Lab Anim Res.
2016 Mar;32(1):8-15. 10.5625/lar.2016.32.1.8.
Cardiopulmonary effects of thiopental versus propofol as an induction agent prior to isoflurane anesthesia in chair trained rhesus macaques (Macaca mulatta)
- Affiliations
-
- 1Transplantation Research Institute, Medical Research Center, Department of Medicine, Seoul National University College of Medicine, Seoul, Korea. jaeil@snu.ac.kr
- 2Department of Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2312149
- DOI: http://doi.org/10.5625/lar.2016.32.1.8
Abstract
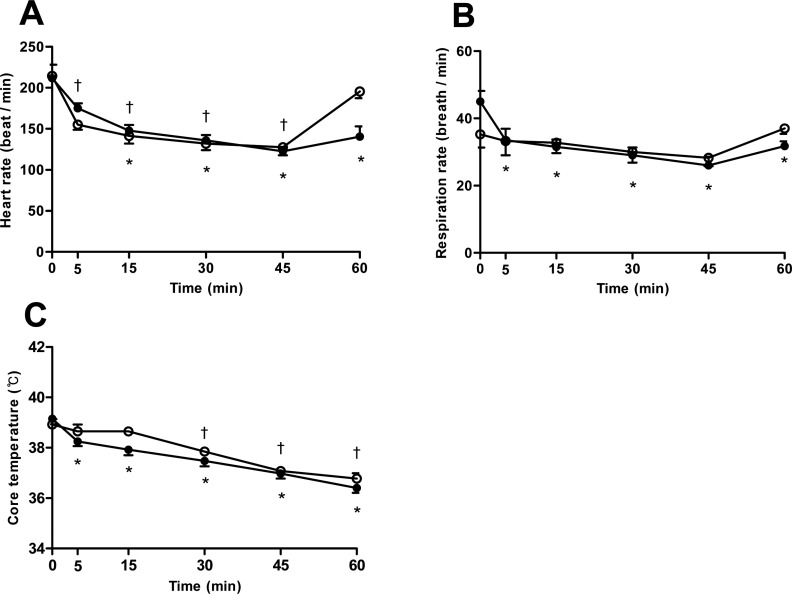
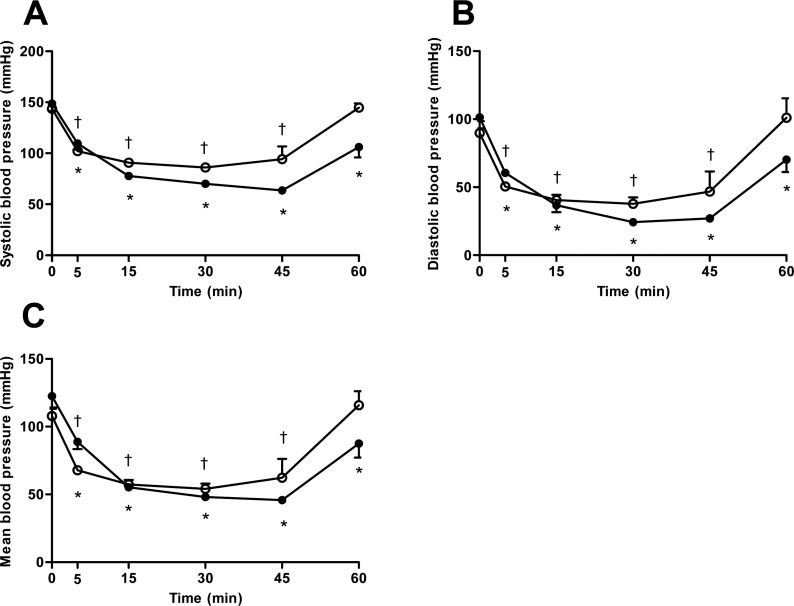
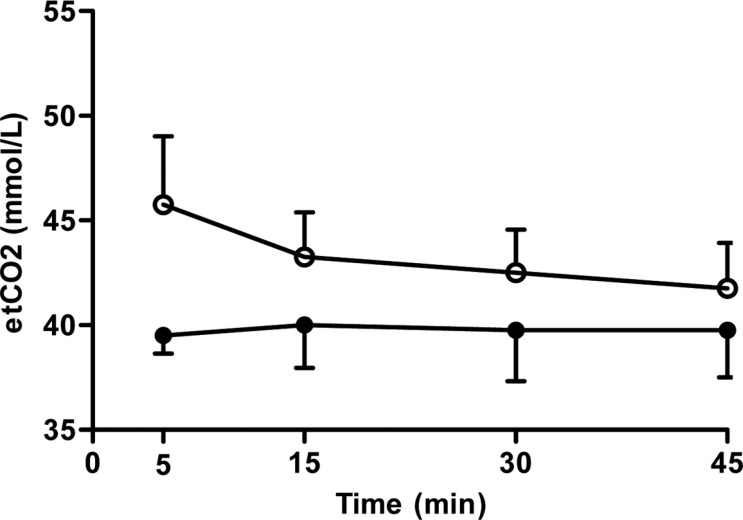
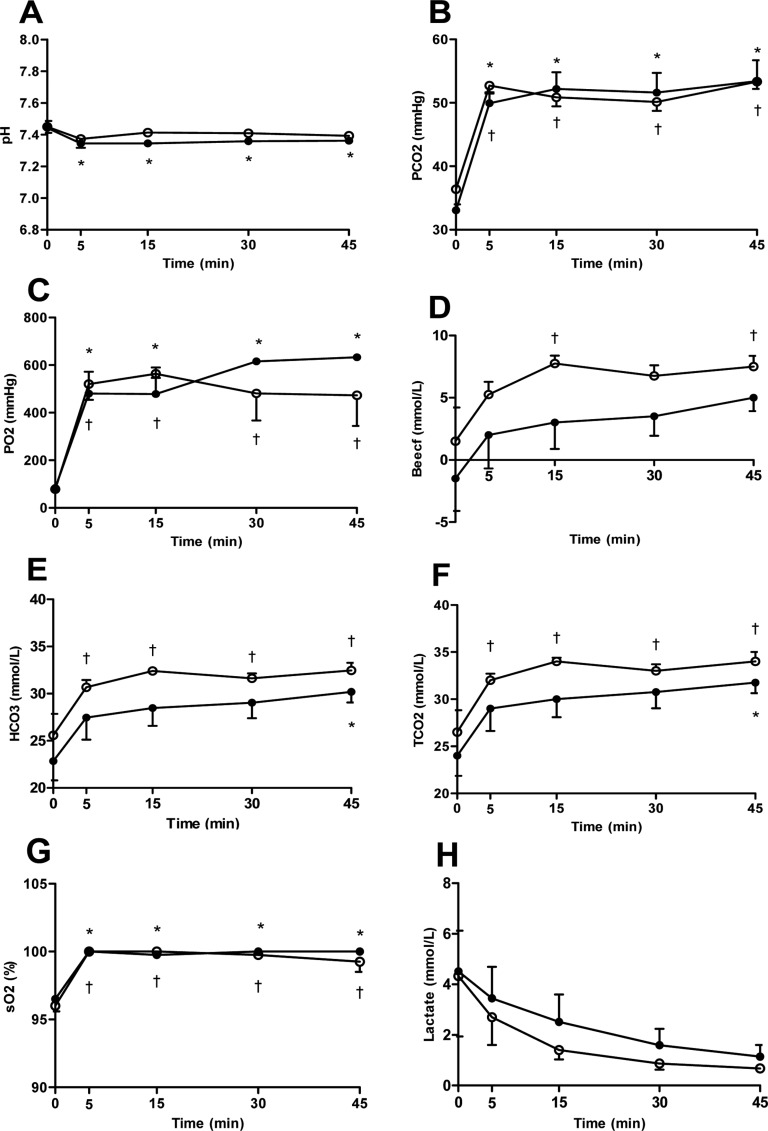
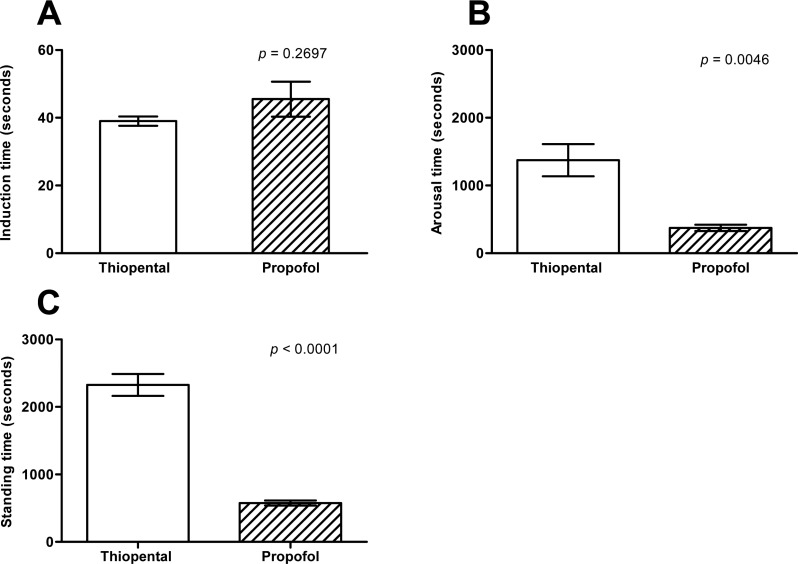
- The purpose of this study was to evaluate the effects of thiopental versus propofol on cardiopulmonary functions, when used as an induction agent prior to isoflurane anesthesia in rhesus monkeys. Eight healthy rhesus monkeys weighing 3.72 to 5.7 kg, 4-5 years old, were used in the study. Anesthesia was induced with thiopental or propofol intravenous injection, and then maintained with isoflurane in oxygen for 45 minutes. Cardiopulmonary measurements were obtained before and 5, 15, 30, 45, and 60 minutes after induction. The induction doses of thiopental and propofol were 19.41±0.54 and 9.33±1.02 mg/kg, respectively. In both groups, the values of heart rate, respiratory rate, temperature, systolic