World J Mens Health.
2013 Aug;31(2):103-125.
Risks and Benefits of Late Onset Hypogonadism Treatment: An Expert Opinion
- Affiliations
-
- 1Endocrinology Unit, Medical Department, Azienda Usl, Maggiore-Bellaria Hospital, Bologna, Italy.
- 2Sexual Medicine and Andrology Unit, Department of Experimental, Clinical and Biomedical Sciences, University of Florence, Florence, Italy. m.maggi@dfc.unifi.it
Abstract
- Late-onset hypogonadism (LOH) is a syndromic condition that has a well-recognized association with sexual and reproductive failure. LOH is frequently associated with chronic conditions including cardiovascular diseases (CVD), obesity, osteoporosis, HIV infection, renal failure, and obstructive pulmonary diseases. Despite this evidence, in patients with these conditions, LOH is still only rarely investigated and testosterone replacement therapy (TRT) rarely considered. In this paper, we critically reviewed the available evidence on LOH treatment focusing on possible risks and benefits. Medical therapy of LOH should be individualized depending on the etiology of the disease and the patient's expectations. The fear of prostate cancer and the risk of erythrocytosis probably represent the main limitations of TRT in aging men. However, TRT in healthy older men in near physiological doses does not appear to incur serious adverse events, although regular monitoring of prostate-specific antigen and hematocrit levels is required. Available evidence also suggests that TRT might ameliorate central obesity and glycometabolic control in patients with metabolic syndrome and type 2 diabetes. In addition, TRT has been associated with an increase in bone mineral density in men with osteoporosis, with an improvement in lean body mass in subjects with human immunodeficiency virus infection or chronic obstructive pulmonary disease, as well as with peripheral oxygenation in patients with chronic kidney diseases. Despite this evidence, however, it should be recognized that the results of these trials were heterogeneous and limited by small sample sizes. Hence, further research is required regarding the long-term benefits and adverse effects of TRT in LOH.
MeSH Terms
-
Aging
Bone Density
Cardiovascular Diseases
Diabetes Mellitus
Erectile Dysfunction
Hematocrit
HIV
HIV Infections
Humans
Hypogonadism
Lung Diseases, Obstructive
Male
Obesity
Obesity, Abdominal
Osteoporosis
Polycythemia
Prostate
Prostate-Specific Antigen
Prostatic Neoplasms
Pulmonary Disease, Chronic Obstructive
Renal Insufficiency
Renal Insufficiency, Chronic
Testosterone
Prostate-Specific Antigen
Testosterone
Figure
Reference
-
1. Corona G, Rastrelli G, Forti G, Maggi M. Update in testosterone therapy for men. J Sex Med. 2011; 8:639–654.2. Corona G, Rastrelli G, Vignozzi L, Maggi M. Emerging medication for the treatment of male hypogonadism. Expert Opin Emerg Drugs. 2012; 17:239–259.
Article3. Andersson AM, Carlsen E, Petersen JH, Skakkebaek NE. Variation in levels of serum inhibin B, testosterone, estradiol, luteinizing hormone, follicle-stimulating hormone, and sex hormone-binding globulin in monthly samples from healthy men during a 17-month period: possible effects of seasons. J Clin Endocrinol Metab. 2003; 88:932–937.
Article4. Fellman J, Eriksson AW. Statistical analysis of the seasonal variation in demographic data. Hum Biol. 2000; 72:851–876.5. Herndon JG, Perachio AA, Turner JJ, Collins DC. Fluctuations in testosterone levels of male rhesus monkeys during copulatory activity. Physiol Behav. 1981; 26:525–528.
Article6. Buvat J, Maggi M, Guay A, Torres LO. Testosterone deficiency in men: systematic review and standard operating procedures for diagnosis and treatment. J Sex Med. 2013; 10:245–284.
Article7. Morelli A, Corona G, Filippi S, Ambrosini S, Forti G, Vignozzi L, et al. Which patients with sexual dysfunction are suitable for testosterone replacement therapy? J Endocrinol Invest. 2007; 30:880–888.
Article8. Mohr BA, Guay AT, O'Donnell AB, McKinlay JB. Normal, bound and nonbound testosterone levels in normally ageing men: results from the Massachusetts Male Ageing Study. Clin Endocrinol (Oxf). 2005; 62:64–73.
