Korean J Urol.
2009 Apr;50(4):387-395.
Functional, Morphologic, and Molecular Biological Changes in the Bladder of OLETF Diabetic Rats according to Duration of Diabetes Mellitus
- Affiliations
-
- 1Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea. uroljy@catholic.ac.kr
- 2Department of Urology, School of Medicine, Kyung Hee University, Seoul, Korea.
Abstract
- PURPOSE
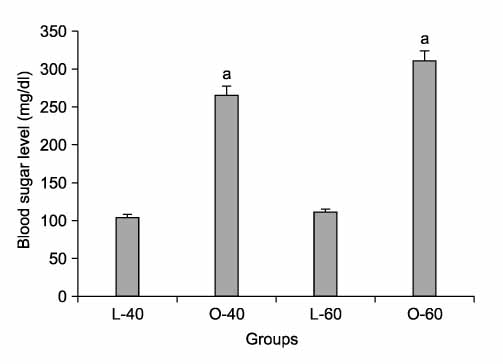
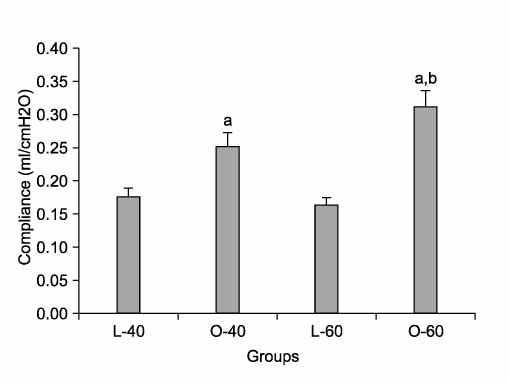
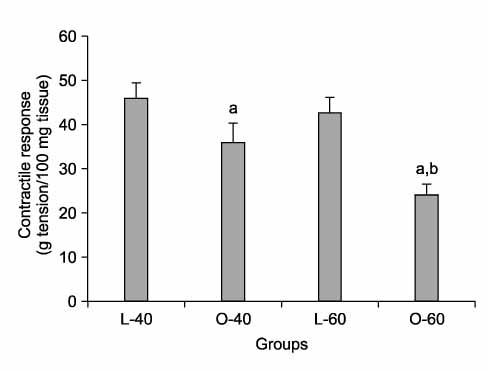
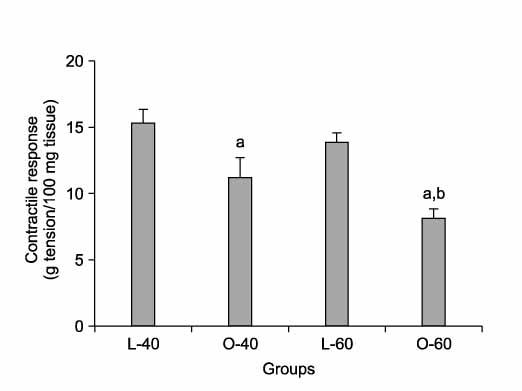
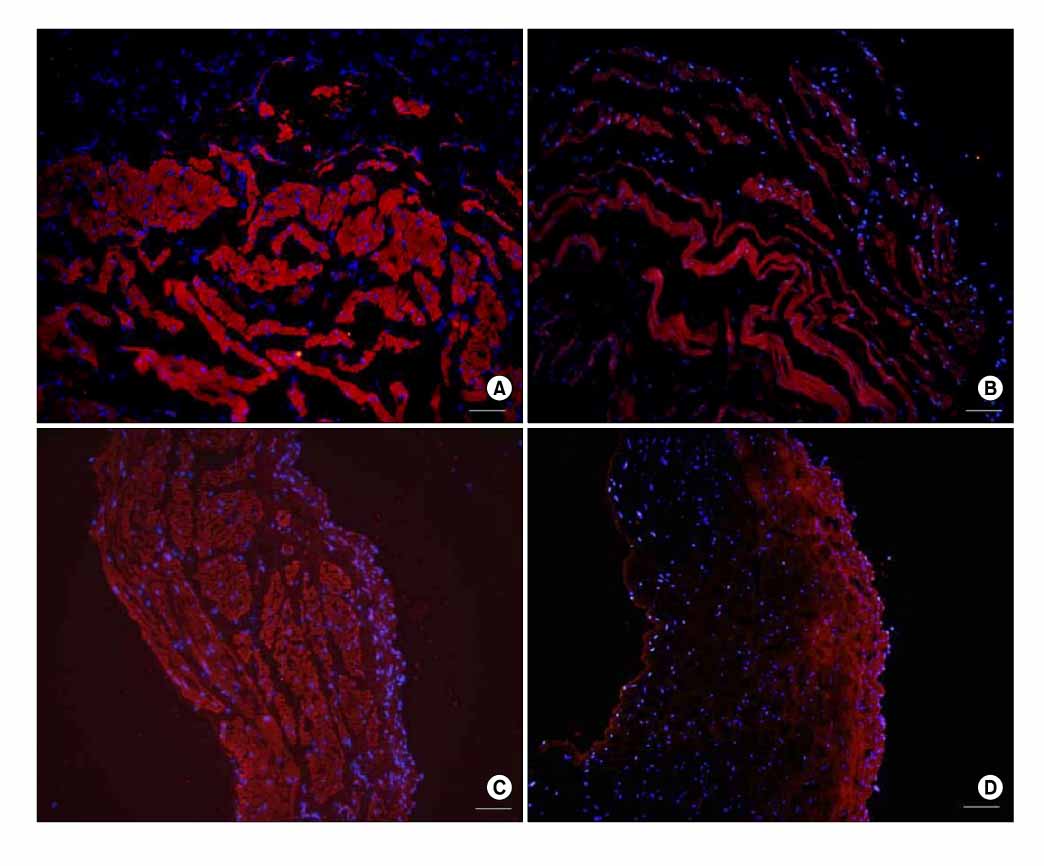
Our study was undertaken to investigate changes in the bladder according to duration of diabetes mellitus in the Otsuka Long Evans Tokushima Fatty (OLETF) rat model, which is similar to type 2 diabetes. MATERIALS AND METHODS: OLETF rats (n=14) and Long Evans Tokushima Otsuka (LETO, n=14) rats were used. LETO is a normal control of OLETF. The animals were assigned to 4 groups: L-40 group, LETO rats 40 weeks after birth (n=7); O-40 group, OLETF rats 40 weeks after birth (n=7); L-60 group, LETO rats 60 weeks after birth (n=7); and O-60 group, OLETF rats 60 weeks after birth (n=7). At 40 weeks or 60 weeks after birth, blood glucose, cystometry, bladder weight, detrusor contractility, and mRNA expression of nerve growth factor (NGF) were assessed. RESULTS: Cystometry showed that diabetic bladders had increased compliance compared with the control groups at 40 and 60 weeks, and the O-60 group had greater compliance than the O-40 group. Contractile responses to electrical stimulation, bethanecol (250microM), and ATP (10 mM) were decreased in the experimental groups compared with the control groups at 40 and 60 weeks, and the O-60 group had a lower contractile response than the O-40 group. The mRNA expression of NGF was decreased in the experimental groups compared with the control groups, and the O-60 group had lower expression than the O-40 group. Changes in NGF were identified through immunohistochemical staining. CONCLUSIONS: The degree of diabetic cystopathy in OLETF rats was changed by duration of type 2 diabetes mellitus. Our results showed that the changes in the bladder in type 2 diabetes mellitus can be identified through a new rat model.
MeSH Terms
-
Adenosine Triphosphate
Animals
Bethanechol
Blood Glucose
Compliance
Dextrans
Diabetes Mellitus
Diabetes Mellitus, Type 2
Drug Combinations
Electric Stimulation
Nerve Growth Factor
Parturition
Rats
Rats, Inbred OLETF
RNA, Messenger
Sodium Chloride
Urinary Bladder
Urinary Bladder, Neurogenic
Adenosine Triphosphate
Bethanechol
Blood Glucose
Dextrans
Drug Combinations
Nerve Growth Factor
RNA, Messenger
Sodium Chloride
Figure
Reference
-
