Ann Rehabil Med.
2021 Dec;45(6):440-449. 10.5535/arm.21126.
Decreased Maximal Tongue Protrusion Length May Predict the Presence of Dysphagia in Stroke Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 2Department of Physical Medicine and Rehabilitation, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- 3Department of Physical Medicine and Rehabilitation, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- KMID: 2523841
- DOI: http://doi.org/10.5535/arm.21126
Abstract
Objective
To investigate the relationship between maximal tongue protrusion length (MTPL) and dysphagia in post-stroke patients.
Methods
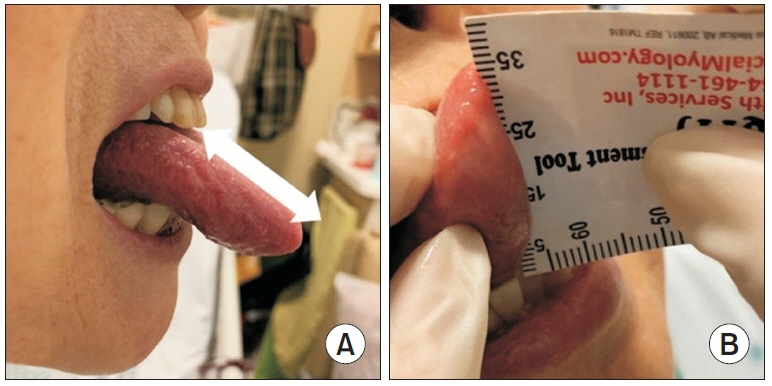
