Korean Circ J.
2012 Aug;42(8):551-557. 10.4070/kcj.2012.42.8.551.
Lack of Association Between Low Density Lipoprotein Particle Size and On-Treatment Platelet Reactivity in Patients With Coronary Artery Disease
- Affiliations
-
- 1Department of Internal Medicine, Cardiovascular Center, Seoul National University Hospital, Seoul, Korea. hanname@medimail.co.kr
- 2Department of Internal Medicine, Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea. cheolkim@plaza.snu.ac.kr
- KMID: 2225005
- DOI: http://doi.org/10.4070/kcj.2012.42.8.551
Abstract
- BACKGROUND AND OBJECTIVES
Small dense low density lipoproteins (sd-LDL) are a risk factor for coronary artery disease and are known to stimulate platelet function in vitro. This study aimed to evaluate whether high proportion of sd-LDL is associated with high on-treatment platelet reactivity (HOPR).
SUBJECTS AND METHODS
From January 2009 to March 2010, 439 subjects (mean age: 64.3+/-9.7, Male : Female=306 : 133) were enrolled from the low density LIPOProtein-cholesterol Size measurement Registry with coronary artery disease, who had undergone elective percutaneous coronary intervention and measured both LDL particle size and on-treatment platelet reactivity (OPR). Mean LDL particle size was measured by gradient gel electrophoresis (Quantimetrix, Lipoprint(TM)) and OPR by the VerifyNow(TM) system (aspirin and P2Y12).
RESULTS
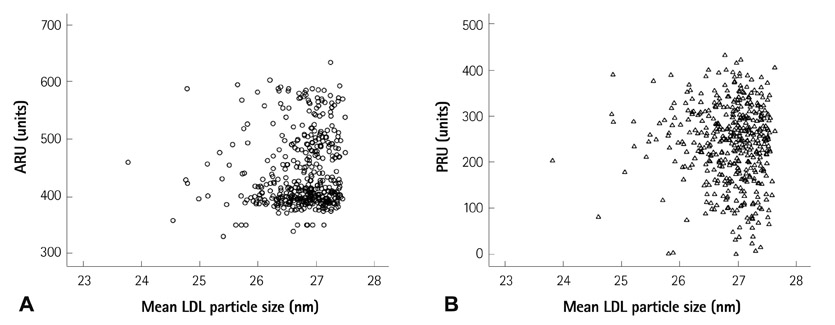
Between pattern A (large, buoyant LDL dominant) and B (sd-LDL dominant) population, there were no significant difference in OPR to aspirin (441.3+/-71.9 vs. 434.07+/-63.45 aspirin reaction units, p=0.351) or clopidogrel (237.9+/-87.3 vs. 244.9+/-80.7 P2Y12 reaction units, p=0.465). There was no difference in LDL particle size between patients with HOPR compared with non-HOPR patients (aspirin: 26.8+/-0.5 vs. 26.7+/-0.6 nm, p=0.078, clopidogrel: 26.7+/-0.6 vs. 26.8+/-0.5 nm, p=0.857). Pearson's correlation coefficients between LDL particle size and platelet reactivity were not statistically significant (aspirin assay: r=0.080, p=0.098, P2Y12 assay: r=-0.027, p=0.568).
CONCLUSION
There was no significant association between LDL particle size and OPR in patients with coronary artery disease.
MeSH Terms
Figure
Reference
-
1. Marcucci R, Gori AM, Paniccia R, et al. Cardiovascular death and nonfatal myocardial infarction in acute coronary syndrome patients receiving coronary stenting are predicted by residual platelet reactivity to ADP detected by a point-of-care assay: a 12-month follow-up. Circulation. 2009. 119:237–242.2. Breet NJ, van Werkum JW, Bouman HJ, et al. High on-treatment platelet reactivity to both aspirin and clopidogrel is associated with the highest risk of adverse events following percutaneous coronary intervention. Heart. 2011. 97:983–990.3. Kim JY, Yoon J. Aspirin and clopidogrel resistance in drug eluting stent era. Korean Circ J. 2007. 37:135–147.4. Ip S, Lichtenstein AH, Chung M, Lau J, Balk EM. Systematic review: association of low-density lipoprotein subfractions with cardiovascular outcomes. Ann Intern Med. 2009. 150:474–484.5. El Harchaoui K, van der Steeg WA, Stroes ES, et al. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007. 49:547–553.6. Koba S, Yokota Y, Hirano T, et al. Small LDL-cholesterol is superior to LDL-cholesterol for determining severe coronary atherosclerosis. J Atheroscler Thromb. 2008. 15:250–260.7. Rizzo M, Berneis K, Corrado E, Novo S. The significance of low-density-lipoproteins size in vascular diseases. Int Angiol. 2006. 25:4–9.8. Borén J, Gustafsson M, Skålén K, Flood C, Innerarity TL. Role of extracellular retention of low density lipoproteins in atherosclerosis. Curr Opin Lipidol. 2000. 11:451–456.9. Hurt-Camejo E, Camejo G, Sartipy P. Phospholipase A2 and small, dense low-density lipoprotein. Curr Opin Lipidol. 2000. 11:465–471.10. Weisser B, Locher R, de Graaf J, Moser R, Sachinidis A, Vetter W. Low density lipoprotein subfractions increase thromboxane formation in endothelial cells. Biochem Biophys Res Commun. 1993. 