J Adv Prosthodont.
2015 Jun;7(3):183-190. 10.4047/jap.2015.7.3.183.
Influence of preparation depths on the fracture load of customized zirconia abutments with titanium insert
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Chonnam National University, Gwangju, Korea. mcnihil@jnu.ac.kr
- 2RIS Foundation for Advanced Biomaterials, School of Dentistry, Chonnam National University, Gwangju, Korea.
- KMID: 2284703
- DOI: http://doi.org/10.4047/jap.2015.7.3.183
Abstract
- PURPOSE
This study evaluated the fracture load of customized zirconia abutments with titanium insert according to preparation depths, with or without 5-year artificial aging.
MATERIALS AND METHODS
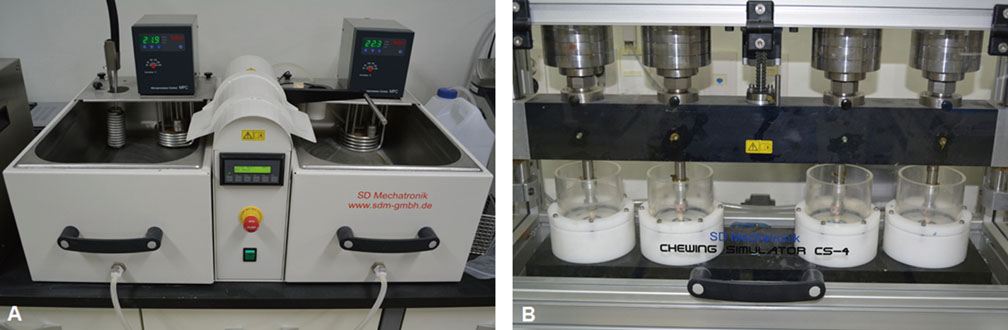
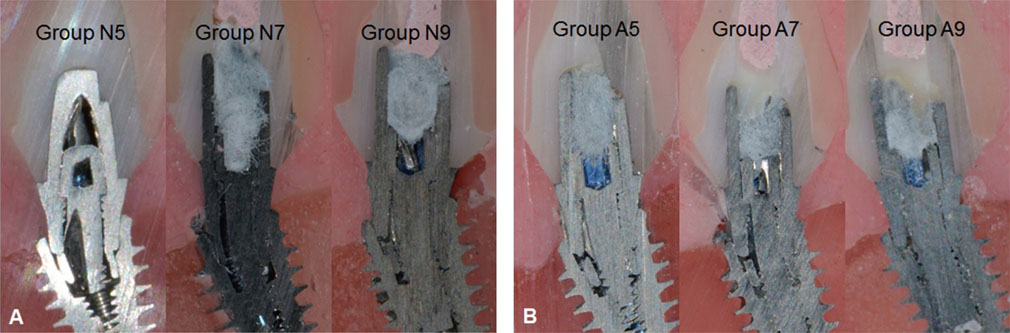
Thirty-six identical lithium disilicate crowns (IPS e.max press) were fabricated to replace a maxillary right central incisor and cemented to the customized zirconia abutment with titanium insert on a 4.5x10 mm titanium fixture. Abutments were fabricated with 3 preparation depths (0.5 mm, 0.7 mm, and 0.9 mm). Half of the samples were then processed using thermocycling (temperature: 5-55degrees C, dwelling time: 120s) and chewing simulation (1,200,000 cycles, 49 N load). All specimens were classified into 6 groups depending on the preparation depth and artificial aging (non-artificial aging groups: N5, N7, N9; artificial aging groups: A5, A7, A9). Static load was applied at 135 degrees to the implant axis in a universal testing machine. Statistical analyses of the results were performed using 1-way ANOVA, 2-way ANOVA, independent t-test and multiple linear regression.