1. Frimodt-Moller C. Diabetic cystopathy: epidemiology and related disorders. Ann Intern Med. 1980. 92:318–321.2. Yoshimura N, Chancellor MB, Andersson KE, Christ GJ. Recent advances in understanding the biology of diabetes-associated bladder complications and novel therapy. BJU Int. 2005. 95:733–738.3. Koo HP, Santarosa RP, Buttyan R, Shabsigh R, Olsson CA, Kaplan SA. Early molecular changes associated with streptozotocin-induced diabetic bladder hypertrophy in the rat. Urol Res. 1993. 21:375–381.4. Steinbacher BC Jr, Nadelhaft I. Increased levels of nerve growth factor in the urinary bladder and hypertrophy of dorsal root ganglion neurons in the diabetic rat. Brain Res. 1998. 782:255–260.5. Kim NS, Moon OR, Kang JH, Lee SY, Jeong BG, Lee SJ, et al. Increasing prevalence of obesity related disease for Koreans associated with overweight and obesity. Korean J Prev Med. 2001. 34:309–315.6. Kawano K, Hirashima T, Mori S, Natori T. OLETF (Otsuka Long-Evans Tokushima Fatty) rat: a new NIDDM rat strain. Diabetes Res Clin Pract. 1994. 24:Suppl. S317–S320.7. Kim JC, Seo SI, Park YH, Hwang TG. Changes of detrusor contractility and growth factors in streptozotosin-induced NIDDM rat. Korean J Urol. 2000. 41:615–621.8. Andersson PO, Malmgren A, Uvelius B. Cystometrical and in vivo evaluation of urinary bladder function in rats with streptozotocin-induced diabetes. J Urol. 1988. 139:1359–1362.9. Longhurst PA, Belis JA. Abnormalities of rat bladder contractility in streptozotocin-induced diabetes mellitus. J Pharmacol Exp Ther. 1986. 238:773–777.10. Eika B, Levin RM, Longhurst PA. Collagen and bladder function in streptozotocin-diabetic rats: effects of insulin and aminoguanidine. J Urol. 1992. 148:167–172.11. Lincoln J, Crockett M, Haven AJ, Burnstock G. Rat bladder in the early stages of streptozotocin-induced diabetes: adrenergic and cholinergic innervation. Diabetologia. 1984. 26:81–87.12. Steers WD, Mackway AM, Ciambotti J, de Groat WC. Effects of streptozotocin-induced diabetes on bladder function in the rat. J Urol. 1990. 143:1032–1036.13. Longhurst PA, Kauer J, Levin RM. The ability of insulin treatment to reverse or prevent the changes in urinary bladder function caused by streptozotocin-induced diabetes mellitus. Gen Pharmacol. 1991. 22:305–311.14. Chung YG, Yoo HG, Kwon YH, Park CS, Lim WS, Ryu JK, et al. The significance of periurethral fibrosis and the change of nitric oxide synthase containing nerves in the urethra of diabetic rats. Korean J Urol. 2007. 48:1050–1057.15. Kang DI, Kim SH, Lee SD, Kwak HS, Choi SH, Kim DR, et al. Effects of Alpha-lipoic acid on nitric oxide synthase expression and ultrastructural changes in the bladder of rats with streptozotocin-induced diabetes. Korean J Urol. 2007. 48:212–218.16. Starer P, Libow L. Cystometric evaluation of bladder dysfunction in elderly diabetic patients. Arch Intern Med. 1990. 