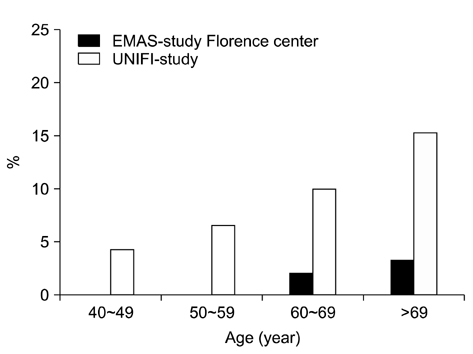
Article9. Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW, et al. European Male Aging Study Group. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab. 2008; 93:2737–2745.
Article10. Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, Gooren LJ, et al. Investigation, treatment and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA and ASA recommendations. Eur J Endocrinol. 2008; 159:507–514.
Article11. Petak SM, Nankin HR, Spark RF, Swerdloff RS, Rodriguez-Rigau LJ. American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients--2002 update. Endocr Pract. 2002; 8:440–456.
Article12. Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, et al. Task Force, Endocrine Society. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010; 95:2536–2559.
Article13. Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. EMAS Group. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010; 363:123–135.
Article14. Corona G, Rastrelli G, Maggi M. Diagnosis and treatment of late-onset hypogonadism. Best Pract Res Clin Endocrinol Metob. 2013; [in press].15. Corona G, Rastrelli G, Monami M, Saad F, Luconi M, Lucchese M, et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analysis. Eur J Endocrinol. 2013; 168:829–843.
Article16. Corona G, Baldi E, Maggi M. Androgen regulation of prostate cancer: where are we now? J Endocrinol Invest. 2011; 34:232–243.
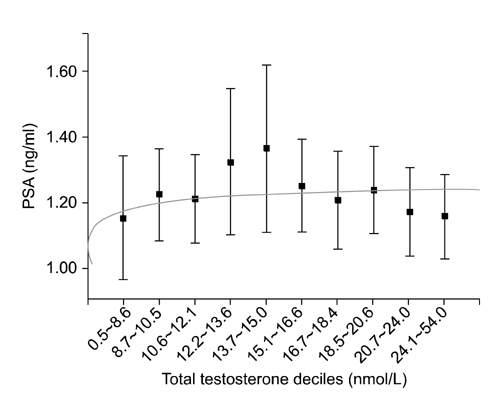
Article17. Corona G, Boddi V, Lotti F, Gacci M, Carini M, De Vita G, et al. The relationship of testosterone to prostate-specific antigen in men with sexual dysfunction. J Sex Med. 2010; 7:284–292.
Article18. Rastrelli G, Corona G, Vignozzi L, Maseroli E, Silverii A, Monami M, et al. Serum PSA as a predictor of testosterone deficiency. J Sex Med. 2013; [Epub ahead of print].
Article19. Bhasin S, Singh AB, Mac RP, Carter B, Lee MI, Cunningham GR. Managing the risks of prostate disease during testosterone replacement therapy in older men: recommendations for a standardized monitoring plan. J Androl. 2003; 24:299–311.
Article20. Kaufman JM, Graydon RJ. Androgen replacement after curative radical prostatectomy for prostate cancer in hypogonadal men. J Urol. 2004; 172:920–922.
Article21. Agarwal PK, Oefelein MG. Testosterone replacement therapy after primary treatment for prostate cancer. J Urol. 2005; 173:533–536.
Article22. Davila HH, Arison CN, Hall MK, Salup R, Lockhart JL, Carrion RE. Analysis of the psa response after testosterone supplemenatation in patients who have previously received management for their localized prostate cancer. J Urol. 2008; 179:Suppl 4. 428. abstract 1247.
