J Korean Assoc Oral Maxillofac Surg.
2017 Aug;43(4):229-238. 10.5125/jkaoms.2017.43.4.229.
Risk factor analysis of additional administration of sedative agent and patient dissatisfaction in intravenous conscious sedation using midazolam for third molar extraction
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dankook University Jukjeon Dental Hospital, Yongin, Korea.
- 2Department of Oral and Maxillofacial Surgery, Gachon University Gil Medical Center, Incheon, Korea.
- 3Department of Oral and Maxillofacial Surgery, Section of Dentistry, SMG-SNU Boramae Medical Center, Seoul, Korea. neo0224@gmail.com
- 4Section of Dentistry, SMG-SNU Boramae Medical Center, Seoul, Korea.
- KMID: 2391353
- DOI: http://doi.org/10.5125/jkaoms.2017.43.4.229
Abstract
OBJECTIVES
The primary purpose of this study was to investigate the factors related with additional administration of sedative agent during intravenous conscious sedation (IVS) using midazolam (MDZ). The secondary purpose was to analyze the factors affecting patient satisfaction.
MATERIALS AND METHODS
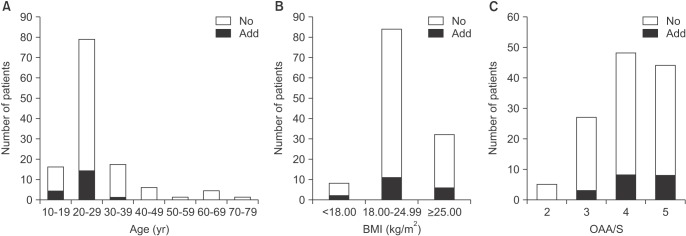
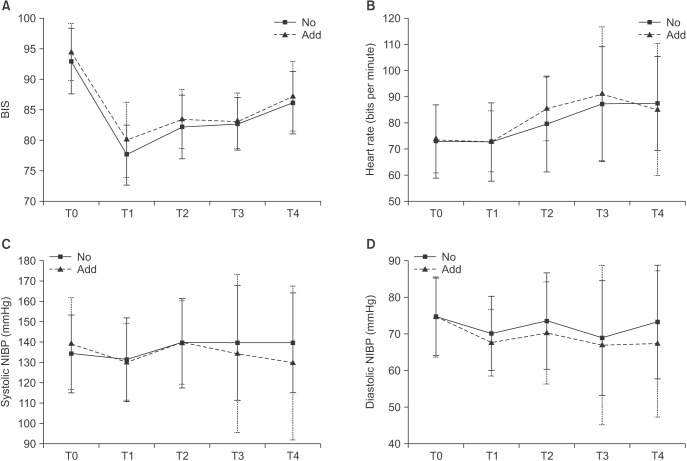
Clinical data for 124 patients who had undergone surgical extraction of mandibular third molar under IVS using MDZ were retrospectively investigated in this case-control study. The initial dose of MDZ was determined by body mass index (BMI) and weight. In the case of insufficient sedation at the beginning of surgery, additional doses were injected. During surgery, peripheral oxygen saturation, bispectral index score (BIS), heart rate, and blood pressure were monitored and recorded. The predictor variables were sex, age, BMI, sleeping time ratio, dental anxiety, Pederson scale, and initial dose of MDZ. The outcome variables were additional administration of MDZ, observer's assessment of alertness/sedation, intraoperative amnesia, and patient satisfaction. Descriptive statistics were computed, and the P-value was set at 0.05.