blood pressure, mean blood pressure, diastolic blood pressure, pH, and lactate were decreased, while the values of partial pressure of carbon dioxide, partial pressure of oxygen, total carbon dioxide, bicarbonate, oxygen saturation, and base excess in the extracellular fluid were increased, as compared with baseline. Systolic blood pressure was significantly lower in thiopental group compare to propofol group. Induction time was very short in both agents but not revealed a significant difference between both groups. However, recovery time was extremely faster in the propofol group. Our results demonstrated that propofol provides a minor suppression in systolic arterial blood pressure than thiopental sodium. In addition, propofol have a fast recovery effect from the anesthesia as well. Furthermore, it is suggested that thiopental sodium could also be used to induce anesthesia instead of propofol, despite slight more suppression of cardiopulmonary function compared to thiopental sodium.
Keyword
MeSH Terms
Figure
Reference
-
1. Bennett JS, Gossett KA, McCarthy MP, Simpson ED. Effects of ketamine hydrochloride on serum biochemical and hematologic variables in rhesus monkeys (Macaca mulatta). Vet Clin Pathol. 1992; 21(1):15–18. PMID: 12671786.2. Lee JI, Hong SH, Lee SJ, Kim YS, Kim MC. Immobilization with ketamine HCl and tiletamine-zolazepam in cynomolgus monkeys. J Vet Sci. 2003; 4(2):187–191. PMID: 14610374.