RESULTS
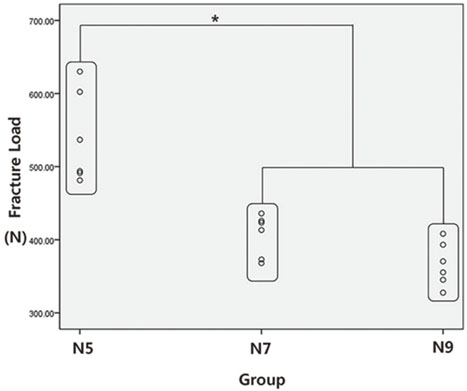
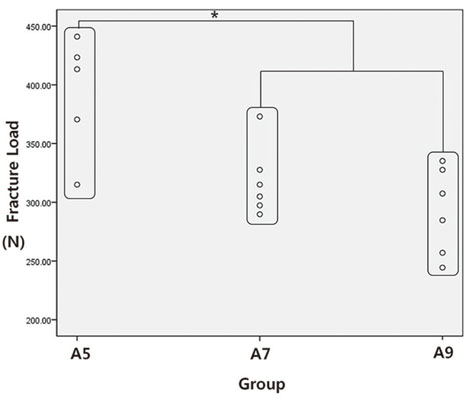
The fracture loads were 539.28 +/- 63.11 N (N5), 406.56 +/- 28.94 N (N7), 366.66 +/- 30.19 N (N9), 392.61 +/- 50.57 N (A5), 317.94 +/- 30.05 N (A7), and 292.74 +/- 37.15 N (A9). The fracture load of group N5 was significantly higher than those of group N7 and N9 (P<.017). Consequently, the fracture load of group A5 was also significantly higher than those of group A7 and A9 (P<.05). After artificial aging, the fracture load was significantly decreased in all groups with various preparation depths (P<.05).
CONCLUSION
The fracture load of a single anterior implant restored with lithium disilicate crown on zirconia abutment with titanium insert differed depending on the preparation depths. After 5-year artificial aging, the fracture loads of all preparation groups decreased significantly.
Keyword
MeSH Terms
Figure
Reference
-
1. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007; 18:97–113.2. Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008; 19:119–130.3. Valenti M, Valenti A. Retrospective survival analysis of 261 lithium disilicate crowns in a private general practice. Quintessence Int. 2009; 40:573–579.4. Wassermann A, Kaiser M, Strub JR. Clinical long-term results of VITA In-Ceram Classic crowns and fixed partial dentures: A systematic literature review. Int J Prosthodont. 2006; 19:355–363.5. Prestipino V, Ingber A. All-ceramic implant abutments: esthetic indications. J Esthet Dent. 1996; 8:255–262.6. Abrahamsson I, Berglundh T, Glantz PO, Lindhe J. The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol. 1998; 25:721–727.7. Prestipino V, Ingber A. Esthetic high-strength implant abutments. Part I. J Esthet Dent. 1993; 5:29–36.8. Prestipino V, Ingber A. Esthetic high-strength implant abutments. Part II. J Esthet Dent. 1993; 5:63–68.9. Sailer I, Philipp A, Zembic A, Pjetursson BE, Hämmerle CH, Zwahlen M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin Oral Implants Res. 2009; 20:4–31.10. Sailer I, Sailer T, Stawarczyk B, Jung RE, Hämmerle CH. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int J Oral Maxillofac Implants. 2009; 24:850–858.11. Truninger TC, Stawarczyk B, Leutert CR, Sailer TR, Hämmerle CH, Sailer I. Bending moments of zirconia and titanium abutments with internal and external implant-abutment connections after aging and chewing simulation. Clin Oral Implants Res. 2012; 23:12–18.12. Aboushelib MN, Salameh Z. Zirconia implant abutment fracture: clinical case reports and precautions for use. Int J Prosthodont. 2009; 22:616–619.13. Kunii J, Hotta Y, Tamaki Y, Ozawa A, Kobayashi Y, Fujishima A, Miyazaki T, Fujiwara T. Effect of sintering on the marginal and internal fit of CAD/CAM-fabricated zirconia frameworks. Dent Mater J. 2007; 26:820–826.14. Park JI, Lee Y, Lee JH, Kim YL, Bae JM, Cho HW. Comparison of fracture resistance and fit accuracy of customized zirconia abutments with prefabricated zirconia abutments in internal hexagonal implants. Clin Implant Dent Relat Res. 2013; 15:769–778.15. Koutayas SO, Mitsias M, Wolfart S, Kern M. Influence of preparation mode and depth on the fracture strength of zirconia ceramic abutments restored with lithium disilicate crowns. Int J Oral Maxillofac Implants. 2012; 27:839–848.16. Mitsias M, Koutayas SO, Wolfart S, Kern M. Influence of zirconia abutment preparation on the fracture strength of single implant lithium disilicate crowns after chewing simulation. Clin Oral Implants Res. 2014; 25:675–682.17. Att W, Kurun S, Gerds T, Strub JR. Fracture resistance of single-tooth implant-supported all-ceramic restorations: an in vitro study. J Prosthet Dent. 2006; 95:111–116.18. Att W, Kurun S, Gerds T, Strub JR. Fracture resistance of single-tooth implant-supported all-ceramic restorations after exposure to the artificial mouth. J Oral Rehabil. 