RESULTS
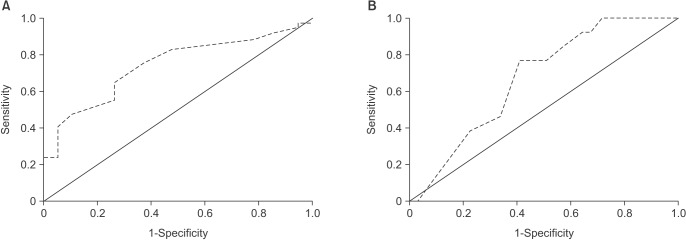
Most patients had an adequate level of sedation with only the initial dose of MDZ and were satisfied with the treatment under sedation; however, 19 patients needed additional administration, and 13 patients were unsatisfied. In multivariable logistic analysis, lower age (odds ratio [OR], 0.825; P=0.005) and higher dental anxiety (OR, 5.744; P=0.003) were related to additional administration; lower intraoperative amnesia (OR, 0.228; P=0.002) and higher BIS right before MDZ administration (OR, 1.379; P=0.029) had relevance to patient dissatisfaction.
CONCLUSION
The preoperative consideration of age and dental anxiety is necessary for appropriate dose determination of MDZ in the minor oral surgery under IVS. The amnesia about the procedure affects patient satisfaction positively.
MeSH Terms
Figure
Reference
-
1. Van der Bijl P, Roelofse JA, Joubert JJ, Breytenbach HS. Intravenous midazolam in oral surgery. Int J Oral Maxillofac Surg. 1987; 16:325–332. PMID: 3112262.
Article2. Rodgers SF, Rodgers MS. Safety of intravenous sedation administered by the operating oral surgeon: the second 7 years of office practice. J Oral Maxillofac Surg. 2011; 69:2525–2529. PMID: 21724314.
Article3. Dundee JW, Halliday NJ, Harper KW, Brogden RN. Midazolam. A review of its pharmacological properties and therapeutic use. Drugs. 1984; 28:519–543. PMID: 6394264.
Article4. Agostoni M, Fanti L, Arcidiacono PG, Gemma M, Strini G, Torri G, et al. Midazolam and pethidine versus propofol and fentanyl patient controlled sedation/analgesia for upper gastrointestinal tract ultrasound endoscopy: a prospective randomized controlled trial. Dig Liver Dis. 2007; 39:1024–1029. PMID: 17913605.
Article5. Ryu DS, Lee DW, Choi SC, Oh IH. Sedation protocol using dexmedetomidine for third molar extraction. J Oral Maxillofac Surg. 2016; 74:926.e1–926.e7. PMID: 26850877.
Article6. Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007; 66:27–34. PMID: 17591470.
Article7. Aldrete JA. Modifications to the postanesthesia score for use in ambulatory surgery. J Perianesth Nurs. 1998; 13:148–155. PMID: 9801540.8. Koerner KR. The removal of impacted third molars. Principles and procedures. Dent Clin North Am. 1994; 38:255–278. PMID: 8206177.9. Corah NL. Development of a dental anxiety scale. J Dent Res. 1969; 48:596. PMID: 5256508.
Article10. Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, et al. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990; 10:244–251. PMID: 2286697.11. Göktay O, Satilmiş T, Garip H, Gönül O, Göker K. A comparison of the effects of midazolam/fentanyl and midazolam/tramadol for conscious intravenous sedation during third molar extraction. J Oral Maxillofac Surg. 2011; 69:1594–1599. PMID: 21277062.
Article12. Ustün Y, Gündüz M, Erdoğan O, Benlidayi ME. Dexmedetomidine versus midazolam in outpatient third molar surgery. J Oral Maxillofac Surg. 2006; 64:1353–1358. PMID: 16916668.13. Moore PA, Finder RL, Jackson DL. Multidrug intravenous sedation: determinants of the sedative dose of midazolam. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84:5–10. PMID: 9247941.14. Zacharias M, Hunter KM, Luyk NH. Patient-controlled sedation using midazolam. Br J Oral Maxillofac Surg. 1994; 32:168–173. PMID: 8068589.
Article15. Jirapinyo P, Abu Dayyeh BK, Thompson CC. Conscious sedation for upper endoscopy in the gastric bypass patient: prevalence of cardiopulmonary adverse events and predictors of sedation requirement. Dig Dis Sci. 2014; 59:2173–2177. PMID: 24723069.
