Korean Circ J.
2010 Dec;40(12):632-638. 10.4070/kcj.2010.40.12.632.
Effect of Lacidipine on Blood Pressure and Endothelial Function in Mild-to-Moderate Essential Hypertension Patients With Diabetes in Korea
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Seoul National University, Seoul, Korea. ohbhmed@snu.ac.kr
- 2Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Inje University College of Medicine, Busan Paik Hospital, Busan, Korea.
- 4Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- 5Department of Internal Medicine, Konkuk University College of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, Ewha Womans University College of Medicine, Mokdong Hospital, Seoul, Korea.
- 7Department of Internal Medicine, The Catholic University College of Medicine, Seoul St. Mary's Hospital, Seoul, Korea.
- 8Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 9Department of Internal Medicine, Korea University College of Medicine, Anam Hospital, Seoul, Korea.
- 10Department of Internal Medicine, Gachon University Gil Hospital, Incheon, Korea.
- 11Department of Internal Medicine, Wonkwang University College of Medicine, Iksan, Korea.
- 12Department of Internal Medicine, Yonsei University Wonju Christian Hospital, Wonju, Korea.
- 13Department of Internal Medicine, Inje University College of Medicine, IIsan Paik Hospital, Goyang, Korea.
- 14Department of Internal Medicine, Chonnam National University College of Medicine, Gwangju, Korea.
- 15Department of Internal Medicine, Eulji University College of Medicine, Daejeon, Korea.
- 16Department of Internal Medicine, Ajou University College of Medicine, Suwon, Korea.
- 17Department of Internal Medicine, Chungnam National University College of Medicine, Daejeon, Korea.
- 18Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea.
- KMID: 2225161
- DOI: http://doi.org/10.4070/kcj.2010.40.12.632
Abstract
- BACKGROUND AND OBJECTIVES
The aim of this study was to evaluate the efficacy of lacidipine in reducing blood pressure (BP) and to determine its effect on endothelial function in mild-to-moderate hypertensive patients with type 2 diabetes mellitus (DM).
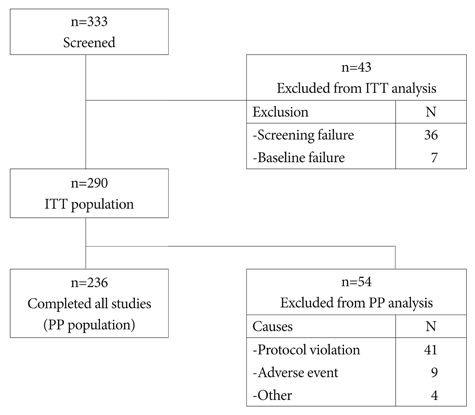
SUBJECTS AND METHODS
This was a prospective, multicenter, open-label, single-arm study, enrolling 290 patients with mild-to-moderate hypertension and type 2 DM. Patients were initially treated with 2 mg lacidipine orally once daily for 4 weeks, which was then increased as necessary every 4 weeks to a maximal dose of 6 mg daily. The primary endpoint was the mean change in systolic blood pressure (SBP) from baseline after 12 weeks of treatment. Secondary endpoints included mean changes in diastolic blood pressure (DBP), flow-mediated vasodilatation (FMD), and serum concentrations of biochemical markers such as high-sensitivity C-reactive protein (hs-CRP), monocyte chemo-attractant protein-1 (MCP-1), matrix metalloproteinase-9 (MMP-9), and plasminogen activator inhibitor-1 (PAI-1).
RESULTS
Lacidipine treatment significantly reduced SBP by -13.4+/-13.0 mmHg (p<0.001) and DBP by -6.2+/-9.3 mmHg (p<0.001). Lacidipine treatment did not improve endothelial-dependent vasodilatation, despite significantly improved nitroglycerin-induced, endothelial-independent vasodilatation. MCP-1 levels significantly decreased from 283.66+/-110.08 pg/mL to 257.83+/-100.23 pg/mL (p<0.001); whereas there were no significant changes in the levels of hs-CRP, MMP-9, or PAI-1.
