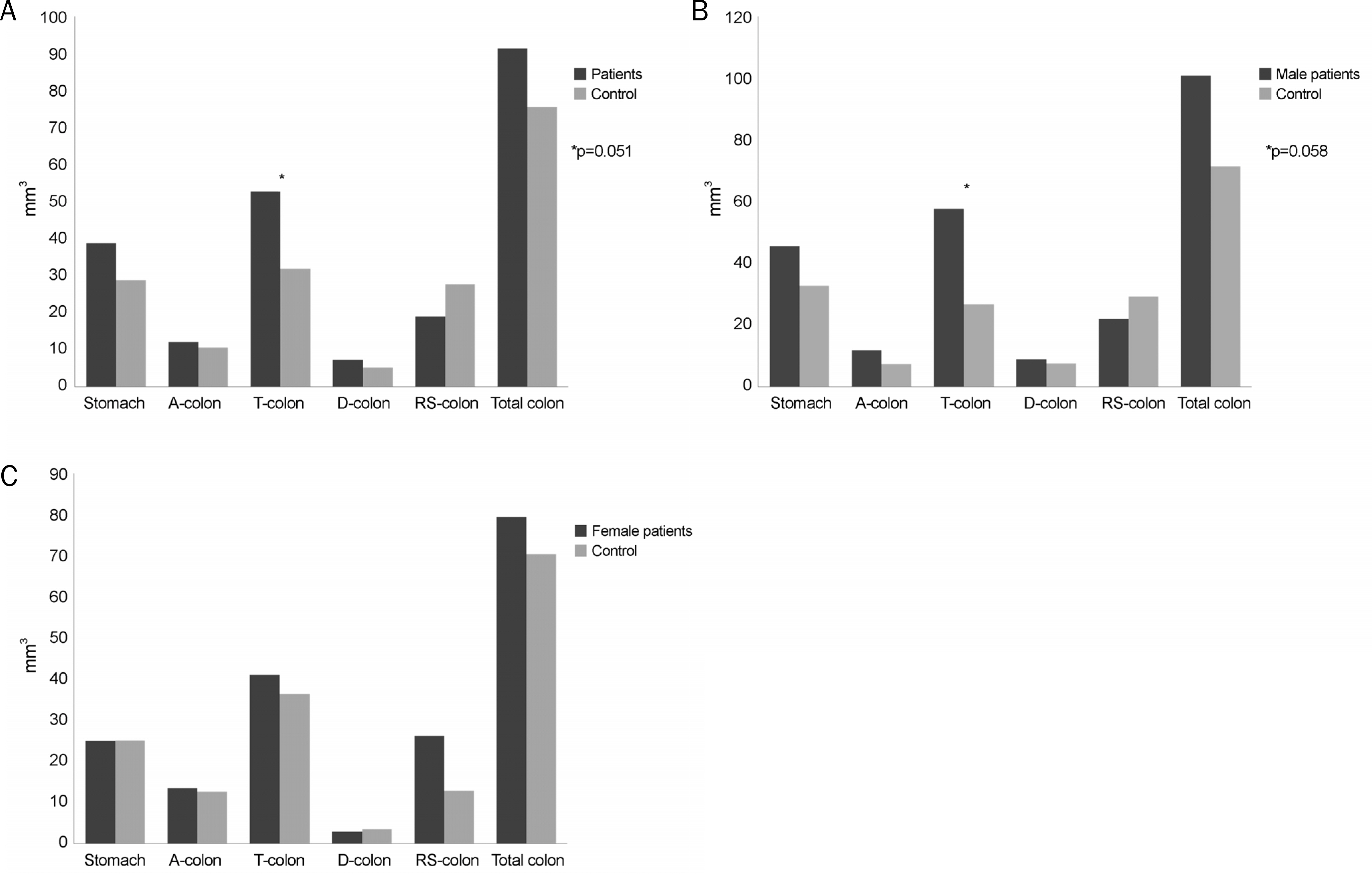
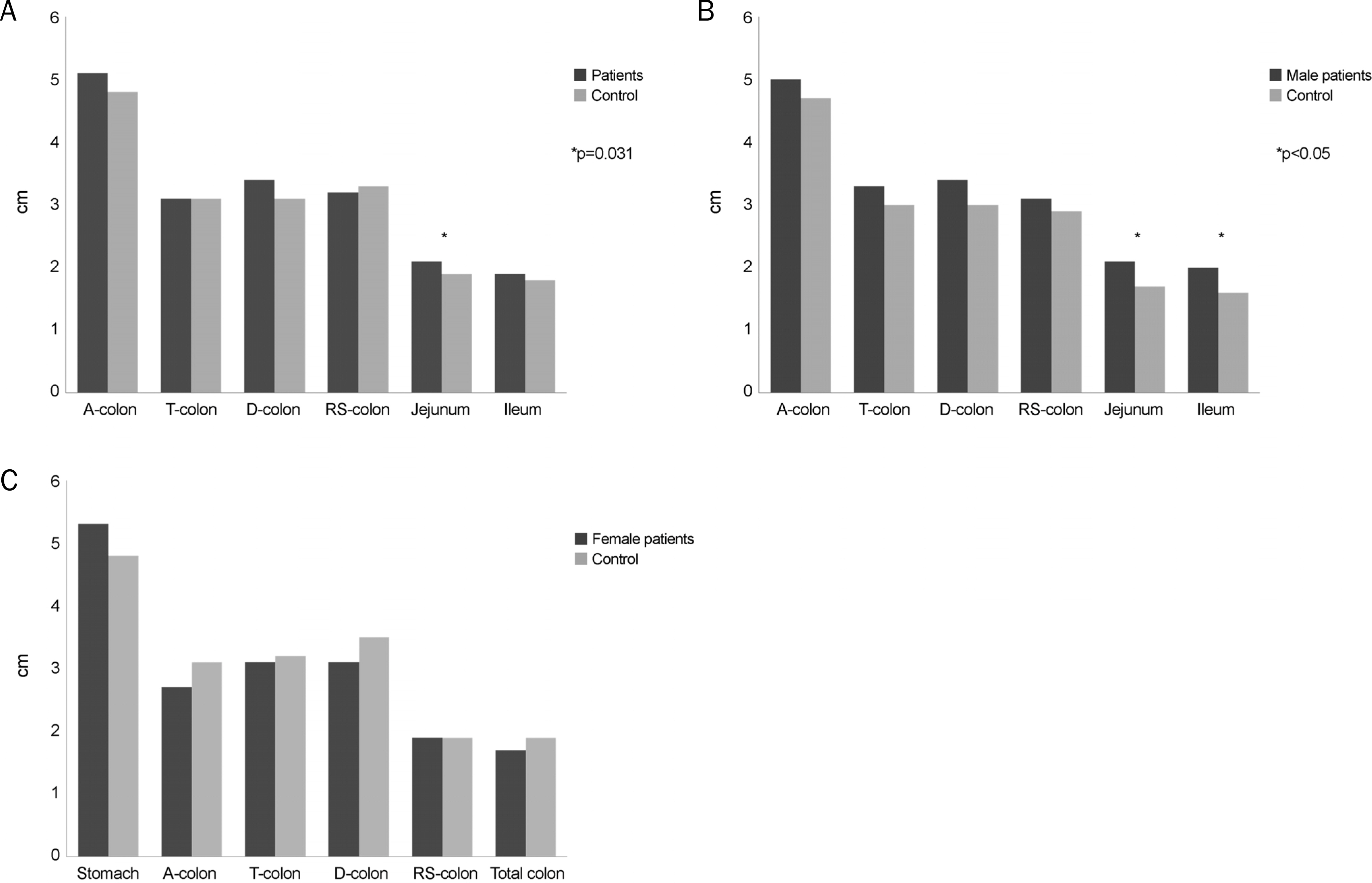
RESULTS
The mean volume of total colon gas in bloated patients was similar to that in control subjects. The distribution of intra-abdominal gas was also similar between the two groups. However, the amount of gas in the transverse colon tended to be significantly higher in patients with bloating than in controls (p=0.06). Body mass index was similar between the two groups (23.4±3.2 kg/m2 and 22.3±3.1 kg/m2, respectively). Moreover, no significant differences with respect to circumferential area, subcutaneous fat, visceral fat area, and total fat area were found between the two groups.