Article16. Maeda S, Tomayasu Y, Higuchi H, Ishii-Maruhama M, Yamane A, Yabuki A, et al. Independent factors affecting recovery time after sedation in patients with intellectual disabilities. Open Dent J. 2015; 9:146–149. PMID: 25926898.
Article17. Brill MJ, van Rongen A, Houwink AP, Burggraaf J, van Ramshorst B, Wiezer RJ, et al. Midazolam pharmacokinetics in morbidly obese patients following semi-simultaneous oral and intravenous administration: a comparison with healthy volunteers. Clin Pharmacokinet. 2014; 53:931–941. PMID: 25141974.
Article18. Cillo JE Jr, Finn R. Correlation and comparison of body mass index on hemodynamics in hypertensive and normotensive patients undergoing intravenous sedation. J Oral Maxillofac Surg. 2006; 64:583–588. PMID: 16546636.
Article19. Moretto M, Kupski C, Mottin CC, Repetto G, Garcia Toneto M, Rizzolli J, et al. Hepatic steatosis in patients undergoing bariatric surgery and its relationship to body mass index and co-morbidities. Obes Surg. 2003; 13:622–624. PMID: 12940291.
Article20. Czwornog J, Austin GL. Body mass index, age, and gender affect prep quality, sedation use, and procedure time during screening colonoscopy. Dig Dis Sci. 2013; 58:3127–3133. PMID: 23812829.
Article21. Seto M, Furuta H, Sakamoto Y, Kikuta T. Sedative methods used during extraction of wisdom teeth in patients with a high level of dental anxiety. J Korean Assoc Oral Maxillofac Surg. 2011; 37:241–244.
Article22. Levitzky BE, Lopez R, Dumot JA, Vargo JJ. Moderate sedation for elective upper endoscopy with balanced propofol versus fentanyl and midazolam alone: a randomized clinical trial. Endoscopy. 2012; 44:13–20. PMID: 22068700.
Article23. Diercke K, Bürger GD, Bermejo JL, Lux CJ, Brunner M. The management of dental anxiety and impact of psychosomatic factors on dentistry: is recent scientific research translated into German dental practices? J Health Psychol. 2013; 18:1519–1528. PMID: 23221489.
Article24. Liu J, Singh H, White PF. Electroencephalogram bispectral analysis predicts the depth of midazolam-induced sedation. Anesthesiology. 1996; 84:64–69. PMID: 8572355.
Article25. Sleigh JW, Andrzejowski J, Steyn-Ross A, Steyn-Ross M. The bispectral index: a measure of depth of sleep? Anesth Analg. 1999; 88:659–661. PMID: 10072023.26. Chisholm CJ, Zurica J, Mironov D, Sciacca RR, Ornstein E, Heyer EJ. Comparison of electrophysiologic monitors with clinical assessment of level of sedation. Mayo Clin Proc. 2006; 81:46–52. PMID: 16438478.
Article27. Shah P, Manley G, Craig D. Bispectral index (BIS) monitoring of intravenous sedation for dental treatment. SAAD Dig. 2014; 30:7–11. PMID: 24624517.28. Munoz Garcia J, Vidal Marcos AV, Restoy Lozano A, Gasco Garcia C. Utility of bispectral index monitoring during intravenous sedation in the dental office. Int J Oral Maxillofac Implants. 2012; 27:375–382. PMID: 22442778.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The clinical study on the sedative effect and recovery in patients undergoing intravenous conscious sedation with midazolam for mandibular third molars extraction
- Considerations for submucosal midazolam administration in combination with oral and inhaled medications for sedation of pediatric dental patients
- Sedation at Sedation Clinic of Department of Dentistry in Hanyang University Medical Center (II)
- Administration order of midazolam/fentanyl for moderate dental sedation
- A Case of Midazolam Anaphylaxis