150:810–813.17. Kaplan SA, Te AE, Blaivas JG. Urodynamic findings in patients with diabetic cystopathy. J Urol. 1995. 153:342–344.18. Kanda M, Eto K, Tanabe N, Sugiyama A, Hashimoto K, Ueno A. Effects of ONO-2235, an aldose reductase inhibitor, on muscarinic receptors and contractile response of the urinary bladder in rats with streptozotocin-induced diabetes. Jpn J Pharmacol. 1997. 73:221–228.19. Ordonez G, Fernandez A, Perez A, Sotelo J. Low contents of nerve growth factor in serum and submaxillary gland of diabetic mice. A possible etiological element of diabetic neuropathy. J Neurol Sci. 1994. 121:163–166.20. Fernyhough P, Diemel LT, Brewster WJ, Tomlinson DR. Deficits in sciatic nerve neuropeptide content coincide with a reduction in target tissue nerve growth factor messenger RNA in streptozotocin-diabetic rats: effects of insulin treatment. Neuroscience. 1994. 62:337–344.21. Fernyhough P, Diemel LT, Brewster WJ, Tomlinson DR. Altered neurotrophin mRNA levels in peripheral nerve and skeletal muscle of experimentally diabetic rats. J Neurochem. 1995. 64:1231–1237.22. Jakobsen J, Brimijoin S, Skau K, Sidenius P, Wells D. Retrograde axonal transport of transmitter enzymes, fucose-labeled protein, and nerve growth factor in streptozotocin-diabetic rats. Diabetes. 1981. 30:797–803.23. Schmidt RE, Modert CW, Yip HK, Johnson EM Jr. Retrograde axonal transport of intravenously administered 125I-nerve growth factor in rats with streptozotocin-induced diabates. Diabetes. 1993. 32:654–663.24. Hellweg R, Raivich G, Hartung HD, Hock C, Keutzberg GW. Axonal transport of endogenous nerve growth factor (NGF) and NGF receptor in experimental diabetic neuropathy. Exp Neurol. 1994. 130:24–30.25. Hellweg R, Hartung HD. Endogenous levels of nerve growth factor (NGF) are altered in experimental diabetes mellitus: a possible role for NGF in the pathogenesis of diabetic neuropathy. J Neurosci Res. 1990. 26:258–267.26. Sasaki K, Yoshimura N, Chancellor MB. Implications of diabetes mellitus in urology. Urol Clin North Am. 2003. 30:1–12.27. Pittenger G, Vinik A. Nerve growth factor and diabetic neuropathy. Exp Diabesity Res. 2003. 4:271–285.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Moderate Alcohol Intake in the Bladder of the Otsuka Long Evans Tokushima Fatty Diabetic Rats
- Ultrastructural Changes in Corneas of Diabetic Otsuka Long-Evans Tokushima Fatty (OLETF) Rats
- Anti-diabetic effects of benfotiamine on an animal model of type 2 diabetes mellitus
- Effects of Caloric Restriction on the Expression of PGC-1 and PPARs mRNA in Liver of Otsuka Long-Evans Tokushima Fatty Rats
- The Effects of Alpha-Lipoic Acid on Epidermal Nerve Preservation in the Diabetic Neuropathy of OLETF Rats