CONCLUSIONS
Bloating might not just be the result of gastrointestinal gas or intra-abdominal fat. Other contributing factors, such as localized abnormality in gas distribution and visceral hypersensitivity, may be involved.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Usefulness of Gastrointestinal Gas Measurement in Patients with Functional Bloating
Hyun Jin Kim
Korean J Gastroenterol. 2018;71(6):301-302. doi: 10.4166/kjg.2018.71.6.301.Bloating in a supine position
Akira Hokama, Yasuka Nakada, Aki Yanagida, Erika Koga, Kunikazu Hoshino, Jiro Fujita
Intest Res. 2021;19(2):252-253. doi: 10.5217/ir.2020.00019.
Reference
-
References
1. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006; 130:1480–1491.
Article2. Ryu MS, Jung HK, Ryu JI, Kim JS, Kong KA. Clinical dimensions of bloating in functional gastrointestinal disorders. J Neurogastroenterol Motil. 2016; 22:509–516.
Article3. Jiang X, Locke GR 3rd, Choung RS, Zinsmeister AR, Schleck CD, Talley NJ. Prevalence and risk factors for abdominal bloating and visible distention: a population-based study. Gut. 2008; 57:756–763.
Article4. Ringel Y, Williams RE, Kalilani L, Cook SF. Prevalence, characteristics, and impact of bloating symptoms in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009; 7:68–72. quiz 3.
Article5. Azpiroz F, Malagelada JR. Abdominal bloating. Gastroenterology. 2005; 129:1060–1078.
Article6. Lasser RB, Bond JH, Levitt MD. The role of intestinal gas in functional abdominal pain. N Engl J Med. 1975; 293:524–526.
Article7. Serra J, Azpiroz F, Malagelada JR. Impaired transit and tolerance of intestinal gas in the irritable bowel syndrome. Gut. 2001; 48:14–19.
Article8. Koide A, Yamaguchi T, Odaka T, et al. Quantitative analysis of bowel gas using plain abdominal radiograph in patients with irritable bowel syndrome. Am J Gastroenterol. 2000; 95:1735–1741.
Article9. Maxton DG, Martin DF, Whorwell PJ, Godfrey M. Abdominal distension in female patients with irritable bowel syndrome: exploration of possible mechanisms. Gut. 1991; 32:662–664.
Article10. Accarino A, Perez F, Azpiroz F, Quiroga S, Malagelada JR. Intestinal gas and bloating: effect of prokinetic stimulation. Am J Gastroenterol. 2008; 103:2036–2042.
Article11. van Oijen MG, Josemanders DF, Laheij RJ, van Rossum LG, Tan AC, Jansen JB. Gastrointestinal disorders and symptoms: does body mass index matter? Neth J Med. 2006; 64:45–49.12. Delgado-Aros S, Locke GR 3rd, Camilleri M, et al. Obesity is associated with increased risk of gastrointestinal symptoms: a population-based study. Am J Gastroenterol. 2004; 99:1801–1806.
Article13. Vehmas T, Kairemo KJ, Taavitsainen MJ. Measuring visceral adipose tissue content from contrast enhanced computed tomography. Int J Obes Relat Metab Disord. 1996; 20:570–573.14. Song KH, Jung HK, Min BH, et al. Development and validation of the Korean Rome III questionnaire for diagnosis of functional gastrointestinal disorders. J Neurogastroenterol Motil. 2013; 19:509–515.