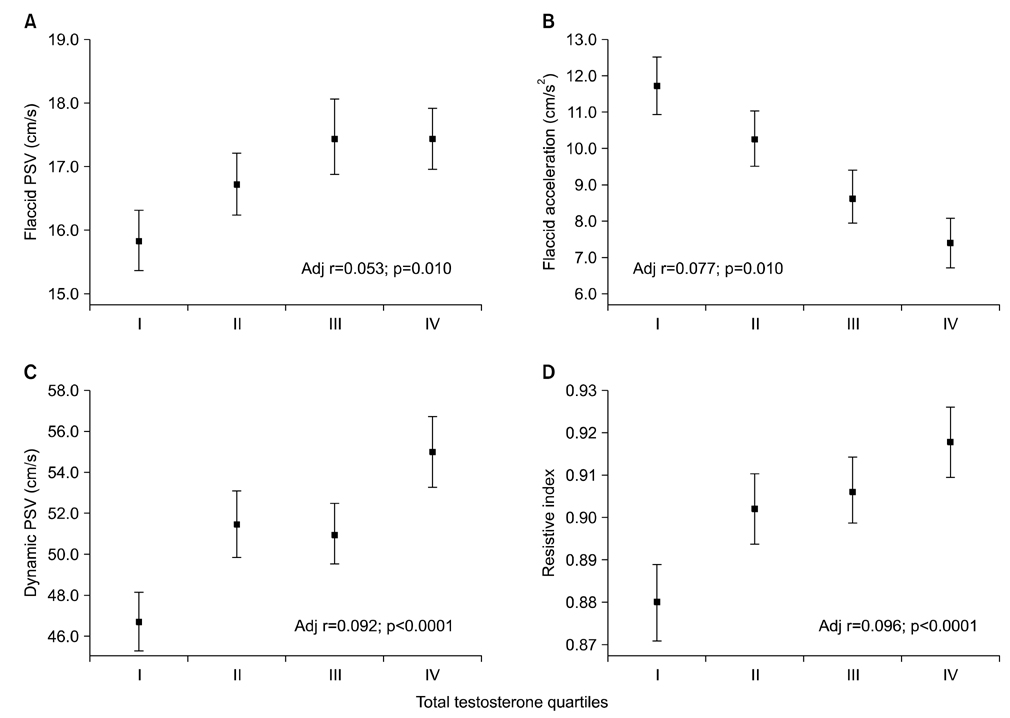
Article23. Nabulsi O, Tal R, Gotto G, Narus J, Goldenberg L, Mulhall JP. Outcomes analysis of testosterone supplementation in hypogonadal men following radical prostatectomy. J Urol. 2008; 179:Suppl 4. 406. abstract 1244.
Article24. Khera M, Grober ED, Najari B, Colen JS, Mohamed O, Lamb DJ, et al. Testosterone replacement therapy following radical prostatectomy. J Sex Med. 2009; 6:1165–1170.
Article25. Leibowitz RL, Dorff TB, Tucker S, Symanowski J, Vogelzang NJ. Testosterone replacement in prostate cancer survivors with hypogonadal symptoms. BJU Int. 2010; 105:1397–1401.
Article26. Morales A, Black AM, Emerson LE. Testosterone administration to men with testosterone deficiency syndrome after external beam radiotherapy for localized prostate cancer: preliminary observations. BJU Int. 2009; 103:62–64.
Article27. Sarosdy MF. Testosterone replacement for hypogonadism after treatment of early prostate cancer with brachytherapy. Cancer. 2007; 109:536–541.
Article28. Morgentaler A, Lipshultz LI, Bennett R, Sweeney M, Avila D Jr, Khera M. Testosterone therapy in men with untreated prostate cancer. J Urol. 2011; 185:1256–1260.
Article29. Pastuszak AW, Pearlman AM, Godoy G, Miles BJ, Lipshultz LI, Khera M. Testosterone replacement therapy in the setting of prostate cancer treated with radiation. Int J Impot Res. 2013; 25:24–28.
Article30. Fibbi B, Penna G, Morelli A, Adorini L, Maggi M. Chronic inflammation in the pathogenesis of benign prostatic hyperplasia. Int J Androl. 2010; 33:475–488.
Article31. Vignozzi L, Gacci M, Cellai I, Morelli A, Maneschi E, Comeglio P, et al. PDE5 inhibitors blunt inflammation in human BPH: A potential mechanism of action for PDE5 inhibitors in LUTS. Prostate. 2013; [Epub ahead of print].