Article3. Davy CW, Trennery PN, Edmunds JG, Altman JF, Eichler DA. Local myotoxicity of ketamine hydrochloride in the marmoset. Lab Anim. 1987; 21(1):60–67. PMID: 3104668.
Article4. Settle TL, Rico PJ, Lugo-Roman LA. The effect of daily repeated sedation using ketamine or ketamine combined with medetomidine on physiology and anesthetic characteristics in rhesus macaques. J Med Primatol. 2010; 39(1):50–57. PMID: 19912466.
Article5. Springer DA, Baker KC. Effect of ketamine anesthesia on daily food intake in Macaca mulatta and Cercopithecus aethiops. Am J Primatol. 2007; 69(10):1080–1092. PMID: 17330308.6. Brainard BM, Campbell VL, Drobatz KJ, Perkowski SZ. The effects of surgery and anesthesia on blood magnesium and calcium concentrations in canine and feline patients. Vet Anaesth Analg. 2007; 34(2):89–98. PMID: 17316389.
Article7. Chang J, Kim S, Jung J, Lee H, Chang D, Lee Y, Lee I, Yoon J, Choi M. Evaluation of the effects of thiopental, propofol, and etomidate on glomerular filtration rate measured by the use of dynamic computed tomography in dogs. Am J Vet Res. 2011; 72(1):146–151. PMID: 21194347.
Article8. Enouri SS, Kerr CL, McDonell WN, Dyson DH. Cardiopulmonary effects of anesthetic induction with thiopental, propofol, or a combination of ketamine hydrochloride and diazepam in dogs sedated with a combination of medetomidine and hydromorphone. Am J Vet Res. 2008; 69(5):586–595. PMID: 18447788.
