World J Mens Health.
2016 Dec;34(3):179-185. 10.5534/wjmh.2016.34.3.179.
Anti-Inflammatory and Antimicrobial Effects of a Novel Herbal Formulation (WSY-1075) in a Chronic Bacterial Prostatitis Rat Model
- Affiliations
-
- 1Department of Urology, College of Medicine, The Catholic University of Korea, Seoul, Korea. ksw1227@catholic.ac.kr
- 2Catholic Integrative Medicine Research Institute, The Catholic University of Korea, Seoul, Korea.
- KMID: 2364200
- DOI: http://doi.org/10.5534/wjmh.2016.34.3.179
Abstract
- PURPOSE
The aim of this study was to investigate the anti-inflammatory and anti-oxidative effects of a multi-herbal formula known as WSY-1075 in the treatment of chronic bacterial prostatitis in a rat model.
MATERIALS AND METHODS
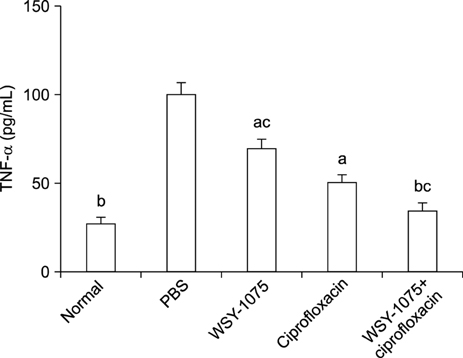
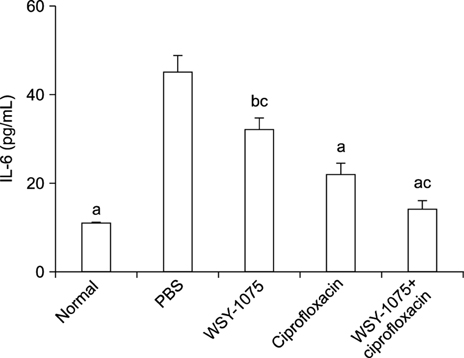
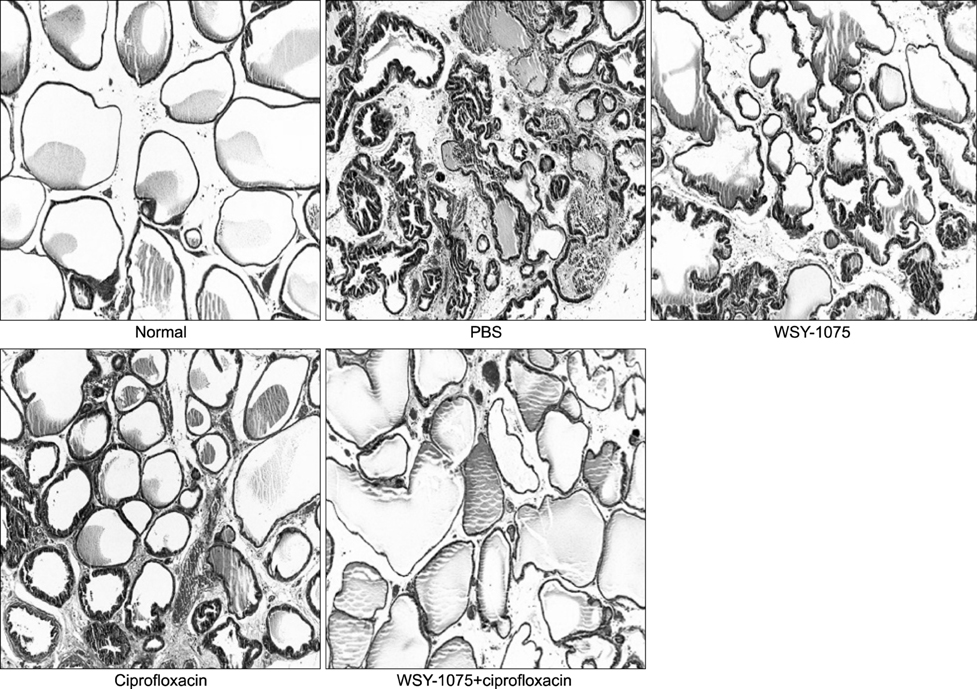
Experimental chronic bacterial prostatitis was induced in 32 Wistar rats by instillation of a bacterial suspension (Escherichia coli, 10⸠colony-forming units [CFU]/mL) into the prostatic urethra. After the induction of prostatitis, the rats were randomly divided into one of 4 treatment groups: control (n=8), ciprofloxacin (n=8), WSY-1075 (400 mg/kg) (n=8), and WSY-1075 (400 mg/kg)+ciprofloxacin (n=8). After 4 weeks of treatment, microbiological data from prostate tissue cultures, level of prostatic pro-inflammatory cytokines (tumor necrosis factor-α [TNF-α], interleukin [IL]-6, and IL-8), anti-oxidant effects (superoxide dismutase [SOD]), and histological findings were noted.