Article32. Vignozzi L, Gacci M, Cellai I, Santi R, Corona G, Morelli A, et al. Fat boosts, while androgen receptor activation counteracts, BPH-associated prostate inflammation. Prostate. 2013; 73:789–800.
Article33. Lotti F, Corona G, Degli Innocenti S, Filimberti E, Scognamiglio V, Vignozzi L, et al. Seminal, ultrasound and psychobiological parameters correlate with metabolic syndrome in male members of infertile couples. Andrology. 2013; 1:229–239.
Article34. Gacci M, Vignozzi L, Sebastianelli A, Salvi M, Giannessi C, De Nunzio C, et al. Metabolic syndrome and lower urinary tract symptoms: the role of inflammation. Prostate Cancer Prostatic Dis. 2013; 16:101–106.
Article35. Vignozzi L, Morelli A, Sarchielli E, Comeglio P, Filippi S, Cellai I, et al. Testosterone protects from metabolic syndrome-associated prostate inflammation: an experimental study in rabbit. J Endocrinol. 2012; 212:71–84.
Article36. Morelli A, Comeglio P, Filippi S, Sarchielli E, Vignozzi L, Maneschi E, et al. Mechanism of action of phosphodiesterase type 5 inhibition in metabolic syndrome-associated prostate alterations: an experimental study in the rabbit. Prostate. 2013; 73:428–441.
Article37. Morelli A, Comeglio P, Filippi S, Sarchielli E, Cellai I, Vignozzi L, et al. Testosterone and farnesoid X receptor agonist INT-747 counteract high fat diet-induced bladder alterations in a rabbit model of metabolic syndrome. J Steroid Biochem Mol Biol. 2012; 132:80–92.
Article38. Vignozzi L, Morelli A, Filippi S, Comeglio P, Chavalmane AK, Marchetta M, et al. Farnesoid X receptor activation improves erectile function in animal models of metabolic syndrome and diabetes. J Sex Med. 2011; 8:57–77.
Article39. Filippi S, Vignozzi L, Morelli A, Chavalmane AK, Sarchielli E, Fibbi B, et al. Testosterone partially ameliorates metabolic profile and erectile responsiveness to PDE5 inhibitors in an animal model of male metabolic syndrome. J Sex Med. 2009; 6:3274–3288.
Article40. Vignozzi L, Cellai I, Santi R, Lombardelli L, Morelli A, Comeglio P, et al. Antiinflammatory effect of androgen receptor activation in human benign prostatic hyperplasia cells. J Endocrinol. 2012; 214:31–43.
Article41. Shigehara K, Namiki M. Late-onset hypogonadism syndrome and lower urinary tract symptoms. Korean J Urol. 2011; 52:657–663.
Article42. Pearl JA, Berhanu D, François N, Masson P, Zargaroff S, Cashy J, et al. Testosterone supplementation does not worsen lower urinary tract symptoms. J Urol. 2013; [Epub ahead of print].
Article43. Guo W, Bachman E, Li M, Roy CN, Blusztajn J, Wong S, et al. Testosterone administration inhibits hepcidin transcription and is associated with increased iron incorporation into red blood cells. Aging Cell. 2013; 12:280–291.
Article44. Calof OM, Singh AB, Lee ML, Kenny AM, Urban RJ, Tenover JL, et al. Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci. 2005; 60:1451–1457.
Article45. Fernández-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ, et al. Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2010; 95:2560–2575.46. Hoyos CM, Killick R, Yee BJ, Grunstein RR, Liu PY. Effects of testosterone therapy on sleep and breathing in obese men with severe obstructive sleep apnoea: a randomized placebo-controlled trial. Clin Endocrinol (Oxf). 2012; 77:599–607.
Article47. Snyder PJ, Peachey H, Hannoush P, Berlin JA, Loh L, Lenrow DA, et al. Effect of testosterone treatment on body composition and muscle strength in men over 65 years of age. J Clin Endocrinol Metab. 1999; 84:2647–2653.
Article48. Kamischke A, Nieschlag E. Analysis of medical treatment of male infertility. Hum Reprod. 1999; 14:Suppl 1. 1–23.
Article49. Bang JK, Lim JJ, Choi J, Won HJ, Yoon TK, Hong JY, et al. Reversible infertility associated with testosterone therapy for symptomatic hypogonadism in infertile couple. Yonsei Med J. 2013; 54:702–706.