192:1245–1250.11. Hoefner DM, Hodel SD, O'Brien JF, et al. Development of a rapid, quantitative method for LDL subfractionation with use of the Quantimetrix Lipoprint LDL System. Clin Chem. 2001. 47:266–274.12. Krauss RM, Burke DJ. Identification of multiple subclasses of plasma low density lipoproteins in normal humans. J Lipid Res. 1982. 23:97–104.13. Kazumi T, Kawaguchi A, Hozumi T, et al. Low density lipoprotein particle diameter in young, nonobese, normolipidemic Japanese men. Atherosclerosis. 1999. 142:113–119.14. Yoon Y, Song J, Park HD, Park KU, Kim JQ. Significance of small dense low-density lipoproteins as coronary risk factor in diabetic and non-diabetic Korean populations. Clin Chem Lab Med. 2005. 43:431–437.15. Kwon SW, Yoon SJ, Kang TS, et al. Significance of small dense low-density lipoprotein as a risk factor for coronary artery disease and acute coronary syndrome. Yonsei Med J. 2006. 47:405–414.16. Van Werkum JW, Harmsze AM, Elsenberg EH, Bouman HJ, ten Berg JM, Hackeng CM. The use of the VerifyNow system to monitor antiplatelet therapy: a review of the current evidence. Platelets. 2008. 19:479–488.17. Paniccia R, Antonucci E, Gori AM, et al. Different methodologies for evaluating the effect of clopidogrel on platelet function in high-risk coronary artery disease patients. J Thromb Haemost. 2007. 5:1839–1847.18. De Graaf J, Hak-Lemmers HL, Hectors MP, Demacker PN, Hendriks JC, Stalenhoef AF. Enhanced susceptibility to in vitro oxidation of the dense low density lipoprotein subfraction in healthy subjects. Arterioscler Thromb. 1991. 11:298–306.19. Chen LY, Mehta P, Mehta JL. Oxidized LDL decreases L-arginine uptake and nitric oxide synthase protein expression in human platelets: relevance of the effect of oxidized LDL on platelet function. Circulation. 1996. 93:1740–1746.20. Wang JS, Lin CC, Chen JK, Wong MK. Role of chronic exercise in decreasing oxidized LDL-potentiated platelet activation by enhancing platelet-derived no release and bioactivity in rats. Life Sci. 2000. 66:1937–1948.21. Collot-Teixeira S, De Lorenzo F, McGregor JL. Scavenger receptor A and CD36 are implicated in mediating platelet activation induced by oxidized low-density lipoproteins. Arterioscler Thromb Vasc Biol. 2007. 27:2491–2492.22. Lee PY, Chen WH, Ng W, et al. Low-dose aspirin increases aspirin resistance in patients with coronary artery disease. Am J Med. 2005. 118:723–727.23. Cecchi E, Marcucci R, Paniccia R, et al. Effect of blood hematocrit and erythrocyte deformability on adenosine 5'-diphosphate platelet reactivity in patients with acute coronary syndromes on dual antiplatelet therapy. Am J Cardiol. 2009. 104:764–768.24. Kleinbongard P, Schulz R, Rassaf T, et al. Red blood cells express a functional endothelial nitric oxide synthase. Blood. 2006. 107:2943–2951.25. Carroll JS, Ku CJ, Karunarathne W, Spence DM. Red blood cell stimulation of platelet nitric oxide production indicated by quantitative monitoring of the communication between cells in the bloodstream. Anal Chem. 2007. 79:5133–5138.26. Park KW, Park JJ, Jeon KH, et al. Enhanced clopidogrel responsiveness in smokers: smokers’ paradox is dependent on cytochrome P450 CYP1A2 status. Arterioscler Thromb Vasc Biol. 2011. 31:665–671.27. Rosenson RS. Myocardial injury: the acute phase response and lipoprotein metabolism. J Am Coll Cardiol. 1993. 22:933–940.28. Barth JH, Jackson BM, Farrin AJ, et al. Change in serum lipids after acute coronary syndromes: secondary analysis of SPACE ROCKET study data and a comparative literature review. Clin Chem. 2010. 56:1592–1598.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Low-Density Lipoprotein Subclasses and Lipoprotein Lipase Gene Polymorphisms in Coronary Artery Disease
- Low-Density Lipoprotein Particle Size Distribution in Subjects with Coronary Artery Disease
- Smaller Mean LDL Particle Size and Higher Proportion of Small Dense LDL in Korean Type 2 Diabetic Patients
- Effects of Platelet Number and Platelet Indices on Platelet Reactivity in Patients Treated with Clopidogrel or Ticagrelor
- Significance of Small Dense Low-Density Lipoprotein as a Risk Factor for Coronary Artery Disease and Acute Coronary Syndrome