RESULTS
The WSY-1075, ciprofloxacin, and WSY-1075+ciprofloxacin groups showed fewer CFUs in prostate tissue cultures than the control group. The WSY-1075, ciprofloxacin and WSY-1075+ciprofloxacin groups showed statistically significantly lower levels of the pro-inflammatory cytokines TNF-α, IL-6, and IL-8 than the control group. SOD levels in the WSY-1075, ciprofloxacin and WSY-1075+ciprofloxacin groups were significantly higher than in the control group.
CONCLUSIONS
This study found that WSY-1075 had anti-microbial effects, anti-inflammatory effects, and anti-oxidative effects in a chronic bacterial prostatitis rat model. We expect the WSY-1075 may be useful for the clinical treatment of chronic bacterial prostatitis.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Improvement of Persistent Detrusor Overactivity through Treatment with a Phytotherapeutic Agent (WSY-1075) after Relief of Bladder Outlet Obstruction
Su Jin Kim, Seung Hwan Jeon, Eun Bi Kwon, Hyun Cheol Jeong, Sae Woong Choi, Woong Jin Bae, Hyuk Jin Cho, U-Syn Ha, Sung Hoo Hong, Ji Youl Lee, Sung Yeoun Hwang, Sae Woong Kim
World J Mens Health. 2018;36(2):153-160. doi: 10.5534/wjmh.17010.Letter to the Editor regarding the Article: “Anti-Inflammatory and Antimicrobial Effects of a Novel Herbal Formulation (WSY-1075) in a Chronic Bacterial Prostatitis Rat Model” by Park et al. World J Mens Health 2016;34(3):179-185
Yu Seob Shin, Bo Ram Choi, Jong Kwan Park
World J Mens Health. 2018;36(1):87-88. doi: 10.5534/wjmh.17044.
Reference
-
1. Pfau A. Prostatitis. A continuing enigma. Urol Clin North Am. 1986; 13:695–715.2. Wagenlehner FM, Weidner W, Naber KG. Therapy for prostatitis, with emphasis on bacterial prostatitis. Expert Opin Pharmacother. 2007; 8:1667–1674.
Article3. Nickel JC. Antibiotics for bacterial prostatitis. J Urol. 2000; 163:1407.
Article4. Shoskes DA, Manickam K. Herbal and complementary medicine in chronic prostatitis. World J Urol. 2003; 21:109–113.
Article5. Nadler RB, Koch AE, Calhoun EA, Campbell PL, Pruden DL, Bennett CL, et al. IL-1beta and TNF-alpha in prostatic secretions are indicators in the evaluation of men with chronic prostatitis. J Urol. 2000; 164:214–218.6. Shin S, Jeon JH, Park D, Jang JY, Joo SS, Hwang BY, et al. Anti-inflammatory effects of an ethanol extract of Angelica gigas in a Carrageenan-air pouch inflammation model. Exp Anim. 2009; 58:431–436.
Article7. Park CH, Noh JS, Kim JH, Tanaka T, Zhao Q, Matsumoto K, et al. Evaluation of morroniside, iridoid glycoside from Corni Fructus, on diabetes-induced alterations such as oxidative stress, inflammation, and apoptosis in the liver of type 2 diabetic db/db mice. Biol Pharm Bull. 2011; 34:1559–1565.
Article8. Lee JH, Lee JH, Lee YM, Kim PN, Jeong CS. Potential analgesic and anti-inflammatory activities of Panax ginseng head butanolic fraction in animals. Food Chem Toxicol. 2008; 46:3749–3752.
Article9. Oh YC, Cho WK, Im GY, Jeong YH, Hwang YH, Liang C, et al. Anti-inflammatory effect of Lycium Fruit water extract in lipopolysaccharide-stimulated RAW 264.7 macrophage cells. Int Immunopharmacol. 2012; 13:181–189.
Article10. Kim KW, Kim KS, Park SD, Kim JK, Chung KH, Kim DS, et al. Effect of Cervus korean TEMMINCK var. mantchuricus Swinhoe on protease activities, antioxidant and free radical damages in rheumatis arthritis rats. Toxicol In Vitro. 2008; 22:80–86.