Article50. Burger HG, de Kretser DM, Hudson B, Wilson JD. Effects of preceding androgen therapy on testicular response to human pituitary gonadotropin in hypogonadotropic hypogonadism: a study of three patients. Fertil Steril. 1981; 35:64–68.51. Raivio T, Falardeau J, Dwyer A, Quinton R, Hayes FJ, Hughes VA, et al. Reversal of idiopathic hypogonadotropic hypogonadism. N Engl J Med. 2007; 357:863–873.
Article52. Liu PY, Baker HW, Jayadev V, Zacharin M, Conway AJ, Handelsman DJ. Induction of spermatogenesis and fertility during gonadotropin treatment of gonadotropin-deficient infertile men: predictors of fertility outcome. J Clin Endocrinol Metab. 2009; 94:801–808.
Article53. O'Connor DB, Corona G, Forti G, Tajar A, Lee DM, Finn JD, et al. Assessment of sexual health in aging men in Europe: development and validation of the European Male Ageing Study sexual function questionnaire. J Sex Med. 2008; 5:1374–1385.54. Corona G, Mannucci E, Ricca V, Lotti F, Boddi V, Bandini E, et al. The age-related decline of testosterone is associated with different specific symptoms and signs in patients with sexual dysfunction. Int J Androl. 2009; 32:720–728.
Article55. Corona G, Rastrelli G, Vignozzi L, Mannucci E, Maggi M. How to recognize late-onset hypogonadism in men with sexual dysfunction. Asian J Androl. 2012; 14:251–259.
Article56. Corona G, Rastrelli G, Ricca V, Jannini EA, Vignozzi L, Monami M, et al. Risk factors associated with primary and secondary reduced libido in male patients with sexual dysfunction. J Sex Med. 2013; 10:1074–1089.
Article57. Vignozzi L, Corona G, Petrone L, Filippi S, Morelli AM, Forti G, et al. Testosterone and sexual activity. J Endocrinol Invest. 2005; 28:3 Suppl. 39–44.58. Corona G, Maggi M. The role of testosterone in erectile dysfunction. Nat Rev Urol. 2010; 7:46–56.
Article59. Isidori AM, Giannetta E, Gianfrilli D, Greco EA, Bonifacio V, Aversa A, et al. Effects of testosterone on sexual function in men: results of a meta-analysis. Clin Endocrinol (Oxf). 2005; 63:381–389.
Article60. Boloña ER, Uraga MV, Haddad RM, Tracz MJ, Sideras K, Kennedy CC, et al. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc. 2007; 82:20–28.
Article61. Jain P, Rademaker AW, McVary KT. Testosterone supplementation for erectile dysfunction: results of a metaanalysis. J Urol. 2000; 164:371–375.
Article62. Corona G, Mondaini N, Ungar A, Razzoli E, Rossi A, Fusco F. Phosphodiesterase type 5 (PDE5) inhibitors in erectile dysfunction: the proper drug for the proper patient. J Sex Med. 2011; 8:3418–3432.
Article63. Spitzer M, Basaria S, Travison TG, Bhasin S. In response. Effects of testosterone replacement on response to sildenafil citrate. Ann Intern Med. 2013; 158:570–571.64. Aversa A, Jannini EA, Maggi M, Lenzi A. Effects of testosterone replacement on response to sildenafil citrate. Ann Intern Med. 2013; 158:569–570.
Article65. Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011; 34:41–48.
Article66. Corona G, Jannini EA, Vignozzi L, Rastrelli G, Maggi M. The hormonal control of ejaculation. Nat Rev Urol. 2012; 9:508–519.
Article67. Corona G, Mannucci E, Petrone L, Fisher AD, Balercia G, De Scisciolo G, et al. Psychobiological correlates of delayed ejaculation in male patients with sexual dysfunctions. J Androl. 2006; 27:453–458.
Article68. Corona G, Rastrelli G, Vignozzi L, Mannucci E, Maggi M. Testosterone, cardiovascular disease and the metabolic syndrome. Best Pract Res Clin Endocrinol Metab. 2011; 25:337–353.