2006; 33:380–386.19. Aramouni P, Zebouni E, Tashkandi E, Dib S, Salameh Z, Almas K. Fracture resistance and failure location of zirconium and metallic implant abutments. J Contemp Dent Pract. 2008; 9:41–48.20. Adatia ND, Bayne SC, Cooper LF, Thompson JY. Fracture resistance of yttria-stabilized zirconia dental implant abutments. J Prosthodont. 2009; 18:17–22.21. Kim S, Kim HI, Brewer JD, Monaco EA Jr. Comparison of fracture resistance of pressable metal ceramic custom implant abutments with CAD/CAM commercially fabricated zirconia implant abutments. J Prosthet Dent. 2009; 101:226–230.22. Butz F, Heydecke G, Okutan M, Strub JR. Survival rate, fracture strength and failure mode of ceramic implant abutments after chewing simulation. J Oral Rehabil. 2005; 32:838–843.23. ISO 14801. Dentistry-fatigue test for endosseous dental implants. Geneva; Switzerland: International Standards Organization (ISO);2005.24. Tsukiyama T, Marcushamer E, Griffin TJ, Arguello E, Magne P, Gallucci GO. Comparison of the anatomic crown width/length ratios of unworn and worn maxillary teeth in Asian and white subjects. J Prosthet Dent. 2012; 107:11–16.25. ISO 10477. Dentistry. Polymer-based crown and bridge materials. Geneva; Switzerland: International Standards Organization (ISO);1996.26. Gale MS, Darvell BW. Thermal cycling procedures for laboratory testing of dental restorations. J Dent. 1999; 27:89–99.27. Krejci I, Lutz F. In-vitro test results of the evaluation of dental restoration systems. Correlation with in-vivo results. Schweiz Monatsschr Zahnmed. 1990; 100:1445–1449.28. Kellerhoff RK, Fischer J. In vitro fracture strength and thermal shock resistance of metal-ceramic crowns with cast and machined AuTi frameworks. J Prosthet Dent. 2007; 97:209–215.29. Culp L, McLaren EA. Lithium disilicate: the restorative material of multiple options. Compend Contin Educ Dent. 2010; 31:716–720. 722724–725.30. Strub JR, Beschnidt SM. Fracture strength of 5 different all-ceramic crown systems. Int J Prosthodont. 1998; 11:602–609.31. Attia A, Kern M. Influence of cyclic loading and luting agents on the fracture load of two all-ceramic crown systems. J Prosthet Dent. 2004; 92:551–556.32. Pera P, Gilodi S, Bassi F, Carossa S. In vitro marginal adaptation of alumina porcelain ceramic crowns. J Prosthet Dent. 1994; 72:585–590.33. Shearer B, Gough MB, Setchell DJ. Influence of marginal configuration and porcelain addition on the fit of In-Ceram crowns. Biomaterials. 1996; 17:1891–1895.34. De Boever JA, McCall WD Jr, Holden S, Ash MM Jr. Functional occlusal forces: an investigation by telemetry. J Prosthet Dent. 1978; 40:326–333.35. Waltimo A, Könönen M. A novel bite force recorder and maximal isometric bite force values for healthy young adults. Scand J Dent Res. 1993; 101:171–175.36. Swab JJ. Low temperature degradation of Y-TZP materials. J Mater Sci. 1991; 26:6706–6714.37. Guazzato M, Albakry M, Ringer SP, Swain MV. Strength, fracture toughness and microstructure of a selection of all-2015-06-24ceramic materials. Part II. Zirconia-based dental ceramics. Dent Mater. 2004; 20:449–456.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of marginal and internal fit of zirconia abutments with titanium abutments in internal hexagonal implants
- Zirconia Abutment Fracture in the Anterior Region: Case Series
- Fracture resistance of zirconia and resin nano ceramic implant abutments according to thickness after thermocycling
- Effect of coloring treatment of translucent zirconia on the masking ability of metal abutment
- Comparison of fit accuracy and torque maintenance of zirconia and titanium abutments for internal tri-channel and external-hex implant connections