Free tongue length (FTL) was measured using the quick tongue-tie assessment tool and MTPL was measured using a transparent plastic ruler in 47 post-stroke patients. The MTPL-to-FTL (RMF) ratio was calculated. Swallowing function in all patients was evaluated via videofluoroscopic swallowing study (VFSS), PenetrationAspiration Scale (PAS), Functional Oral Intake Scale (FOIS), and Videofluoroscopic Dysphagia Scale (VDS).
Results
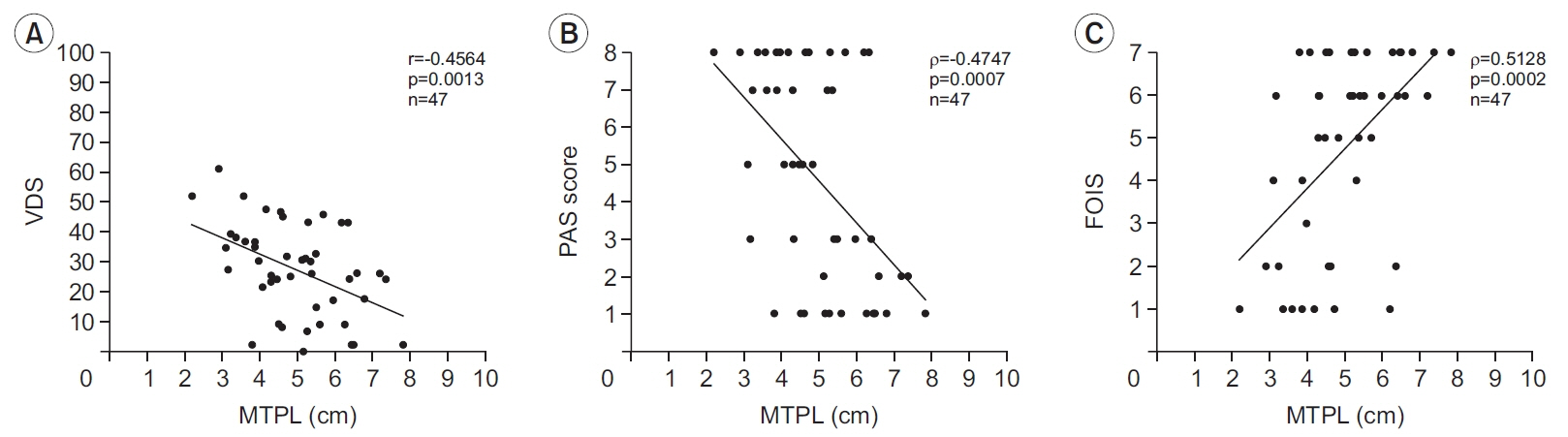
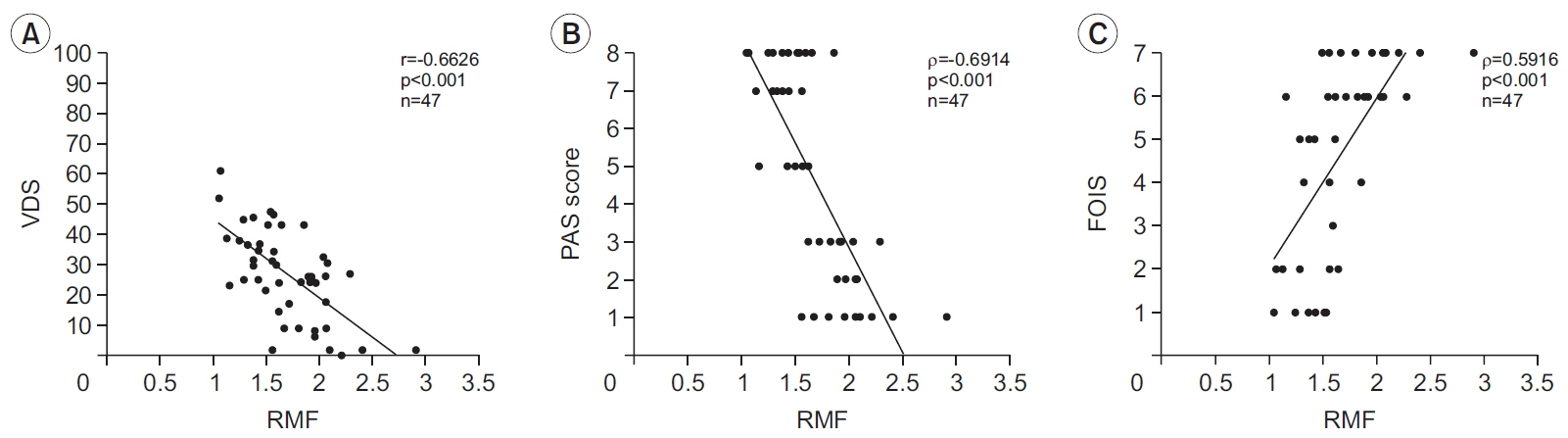
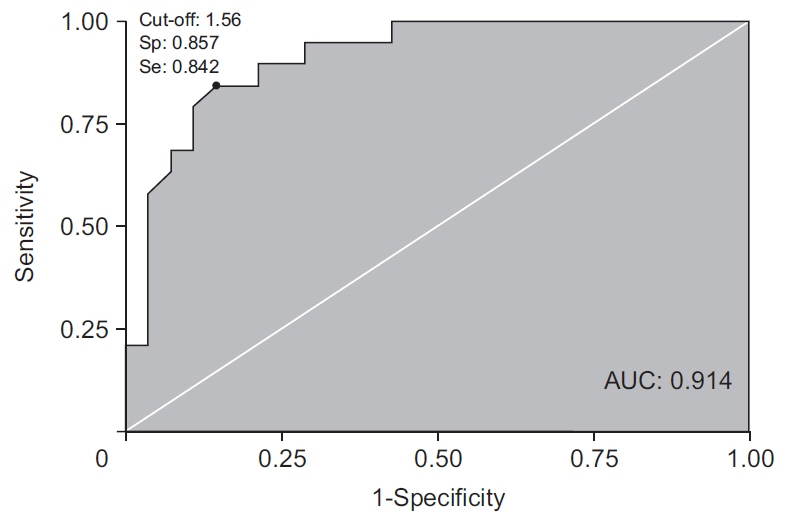
The MTPL and RMF values were significantly higher in the non-aspirator group than in the aspirator group (MTPL, p=0.0049; RMF, p<0.001). MTPL and RMF showed significant correlations with PAS, FOIS and VDS scores. The cut-off value in RMF for the prediction of aspiration was 1.56, with a sensitivity of 84% and a specificity of 86%.
