Korean J Urol.
2008 Sep;49(9):818-825.
The Prevalence and Risk Factors of Nocturia for Males Participating in a Prostate Examination Survey
- Affiliations
-
- 1Department of Urology, College of Medicine, Hanyang University, Seoul, Korea. harabugi@hanyang.ac.kr
- 2Korea Prostate Health Council, Seoul, Korea.
Abstract
-
PURPOSE: Elderly men are often troubled by lower urinary tract symptoms (LUTS), including frequency, urgency, incontinence and nocturia. Especially, nocturia is one of the frequently complained about urologic symptoms and this can be combined with sleep disorders. We investigated the prevalence and risk factors for nocturia in males who participated in a prostate examination survey.
MATERIALS AND METHODS
A total of 7,299 men participated in a prostate examination survey from March 2003 to December 2006; these men were given an International Prostate Symptom Score(IPSS) and they underwent transrectal ultrasonography of the prostate. The prevalence of nocturia and its associated factors, which included age, the IPSS severity, the prostate volume and the place of residence, were evaluated.
RESULTS
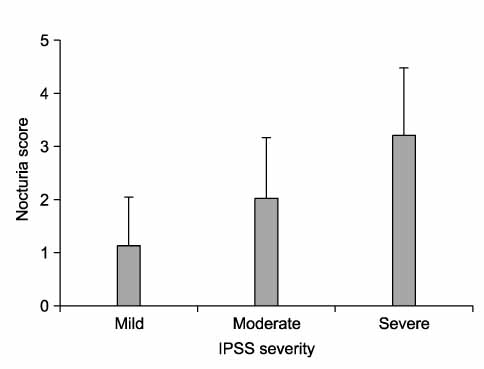
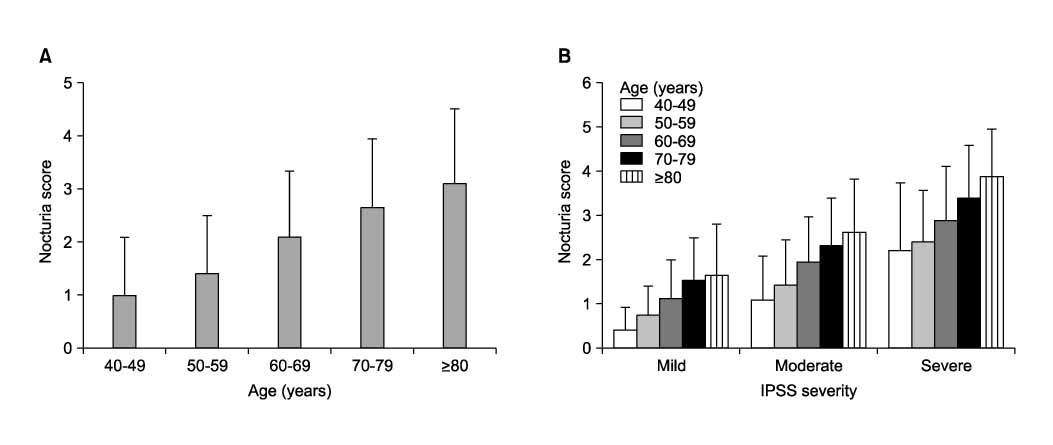
Among the men who were evaluated, 23.4% reported voiding once per night and 68% reported voiding twice or more per night. The severe IPSS group revealed a significantly higher nocturia score compared to the mild and moderate IPSS group. While the nocturia score and the other LUTS score increased significantly with age, only the nocturia score increased significantly with age in each of the IPSS severity groups. The nocturia score increased significantly with a prostate volume >or=30g. Men living in Seoul showed a significantly lower nocturia score than that for men living in other areas. Multiple logistic regression analysis also indicated that an older age, a severe IPSS score, the country of residence were the independent risk factors. Multiple regression analysis revealed the nocturia score to have the highest correlation with the quality of life.
CONCLUSIONS
For Korean males, the prevalence of nocturia >or=2 is 68% and the incidence of nocturia increased significantly according to age, the IPSS severity, the prostate volume and the place of residence.
MeSH Terms
Figure
Reference
-
1. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006. 50:1306–1314.2. Hald T, Horn T. The human urinary bladder in ageing. Br J Urol. 1998. 82:Suppl 1. 59–64.3. Barry MJ, Fowler FJ Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The measurement committee of the American Urological Association. J Urol. 1992. 148:1549–1557.4. Cho KS, Jo MK, Lim D, Son H, Park SK, Yoo KY, et al. Epidemiologic survey using International Prostate Symptom Score (I-PSS) of lower urinary tract symptoms (LUTS) in elderly men above 40 years old in Seoul area. Korean J Urol. 2001. 42:840–848.5. Jennum P. Sleep and nocturia. BJU Int. 2002. 90:Suppl 3. 21–24.6. Stewart RB, Moore MT, May FE, Marks RG, Hale WE. Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc. 1992. 40:1217–1220.7. Choo MS, Ku JH, Park CH, Lee YS, Lee KS, Lee JG, et al. Prevalence of nocturia in a Korean population aged 40 to 89 years. Neurourol Urodyn. 2008. 27:60–64.8. Kim ET, Lee SI, Lee KS. The etiology and classification of nocturia in adults. Korean J Urol. 2001. 42:1075–1079.9. Asplund R. Mortality in the elderly in relation to nocturnal micturition. BJU Int. 1999. 84:297–301.10. Liew LC, Tiong HY, Wong ML, Png DC, Tan JK. A population study of nocturia in Singapore. BJU Int. 2006. 97:109–112.11. Schatzl G, Temml C, Schmidbauer J, Dolezal B, Haidinger G, Madersbacher S. Cross-sectional study of nocturia in both sexes: analysis of a voluntary health screening project. Urology. 2000. 56:71–75.12. Van Dijk L, Kooij DG, Schellevis FG. Nocturia in the dutch adult population. BJU Int. 2002. 90:644–648.13. Jackson S. Lower urinary tract symptoms and nocturia in men and women: prevalence, aetiology and diagnosis. BJU Int. 1999. 84:Suppl 1. 5–8.14. Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E. The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int. 2003. 92:948–954.15. Tikkinen KA, Tammela TL, Huhtala H, Auvinen A. Is nocturia equally common among men and women? A population based study in Finland. J Urol. 2006. 175:596–560.16. Asplund R. The nocturnal polyuria syndrome (NPS). Gen Pharmacol. 1995. 26:1203–1209.17. Margel D, Lifshitz D, Brown N, Lask D, Livne PM, Tal R. Predictors of nocturia quality of life before and shortly after prostatectomy. Urology. 2007. 70:493–497.18. Chute CG, Panser LA, Girman CJ, Oesterling JE, Guess HA, Jacobsen SJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993. 150:85–89.19. Pinnock C, Marshall VR. Troublesome lower urinary tract symptoms in the community: a prevalence study. Med J Aust. 1997. 167:72–75.20. Weiss JP, Blaivas JG, Stember DS, Brooks MM. Nocturia in adults: etiology and classification. Neurourol Urodyn. 1998. 17:467–472.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post Treatment Change of Nocturia in Patients with Benign Prostatic Hyperplasia
- Analyzing the Factors Associated With Nocturia in Older People in the United States
- Prevalence and Correlates of Nocturia in Community-dwelling Older Men: Results from the Korean Longitudinal Study on Health and Aging
- A Population-Based Study of Factors Associated With Nocturia in Reproductive-Aged Turkish Women
- Prevalence and Predictors of Nocturia in Patients with Obstructive Sleep Apnea Syndrome