Article15. Adam A, Dixon AK. Grainger & Allison's diagnostic radiology: a textbook of medical imaging. 5th ed.Philadelphia: Churchill Livingstone/Elsevier;2008.16. Chang L, Lee OY, Naliboff B, Schmulson M, Mayer EA. Sensation of bloating and visible abdominal distension in patients with irritable bowel syndrome. Am J Gastroenterol. 2001; 96:3341–3347.
Article17. Lembo T, Naliboff B, Munakata J, et al. Symptoms and visceral perception in patients with pain-predominant irritable bowel syndrome. Am J Gastroenterol. 1999; 94:1320–1326.
Article18. Houghton LA, Lea R, Agrawal A, Reilly B, Whorwell PJ. Relationship of abdominal bloating to distention in irritable bowel syndrome and effect of bowel habit. Gastroenterology. 2006; 131:1003–1010.
Article19. King TS, Elia M, Hunter JO. Abnormal colonic fermentation in irritable bowel syndrome. Lancet. 1998; 352:1187–1189.
Article20. Mc Williams SR, Mc Laughlin PD, O'Connor OJ, et al. Computed tomography assessment of intestinal gas volumes in functional gastrointestinal disorders. J Neurogastroenterol Motil. 2012; 18:419–425.
Article21. Serra J, Azpiroz F, Malagelada JR. Mechanisms of intestinal gas retention in humans: impaired propulsion versus obstructed evacuation. Am J Physiol Gastrointest Liver Physiol. 2001; 281:G138–G143.
Article22. Lam C, Chaddock G, Marciani Laurea L, et al. Distinct abnormalities of small bowel and regional colonic volumes in subtypes of irritable bowel syndrome revealed by MRI. Am J Gastroenterol. 2017; 112:346–355.
Article23. Kellow JE, Phillips SF, Miller LJ, Zinsmeister AR. Dysmotility of the small intestine in irritable bowel syndrome. Gut. 1988; 29:1236–1243.
Article24. Kellow JE, Phillips SF. Altered small bowel motility in irritable bowel syndrome is correlated with symptoms. Gastroenterology. 1987; 92:1885–1893.
Article25. Hernando-Harder AC, Serra J, Azpiroz F, et al. Colonic responses to gas loads in subgroups of patients with abdominal bloating. Am J Gastroenterol. 2010; 105:876–882.
Article26. Agrawal A, Whorwell PJ. Review article: abdominal bloating and distension in functional gastrointestinal disorders–epidemiology and exploration of possible mechanisms. Aliment Pharmacol Ther. 2008; 27:2–10.27. Ludidi S, Mujagic Z, Jonkers D, et al. Markers for visceral hypersensitivity in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2014; 26:1104–1111.
Article28. Lee KJ. Obesity and functional gastrointestinal disorders. Korean J Gastroenterol. 2012; 59:1–7.
Article29. Eslick GD. Gastrointestinal symptoms and obesity: a metaanalysis. Obes Rev. 2012; 13:469–479.
Article30. Sullivan SN. A prospective study of unexplained visible abdominal bloating. N Z Med J. 1994; 107:428–430.31. Eslick GD, Howell SC, Talley NJ. Dysmotility symptoms are independently associated with weight change: a population-based study of Australian adults. J Neurogastroenterol Motil. 2015; 21:603–611.
Article32. Bendezú RA, Barba E, Burri E, et al. Colonic content in health and its relation to functional gut symptoms. Neurogastroenterol Motil. 2016; 28:849–854.
Article33. Accarino A, Perez F, Azpiroz F, Quiroga S, Malagelada JR. Abdominal distention results from caudo-ventral redistribution of contents. Gastroenterology. 2009; 136:1544–1551.
Article