Article9. Kojima K, Nishimura R, Mutoh T, Hong SH, Mochizuki M, Sasaki N. Effects of medetomidine-midazolam, acepromazinebutorphanol, and midazolam-butorphanol on induction dose of thiopental and propofol and on cardiopulmonary changes in dogs. Am J Vet Res. 2002; 63(12):1671–1679. PMID: 12492281.
Article10. Turner DM, Ilkiw JE. Cardiovascular and respiratory effects of three rapidly acting barbiturates in dogs. Am J Vet Res. 1990; 51(4):598–604. PMID: 2327623.11. Foster A, Zeller W, Pfannkuche HJ. Effect of thiopental, saffan, and propofol anesthesia on cardiovascular parameters and bronchial smooth muscle in the rhesus monkey. Lab Anim Sci. 1996; 46(3):327–334. PMID: 8799941.12. Fayyaz S, Kerr CL, Dyson DH, Mirakhur KK. The cardiopulmonary effects of anesthetic induction with isoflurane, ketamine-diazepam or propofol-diazepam in the hypovolemic dog. Vet Anaesth Analg. 2009; 36(2):110–123. PMID: 19239649.
Article13. Aeschbacher G, Webb AI. Propofol in rabbits. 2. Long-term anesthesia. Lab Anim Sci. 1993; 43(4):328–335. PMID: 8231090.14. Quandt JE, Robinson EP, Rivers WJ, Raffe MR. Cardiorespiratory and anesthetic effects of propofol and thiopental in dogs. Am J Vet Res. 1998; 59(9):1137–1143. PMID: 9736392.15. Lee JI, Shin JS, Lee JE, Jung WY, Lee G, Kim MS, Park CG, Kim SJ. Changes of N/L ratio and cortisol levels associated with experimental training in untrained rhesus macaques. J Med Primatol. 2013; 42(1):10–14. PMID: 23131089.
Article16. Enlund M, Andersson J, Hartvig P, Valtysson J, Wiklund L. Cerebral normoxia in the rhesus monkey during isoflurane- or propofol-induced hypotension and hypocapnia, despite disparate blood-flow patterns. A positron emission tomography study. Acta Anaesthesiol Scand. 1997; 41(8):1002–1010. PMID: 9311398.17. Portier KG, Broillet A, Rioufol G, Lepage OM, Depecker M, Taborik F, Tranquart F, Contamin H. A novel minimal invasive closed chest myocardial ischaemia reperfusion model in rhesus monkeys (Macaca mulatta): improved stability of cardiorespiratory parameters. Lab Anim. 2012; 46(2):129–135. PMID: 22334875.
Article18. Mutoh T, Nishimura R, Kim HY, Matsunaga S, Sasaki N. Cardiopulmonary effects of sevoflurane, compared with halothane, enflurane, and isoflurane, in dogs. Am J Vet Res. 1997; 58(8):885–890. PMID: 9256976.19. Fanton JW, Zarr SR, Ewert DL, Woods RW, Koenig SC. Cardiovascular responses to propofol and etomidate in long-term instrumented rhesus monkeys (Macaca mulatta). Comp Med. 2000; 50(3):303–308. PMID: 10894497.20. Ator NA. Selectivity in generalization to GABAergic drugs in midazolam-trained baboons. Pharmacol Biochem Behav. 2003; 75(2):435–445. PMID: 12873636.
Article21. Martin LD, Dissen GA, McPike MJ, Brambrink AM. Effects of anesthesia with isoflurane, ketamine, or propofol on physiologic parameters in neonatal rhesus macaques (Macaca mulatta). J Am Assoc Lab Anim Sci. 2014; 53(3):290–300. PMID: 24827572.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Thiopental Sodium and Propofol as Anesthetic Induction Agents for Hypnotic Time
- A Comparison of the Effect of Propofol and Thiopental on the Hemodynamic parameters in Valvular Replacement Surgery
- Effects of Propofol and Thiopental Sodium on the Intracranial Pressure under Halothane or Isoflurane Anesthesia in the Rabbit
- Effects of propofol and thiopental sodium on the intracranial pressure under halothane or isoflurane anesthesia in the rabbit
- Comparing the effects of thiopental and propofol administration on the cardiovascular response as an induction agent during desflurane anesthesia