The Relationship Between Tongue Pressure and Oral Dysphagia in Stroke Patients
- Affiliations
-
- 1Department of Rehabilitation & Physical Medicine, Kyung-Hee Medical Center, Seoul, Korea.
- 2Department of Rehabilitation & Physical Medicine, Kyung-Hee University Hospital at Gangdong, Seoul, Korea. soyuns@gmail.com
- 3Department of Occupational Therapy, Inje University Busan Paik Hospital, Busan, Korea.
- KMID: 2356647
- DOI: http://doi.org/10.5535/arm.2016.40.4.620
Abstract
OBJECTIVE
To evaluate the relationships between tongue pressure and different aspects of the oral-phase swallowing function.
METHODS
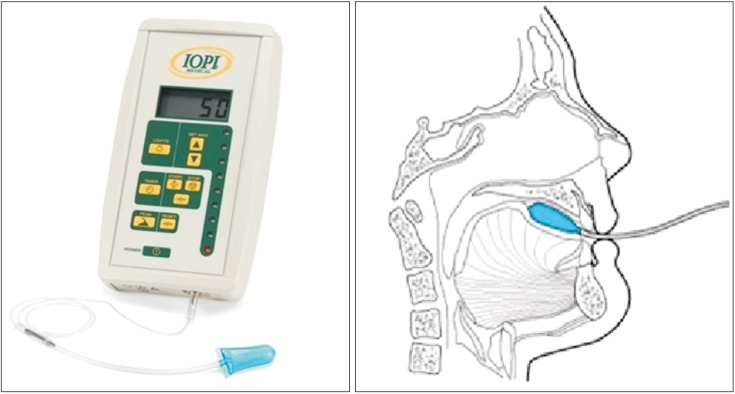
We included 96 stroke patients with dysphagia, ranging in age from 40 to 88 years (mean, 63.7 years). Measurements of tongue pressure were obtained with the Iowa Oral Performance Instrument, a device with established normative data. Three trials of maximum performance were performed for lip closure pressure (LP), anterior hard palate-to-tongue pressure (AP), and posterior hard palate-to-tongue pressure (PP); buccal-to-tongue pressures on both sides were also recorded (buccal-to-tongue pressure, on the weak side [BW]; buccal-to-tongue pressure, on the healthy side [BH]). The average pressure in each result was compared between the groups. Clinical evaluation of the swallowing function was performed with a videofluoroscopic swallowing study.
RESULTS
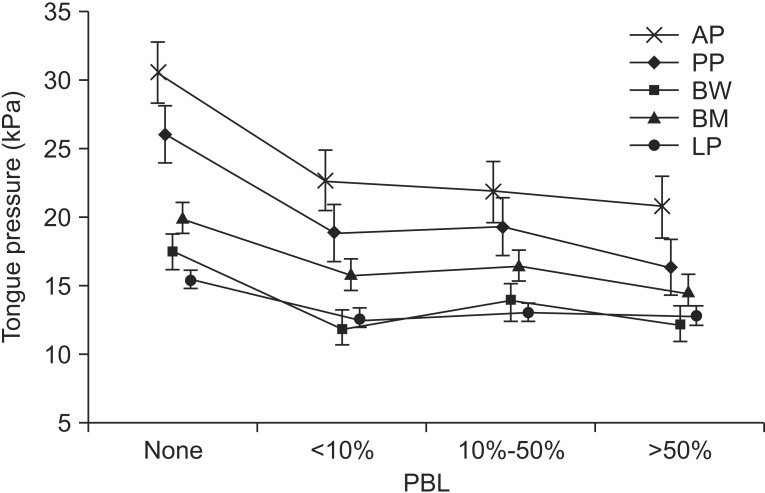
The average maximum AP and PP values in the intact LC group were significantly higher than those in the inadequate lip closure group (AP, p=0.003; PP, p<0.001). AP and PP showed significant relationships with bolus formation (BF), mastication, premature bolus loss (PBL), tongue to palate contact (TP), and oral transit time (OTT). Furthermore, LP, BW, and BH values were significantly higher in the groups with intact mastication, without PBL and intact TP.