Conclusion
There is a relationship between MTPL and dysphagia in post-stroke patients. MTPL and RMF can be useful for detecting aspiration in post-stroke patients.
Figure
Cited by 1 articles
-
Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
Back Min Oh, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Su Jung Park, Beom Jin Kim, Hyun Jung Kim
Ann Rehabil Med. 2023;47(3):192-204. doi: 10.5535/arm.23018.
Reference
-
1. Cohen DL, Roffe C, Beavan J, Blackett B, Fairfield CA, Hamdy S, et al. Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke. 2016; 11:399–411.
Article2. Bray BD, Smith CJ, Cloud GC, Enderby P, James M, Paley L, et al. The association between delays in screening for and assessing dysphagia after acute stroke, and the risk of stroke-associated pneumonia. J Neurol Neurosurg Psychiatry. 2017; 88:25–30.
Article3. Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009; 40:1903–6.
Article4. Groher ME, Crary MA. Dysphagia: clinical management in adults and children. St. Louis, MO: Elsevier;2015.5. Pearson WG Jr, Langmore SE, Zumwalt AC. Evaluating the structural properties of suprahyoid muscles and their potential for moving the hyoid. Dysphagia. 2011; 26:345–51.
Article6. Beom J, Oh BM, Choi KH, Kim W, Song YJ, You DS, et al. Effect of electrical stimulation of the suprahyoid muscles in brain-injured patients with dysphagia. Dysphagia. 2015; 30:423–9.
Article7. Pearson WG Jr, Langmore SE, Yu LB, Zumwalt AC. Structural analysis of muscles elevating the hyolaryngeal complex. Dysphagia. 2012; 27:445–51.
Article8. Huckabee ML, Cannito MP. Outcomes of swallowing rehabilitation in chronic brainstem dysphagia: a retrospective evaluation. Dysphagia. 1999; 14:93–109.
Article9. Cunningham DP, Basmajian JV. Electromyography of genioglossus and geniohyoid muscles during deglutition. Anat Rec. 1969; 165:401–9.
Article10. Dinardo LA, Travers JB. Hypoglossal neural activity during ingestion and rejection in the awake rat. J Neurophysiol. 1994; 72:1181–91.
Article11. Palmer PM, Luschei ES, Jaffe D, McCulloch TM. Contributions of individual muscles to the submental surface electromyogram during swallowing. J Speech Lang Hear Res. 1999; 42:1378–91.
Article12. Shaker R, Cook IJ, Dodds WJ, Hogan WJ. Pressure-flow dynamics of the oral phase of swallowing. Dysphagia. 1988; 3:79–84.
Article13. Clark HM, Henson PA, Barber WD, Stierwalt JA, Sherrill M. Relationships among subjective and objective measures of tongue strength and oral phase swallowing impairments. Am J Speech Lang Pathol. 2003; 12:40–50.
Article14. Kim HD, Choi JB, Yoo SJ, Chang MY, Lee SW, Park JS. Tongue-to-palate resistance training improves tongue strength and oropharyngeal swallowing function in subacute stroke survivors with dysphagia. J Oral Rehabil. 2017; 44:59–64.
Article15. Hirota N, Konaka K, Ono T, Tamine K, Kondo J, Hori K, et al. Reduced tongue pressure against the hard palate on the paralyzed side during swallowing predicts dysphagia in patients with acute stroke. Stroke. 2010; 41:2982–4.
Article16. Fujiwara S, Fujiu-Kurachi M, Hori K, Maeda Y, Ono T. Tongue pressure production and submental surface electromyogram activities during tongue-hold swallow with different holding positions and tongue length. Dysphagia. 2018; 33:403–13.
Article17. Oh JC. Effects of tongue-hold swallows on suprahyoid muscle activation according to the relative tongue protrusion length in the elderly individuals. Dysphagia. 2019; 34:382–90.
Article18. Oh JC. Effects of tongue-hold swallows on suprahyoid muscle activation according to the relative tongue protrusion length: a preliminary study. Springerplus. 2016; 5:1144.