Article11. Goto T, Kawahara M, Kawahara K, Mahinose S, Mizuma Y, Sakamoto N, et al. Experimental bacterial prostatitis in rats. Urol Res. 1991; 19:141–144.
Article12. Terai A, Yamamoto S, Mitsumori K, Okada Y, Kurazono H, Takeda Y, et al. Escherichia coli virulence factors and serotypes in acute bacterial prostatitis. Int J Urol. 1997; 4:289–294.
Article13. Draper HH, Hadley M. Malondialdehyde determination as index of lipid peroxidation. Methods Enzymol. 1990; 186:421–431.14. Jung JS, Shin JA, Park EM, Lee JE, Kang YS, Min SW, et al. Anti-inflammatory mechanism of ginsenoside Rh1 in lipopolysaccharide-stimulated microglia: critical role of the protein kinase A pathway and hemeoxygenase-1 expression. J Neurochem. 2010; 115:1668–1680.
Article15. Sung YH, Chang HK, Kim SE, Kim YM, Seo JH, Shin MC, et al. Anti-inflammatory and analgesic effects of the aqueous extract of corni fructus in murine RAW 264.7 macrophage cells. J Med Food. 2009; 12:788–795.
Article16. Kim JH, Jeong JH, Jeon ST, Kim H, Ock J, Suk K, et al. Decursin inhibits induction of inflammatory mediators by blocking nuclear factor-kappaB activation in macrophages. Mol Pharmacol. 2006; 69:1783–1790.17. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999; 282:236–237.
Article18. Yoon BI, Kim S, Han DS, Ha US, Lee SJ, Kim HW, et al. Acute bacterial prostatitis: how to prevent and manage chronic infection? J Infect Chemother. 2012; 18:444–450.
Article19. Wagenlehner FM, Pilatz A, Bschleipfer T, Diemer T, Linn T, Meinhardt A, et al. Bacterial prostatitis. World J Urol. 2013; 31:711–716.
Article20. Murphy AB, Macejko A, Taylor A, Nadler RB. Chronic prostatitis: management strategies. Drugs. 2009; 69:71–84.21. Sciarra A, Di Silverio F, Salciccia S, Autran Gomez AM, Gentilucci A, Gentile V. Inflammation and chronic prostatic diseases: evidence for a link? Eur Urol. 2007; 52:964–972.
Article22. Kramer G, Mitteregger D, Marberger M. Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? Eur Urol. 2007; 51:1202–1216.
Article23. Penna G, Mondaini N, Amuchastegui S, Degli Innocenti S, Carini M, Giubilei G, et al. Seminal plasma cytokines and chemokines in prostate inflammation: interleukin 8 as a predictive biomarker in chronic prostatitis/chronic pelvic pain syndrome and benign prostatic hyperplasia. Eur Urol. 2007; 51:524–533.
Article24. Yoon BI, Bae WJ, Kim SJ, Kim HS, Ha US, Sohn DW, et al. The anti-inflammatory effects of a new herbal formula (WSY-1075) in a nonbacterial prostatitis rat model. World J Mens Health. 2013; 31:150–156.
Article25. Zhou JF, Xiao WQ, Zheng YC, Dong J, Zhang SM. Increased oxidative stress and oxidative damage associated with chronic bacterial prostatitis. Asian J Androl. 2006; 8:317–323.
Article26. Vital P, Castro P, Ittmann M. Oxidative stress promotes benign prostatic hyperplasia. Prostate. 2016; 76:58–67.
Article27. Bae WJ, Ha US, Kim S, Kim SJ, Hong SH, Lee JY, et al. Reduction of oxidative stress may play a role in the anti-inflammatory effect of the novel herbal formulation in a rat model of hydrochloric acid-induced cystitis. Neurourol Urodyn. 2015; 34:86–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Anti-Inflammatory Effects of a New Herbal Formula (WSY-1075) in a Nonbacterial Prostatitis Rat Model
- Letter to the Editor regarding the Article: “Anti-Inflammatory and Antimicrobial Effects of a Novel Herbal Formulation (WSY-1075) in a Chronic Bacterial Prostatitis Rat Model†by Park et al. World J Mens Health 2016;34(3):179-185
- Improvement of Persistent Detrusor Overactivity through Treatment with a Phytotherapeutic Agent (WSY-1075) after Relief of Bladder Outlet Obstruction
- Anti-Inflammatory Effect of Phlorotannin on Chronic Nonbacterial Prostatitis in a Rat Model
- Preventive Effect on Inflammation and Anti-Inflammatory and Anti-Microbial Effects of Garlic Extract in a Rat Model of Chronic Bacterial Prostatitis