CONCLUSION
Twelve weeks of treatment with lacidipine was effective and well tolerated in mild-to-moderate hypertensive patients with type 2 DM. In spite of inducing a significant reduction in MCP-1 levels, lacidipine did not improve endothelial function.
Keyword
MeSH Terms
-
Biomarkers
Blood Pressure
C-Reactive Protein
Diabetes Mellitus
Diabetes Mellitus, Type 2
Dihydropyridines
Endothelium
Humans
Hypertension
Korea
Matrix Metalloproteinase 9
Monocytes
Plasminogen Activators
Prospective Studies
Vasodilation
C-Reactive Protein
Dihydropyridines
Matrix Metalloproteinase 9
Plasminogen Activators
Figure
Reference
-
1. Arauz-Pacheco C, Parrott MA, Raskin P. Treatment of hypertension in adults with diabetes. Diabetes Care. 2003. 26:Suppl 1. S80–S82.2. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003. 289:2560–2572.3. Kim KI, Kim Y, Kim HJ, et al. Current status and characteristics of hypertension treatment by primary physicians in Korea: data from Korean Epidemiology Study on Hypertension (KEY Study). Am J Hypertens. 2008. 21:884–889.4. Sowers JR, Haffner S. Treatment of cardiovascular and renal risk factors in the diabetic hypertensive. Hypertension. 2002. 40:781–788.5. Taddei S, Virdis A, Ghiadoni L, Sudano I, Salvetti A. Effects of antihypertensive drugs on endothelial dysfunction: clinical implications. Drugs. 2002. 62:265–284.6. Zanchetti A, Bond MG, Hennig M, et al. Absolute and relative changes in carotid intima-media thickness and atherosclerotic plaques during long-term antihypertensive treatment: further results of the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens. 2004. 22:1201–1212.7. Zanchetti A, Bond MG, Hennig M, et al. Calcium antagonist lacidipine slows down progression of asymptomatic carotid atherosclerosis: principal results of the European Lacidipine Study on Atherosclerosis (ELSA), a randomized, double-blind, long-term trial. Circulation. 2002. 106:2422–2427.8. Frattola A, Parati G, Castiglioni P, et al. Lacidipine and blood pressure variability in diabetic hypertensive patients. Hypertension. 2000. 36:622–628.9. Corretti MC, Anderson TJ, Benjamin EJ, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002. 39:257–265.10. Salako BL, Kadiri S, Walker O, Fehintola FA. Evaluation of lacidipine (a calcium blocker) in the treatment of hypertension in black African people: a double-blind comparison with hydrochlorothiazide. Afr J Med Med Sci. 1998. 27:73–75.11. Tcherdakoff P. French large-scale study evaluating the tolerability and efficacy of lacidipine. J Cardiovasc Pharmacol. 1995. 25:Suppl 3. S27–S32.12. Kim DH, Oh SI, Kim YK, Choi SW, Yoo WS. Efficacy and safety of nifedipine gastrointestinal therapeutic system (Adalat OROS) in patients with mild to moderate essential hypertension. Korean Circ J. 1992. 22:488–493.13. Choi YJ, Lee MM, Choe SJ, et al. A randomized, double-blind clinical trial to determine the efficacy of carvedilol vs. atenolol in patients with stage 1 to 2 essential hypertension. Korean Circ J. 1998. 28:359–365.14. Jin SB, Rhee YW, Chang SW, Kim KC, Kim SP, Song CS. Effects of dihydrochlorothiazide, propranolol, and prazosin on serum lipids in patients with essential hypertension. Korean Circ J. 1985. 15:329–336.15. Cheong HJ, Kang HS, Choue CW, et al. Antihypertensive effects and safety of isradipine in patients with essential hypertension. Korean Circ J. 1993. 23:741–749.16. Park SW, Doo YC, Kim WH, et al. Amlodipine monotherapy in patients with mild to moderate essential hypertension. Korean Circ J. 1992. 