Article19. Lee JH, Kim HS, Yun DH, Chon J, Han YJ, Yoo SD, et al. The relationship between tongue pressure and oral dysphagia in stroke patients. Ann Rehabil Med. 2016; 40:620–8.
Article20. Warnecke T, Im S, Kaiser C, Hamacher C, Oelenberg S, Dziewas R. Aspiration and dysphagia screening in acute stroke: the Gugging Swallowing Screen revisited. Eur J Neurol. 2017; 24:594–601.21. Chen PC, Chuang CH, Leong CP, Guo SE, Hsin YJ. Systematic review and meta-analysis of the diagnostic accuracy of the water swallow test for screening aspiration in stroke patients. J Adv Nurs. 2016; 72:2575–86.
Article22. Mulheren RW, Gonzalez-Fernandez M. Swallow screen associated with airway protection and dysphagia after acute stroke. Arch Phys Med Rehabil. 2019; 100:1289–93.
Article23. O’Neill PA. Swallowing and prevention of complications. Br Med Bull. 2000; 56:457–65.24. Yoon A, Zaghi S, Weitzman R, Ha S, Law CS, Guilleminault C, et al. Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017; 21:767–75.
Article25. Kim J, Oh BM, Kim JY, Lee GJ, Lee SA, Han TR. Validation of the videofluoroscopic dysphagia scale in various etiologies. Dysphagia. 2014; 29:438–43.
Article26. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article27. Goksuluk D, Korkmaz S, Zararsiz G, Karaagaoglu AE. easyROC: an interactive web-tool for ROC curve analysis using R language environment. R J. 2016; 8:213–30.
Article28. Keskool P, Warnpeurch L, Ongard S, Pitaksurachai P, Nujchanart N, Kerdnoppakhun J. The relationships among objective measures of tongue strength and risk of aspiration. Siriraj Med J. 2018; 70:302–9.29. Borggreven PA, Verdonck-de Leeuw I, Rinkel RN, Langendijk JA, Roos JC, David EF, et al. Swallowing after major surgery of the oral cavity or oropharynx: a prospective and longitudinal assessment of patients treated by microvascular soft tissue reconstruction. Head Neck. 2007; 29:638–47.
Article30. Pittman LJ, Bailey EF. Genioglossus and intrinsic electromyographic activities in impeded and unimpeded protrusion tasks. J Neurophysiol. 2009; 101:276–82.
Article31. Murakami K, Hori K, Minagi Y, Uehara F, Salazar SE, Ishihara S, et al. Coordination of tongue pressure production, hyoid movement, and suprahyoid muscle activity during squeezing of gels. Arch Oral Biol. 2020; 111:104631.
Article32. Taniguchi H, Tsukada T, Ootaki S, Yamada Y, Inoue M. Correspondence between food consistency and suprahyoid muscle activity, tongue pressure, and bolus transit times during the oropharyngeal phase of swallowing. J Appl Physiol (1985). 2008; 105:791–9.
Article33. Oguchi H, Watanabe T, Nakamura N, Watanabe S. Influence of tongue movements on masticatory efficiency. Dent Oral Craniofac Res. 2016; 2:1–6.
Article34. Robbins J, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007; 88:150–8.
Article35. Kahrilas PJ, Logemann JA, Lin S, Ergun GA. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992; 103:128–36.
Article36. Pouderoux P, Kahrilas PJ. Deglutitive tongue force modulation by volition, volume, and viscosity in humans. Gastroenterology. 1995; 108:1418–26.
Article37. Mori T, Wakabayashi H, Ogawa N, Fujishima I, Oshima F, Itoda M, et al. The mass of geniohyoid muscle is associated with maximum tongue pressure and tongue area in patients with sarcopenic dysphagia. J Nutr Health Aging. 2021; 25:356–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relations between posture and size of the tongue and dentoalveolar pattern
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Usefulness of Maximal Expiratory Pressure in Evaluating Dysphagia after Ischemic Stroke
- The Effect of Frenotomy on the Tongue Length, Motion, and Speech According to Age
- Effects of Tongue-Holding Maneuver Compared with Mendelsohn Maneuver on Swallowing Function in Stroke Patients