Article69. Corona G, Monami M, Boddi V, Cameron-Smith M, Fisher AD, de Vita G, et al. Low testosterone is associated with an increased risk of MACE lethality in subjects with erectile dysfunction. J Sex Med. 2010; 7:1557–1564.
Article70. Corona G, Rastrelli G, Monami M, Melani C, Balzi D, Sforza A, et al. Body mass index regulates hypogonadism-associated CV risk: results from a cohort of subjects with erectile dysfunction. J Sex Med. 2011; 8:2098–2105.
Article71. Corona G, Rastrelli G, Balercia G, Sforza A, Forti G, Maggi M. Testosterone and cardiovascular risk in patients with erectile dysfunction. J Endocrinol Invest. 2012; 35:809–816.72. Corona G, Rastrelli G, Monami M, Guay A, Buvat J, Sforza A, et al. Hypogonadism as a risk factor for cardiovascular mortality in men: a meta-analytic study. Eur J Endocrinol. 2011; 165:687–701.
Article73. Araujo AB, Dixon JM, Suarez EA, Murad MH, Guey LT, Wittert GA. Clinical review: Endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011; 96:3007–3019.74. Ruige JB, Mahmoud AM, De Bacquer D, Kaufman JM. Endogenous testosterone and cardiovascular disease in healthy men: a meta-analysis. Heart. 2011; 97:870–875.
Article75. Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM. Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab. 2012; 97:2050–2058.
Article76. Muraleedharan V, Marsh H, Channer KS, Jones HT. Long-term testosterone replacement improves survival in men with type 2 diabetes and hypogonadism endocr rev. Endocr Rev. 2011; 32:OR35-2.77. Fernández-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ, et al. Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2010; 95:2560–2575.78. Haddad RM, Kennedy CC, Caples SM, Tracz MJ, Boloña ER, Sideras K, et al. Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc. 2007; 82:29–39.
Article79. Calof OM, Singh AB, Lee ML, Kenny AM, Urban RJ, Tenover JL, et al. Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci. 2005; 60:1451–1457.80. Xu L, Freeman G, Cowling BJ, Schooling CM. Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013; 11:108.
Article81. Toma M, McAlister FA, Coglianese EE, Vidi V, Vasaiwala S, Bakal JA, et al. Testosterone supplementation in heart failure: a meta-analysis. Circ Heart Fail. 2012; 5:315–321.82. Corona G, Rastrelli G, Balercia G, Lotti F, Sforza A, Monami M, et al. Hormonal association and sexual dysfunction in patients with impaired fasting glucose: a cross-sectional and longitudinal study. J Sex Med. 2012; 9:1669–1680.
Article83. Corona G, Rastrelli G, Silverii A, Monami M, Sforza A, Forti G, et al. The identification of prediabetes condition with ARIC algorithm predicts long-term CV events in patients with erectile dysfunction. J Sex Med. 2013; 10:1114–1123.
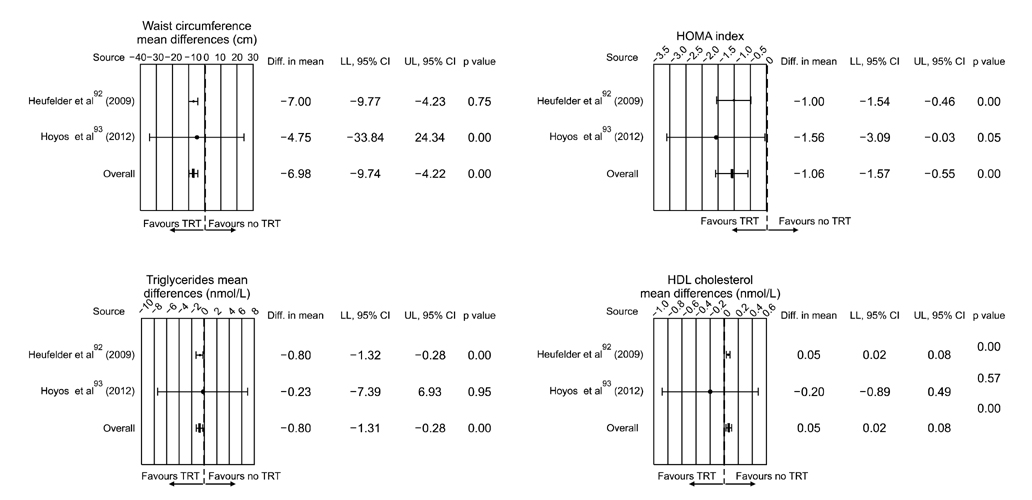
Article84. Corona G, Rastrelli G, Morelli A, Vignozzi L, Mannucci E, Maggi M. Hypogonadism and metabolic syndrome. J Endocrinol Invest. 2011; 34:557–567.85. Corona G, Monami M, Rastrelli G, Aversa A, Sforza A, Lenzi A, et al. Type 2 diabetes mellitus and testosterone: a meta-analysis study. Int J Androl. 2011; 34:528–540.