CONCLUSION
These findings indicate that the tongue pressure appears to be closely related to the oral-phase swallowing function in post-stroke patients, especially BF, mastication, PBL, TP and OTT.
Figure
Cited by 3 articles
-
Association of Post-extubation Dysphagia With Tongue Weakness and Somatosensory Disturbance in Non-neurologic Critically Ill Patients
Hee Seon Park, Jung Hoi Koo, Sun Hong Song
Ann Rehabil Med. 2017;41(6):961-968. doi: 10.5535/arm.2017.41.6.961.Decreased Maximal Tongue Protrusion Length May Predict the Presence of Dysphagia in Stroke Patients
Hyunchul Cho, Jeong Se Noh, Junwon Park, Changwook Park, No Dam Park, Jun Young Ahn, Ji Woong Park, Yoon-Hee Choi, Seong-Min Chun
Ann Rehabil Med. 2021;45(6):440-449. doi: 10.5535/arm.21126.Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
Back Min Oh, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Su Jung Park, Beom Jin Kim, Hyun Jung Kim
Ann Rehabil Med. 2023;47(3):192-204. doi: 10.5535/arm.23018.
Reference
-
1. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.2. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204. PMID: 8685928.3. Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990; 154:953–963. PMID: 2108569.
Article4. Daniels SK, Brailey K, Foundas AL. Lingual discoordination and dysphagia following acute stroke: analyses of lesion localization. Dysphagia. 1999; 14:85–92. PMID: 10028038.
Article5. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-Ed;1998.6. Konaka K, Kondo J, Hirota N, Tamine K, Hori K, Ono T, et al. Relationship between tongue pressure and dysphagia in stroke patients. Eur Neurol. 2010; 64:101–107. PMID: 20628254.
Article7. Ku DN, Ma PP, McConnel FM, Cerenko D. A kinematic study of the oropharyngeal swallowing of a liquid. Ann Biomed Eng. 1990; 18:655–669. PMID: 2281886.
Article8. Clark HM, Henson PA, Barber WD, Stierwalt JA, Sherrill M. Relationships among subjective and objective measures of tongue strength and oral phase swallowing impairments. Am J Speech Lang Pathol. 2003; 12:40–50. PMID: 12680812.
Article9. Horner J, Massey EW. Silent aspiration following stroke. Neurology. 1988; 38:317–319. PMID: 3340301.
Article10. Roth EJ. Medical complications encountered in stroke rehabilitation. Phys Med Rehabil Clin North Am. 1991; 2:563–577.
Article11. DePippo KL, Holas MA, Reding MJ, Mandel FS, Lesser ML. Dysphagia therapy following stroke: a controlled trial. Neurology. 1994; 44:1655–1660. PMID: 7936292.
Article12. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335. PMID: 19717014.
Article13. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article14. Logemann JA. Manual for the videofluorographic study of swallowing. 2nd ed. Austin: Pro-Ed;1993.15. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008; 23:59–64. PMID: 17602263.
Article16. Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995; 50:M257–M262. PMID: 7671027.
Article17. Park JS, You SJ, Kim JY, Yeo SG, Lee JH. Differences in orofacial muscle strength according to age and sex in East Asian healthy adults. Am J Phys Med Rehabil. 2015; 94:677–686. PMID: 25415391.
Article18. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989; 42:703–709. PMID: 2760661.
Article19. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.20. Pouderoux P, Kahrilas PJ. Deglutitive tongue force modulation by volition, volume, and viscosity in humans. Gastroenterology. 1995; 108:1418–1426. PMID: 7729634.
Article21. Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005; 53:1483–1489. PMID: 16137276.
Article22. Hagg M, Anniko M. Influence of lip force on swallowing capacity in stroke patients and in healthy subjects. Acta Otolaryngol. 2010; 130:1204–1208. PMID: 20443741.23. Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008; 19:691–707. PMID: 18940636.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Decreased Maximal Tongue Protrusion Length May Predict the Presence of Dysphagia in Stroke Patients
- Oral Mucosal Lesion Related with Dysphagia
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Comparison of Effects of the Volume, Texture and Taste of Food on Tongue Pressure
- Dysphagia after Oral Cavity and Hypopharyngeal Cancer Surgery