22:852–857.17. Pieper GM, Gross GJ. Oxygen free radicals abolish endothelium-dependent relaxation in diabetic rat aorta. Am J Physiol. 1988. 255:H825–H833.18. Tesfamariam B, Cohen RA. Free radicals mediate endothelial cell dysfunction caused by elevated glucose. Am J Physiol. 1992. 263:H321–H326.19. Dai FX, Diederich A, Skopec J, Diederich D. Diabetes-induced endothelial dysfunction in streptozotocin-treated rats: role of prostaglandin endoperoxides and free radicals. J Am Soc Nephrol. 1993. 4:1327–1336.20. Yugar-Toledo JC, Tanus-Santos JE, Sabha M, et al. Uncontrolled hypertension, uncompensated type II diabetes, and smoking have different patterns of vascular dysfunction. Chest. 2004. 125:823–830.21. Balletshofer BM, Goebbel S, Rittig K, et al. Intense cholesterol lowering therapy with a HMG-CoA reductase inhibitor does not improve nitric oxide dependent endothelial function in type-2-diabetes: a multicenter, randomised, double-blind, three-arm placebo-controlled clinical trial. Exp Clin Endocrinol Diabetes. 2005. 113:324–330.22. Stroes ES, Koomans HA, de Bruin TW, Rabelink TJ. Vascular function in the forearm of hypercholesterolaemic patients off and on lipid-lowering medication. Lancet. 1995. 346:467–471.23. Economides PA, Caselli A, Tiani E, Khaodhiar L, Horton ES, Veves A. The effects of atorvastatin on endothelial function in diabetic patients and subjects at risk for type 2 diabetes. J Clin Endocrinol Metab. 2004. 89:740–747.24. Guerci B, Bohme P, Kearney-Schwartz A, Zannad F, Drouin P. Endothelial dysfunction and type 2 diabetes: part 2. altered endothelial function and the effects of treatments in type 2 diabetes mellitus. Diabetes Metab. 2001. 27:436–447.25. Braunersreuther V, Mach F, Steffens S. The specific role of chemokines in atherosclerosis. Thromb Haemost. 2007. 97:714–721.26. Sardo MA, Campo S, Mandraffino G, et al. Tissue factor and monocyte chemoattractant protein-1 expression in hypertensive individuals with normal or increased carotid intima-media wall thickness. Clin Chem. 2008. 54:814–823.27. Bae JH, Bassenge E, Lim DM, Synn YC, Kim KY, Schwemmer M. Effects of lacidipine on vascular responses in patients with coronary artery disease. Int J Cardiol. 2005. 101:377–383.28. Koh KK, Han SH, Chung WJ, et al. Comparison of effects of losartan, irbesartan, and candesartan on flow-mediated brachial artery dilation and on inflammatory and thrombolytic markers in patients with systemic hypertension. Am J Cardiol. 2004. 93:1432–1435. A10.29. Juhan-Vague I, Alessi MC, Vague P. Thrombogenic and fibrinolytic factors and cardiovascular risk in non-insulin-dependent diabetes mellitus. Ann Med. 1996. 28:371–380.30. Kaikita K, Fogo AB, Ma L, Schoenhard JA, Brown NJ, Vaughan DE. Plasminogen activator inhibitor-1 deficiency prevents hypertension and vascular fibrosis in response to long-term nitric oxide synthase inhibition. Circulation. 2001. 104:839–844.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antihypertensive Effect of Captopril on Essential Hypertension
- Efficacy and Safety of Nifedipine Gastrointestinal Therapeutic System(Adalat OROS) in Patients with Mild to Moderate Essential Hypertension
- Blood Pressure Variability and Vascular Dysfunction in Essential Hypertension
- Manidipine Monotherapy in Patients with Mild to Moderate Essential Hypertension
- Hypotensive Effect of Perindopril in Patients with Essential Hypertension