Article86. Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, et al. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med. 2011; 8:272–283.
Article87. Corona G, Mannucci E, Forti G, Maggi M. Following the common association between testosterone deficiency and diabetes mellitus, can testosterone be regarded as a new therapy for diabetes? Int J Androl. 2009; 32:431–441.
Article88. Saad F, Aversa A, Isidori AM, Zafalon L, Zitzmann M, Gooren L. Onset of effects of testosterone treatment and time span until maximum effects are achieved. Eur J Endocrinol. 2011; 165:675–685.
Article89. Zitzmann M, Mattern A, Hanisch J, Gooren L, Jones H, Maggi M. IPASS: a study on the tolerability and effectiveness of injectable testosterone undecanoate for the treatment of male hypogonadism in a worldwide sample of 1,438 men. J Sex Med. 2013; 10:579–588.
Article90. Saad F, Haider A, Doros G, Traish A. Long-term treatment of hypogonadal men with testosterone produces substantial and sustained weight loss. Obesity (Silver Spring). 2013; [Epub ahead of print].
Article91. Camacho EM, Huhtaniemi IT, O'Neill TW, Finn JD, Pye SR, Lee DM, et al. EMAS Group. Age-associated changes in hypothalamic-pituitary-testicular function in middle-aged and older men are modified by weight change and lifestyle factors: longitudinal results from the European Male Ageing Study. Eur J Endocrinol. 2013; 168:445–455.
Article92. Heufelder AE, Saad F, Bunck MC, Gooren L. Fifty-two-week treatment with diet and exercise plus transdermal testosterone reverses the metabolic syndrome and improves glycemic control in men with newly diagnosed type 2 diabetes and subnormal plasma testosterone. J Androl. 2009; 30:726–733.
Article93. Hoyos CM, Yee BJ, Phillips CL, Machan EA, Grunstein RR, Liu PY. Body compositional and cardiometabolic effects of testosterone therapy in obese men with severe obstructive sleep apnoea: a randomised placebo-controlled trial. Eur J Endocrinol. 2012; 167:531–541.
Article94. Tracz MJ, Sideras K, Boloña ER, Haddad RM, Kennedy CC, Uraga MV, et al. Testosterone use in men and its effects on bone health. A systematic review and meta-analysis of randomized placebo-controlled trials. J Clin Endocrinol Metab. 2006; 91:2011–2016.
Article95. Isidori AM, Giannetta E, Greco EA, Gianfrilli D, Bonifacio V, Isidori A, et al. Effects of testosterone on body composition, bone metabolism and serum lipid profile in middle-aged men: a meta-analysis. Clin Endocrinol (Oxf). 2005; 63:280–293.
Article96. MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med. 2008; 148:197–213.
Article97. Hill L, Lee KC. Pharmacotherapy considerations in patients with HIV and psychiatric disorders: focus on antidepressants and antipsychotics. Ann Pharmacother. 2013; 47:75–89.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Manual of 2008 ISA, ISSAM, EAU, EAA and ASA Recommendations: Investigation, Treatment and Monitoring of Late-onset Hypogonadism in Males
- Management of Late-onset Hypogonadism
- A Study on Late-onset of Hypogonadism, Erectile Dysfunction, Depression, and Quality of Life among Middle-aged Male Worker
- Diagnosis and Treatment of Sexual Dysfunctions in Late-Onset Hypogonadism
- Physical Activity and Exercise for Men with Late Onset Hypogonadism