Korean Circ J.
2013 Nov;43(11):774-781. 10.4070/kcj.2013.43.11.774.
A Case of Progressive Ductal Constriction in a Fetus
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea. choi3628@snuh.ac.kr
- 2Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Pediatric Cardiology, Harbin Children's Hospital, Harbin, China.
- KMID: 2224811
- DOI: http://doi.org/10.4070/kcj.2013.43.11.774
Abstract
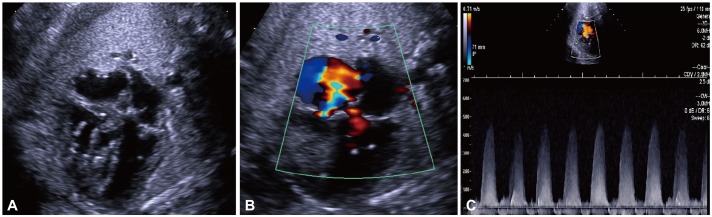
- The ductus arteriosus is a normal and essential structure in fetal circulation. Since the introduction of fetal echocardiography, there have been reports of ductal constriction, many of which were related to maternal use of some medications. However, there have been some reports of idiopathic ductal constriction, which usually present in later gestation. Recently we experienced a case, which initially showed an S-shaped ductus with mild narrowing at 23 weeks and 27 weeks gestation and developed severe ductal constriction at 33 weeks. Soon after birth, ductus was searched for but no ductus was found in 2-D and color images. The neonate required mechanical ventilation with supplemental oxygen for 3 days. All echocardiographic abnormalities were normalized in 7 months. We report progressive ductal constriction in an S-shaped ductus and emphasize the importance of continuous follow up extending to the third trimester and even immediately after birth.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Idiopathic Constriction of the Fetal Ductus Arteriosus with Right Ventricular Failure; Rapid Resolution after Birth
Doo Ri Lee, Kyung Jin Ahn, Gi Beom Kim, Bo Sang Kwon, Eun Jung Bae, Chung Il Noh
Korean J Perinatol. 2014;25(4):297-301. doi: 10.14734/kjp.2014.25.4.297.
Reference
-
1. Weichert J, Hartge DR, Axt-Fliedner R. The fetal ductus arteriosus and its abnormalities--a review. Congenit Heart Dis. 2010; 5:398–408. PMID: 21087423.2. Tulzer G, Gudmundsson S, Sharkey AM, Wood DC, Cohen AW, Huhta JC. Doppler echocardiography of fetal ductus arteriosus constriction versus increased right ventricular output. J Am Coll Cardiol. 1991; 18:532–536. PMID: 1856423.3. Mielke G, Benda N. Blood flow velocity waveforms of the fetal pulmonary artery and the ductus arteriosus: reference ranges from 13 weeks to term. Ultrasound Obstet Gynecol. 2000; 15:213–218. PMID: 10846777.4. Trevett TN Jr, Cotton J. Idiopathic constriction of the fetal ductus arteriosus. Ultrasound Obstet Gynecol. 2004; 23:517–519. PMID: 15133807.5. Harada K, Rice MJ, Shiota T, McDonald RW, Reller MD, Sahn DJ. Two-dimensional echocardiographic evaluation of ventricular systolic function in human fetuses with ductal constriction. Ultrasound Obstet Gynecol. 1997; 10:247–253. PMID: 9383875.6. Luchese S, Mânica JL, Zielinsky P. Intrauterine ductus arteriosus constriction: analysis of a historic cohort of 20 cases. Arq Bras Cardiol. 2003; 81:405–410. 399–404. PMID: 14666282.7. Benson CB, Brown DL, Doubilet PM, DiSalvo DN, Laing FC, Frates MC. Increasing curvature of the normal fetal ductus arteriosus with advancing gestational age. Ultrasound Obstet Gynecol. 1995; 5:95–97. PMID: 7719875.8. Soslow JH, Friedberg MK, Silverman NH. Idiopathic premature closure of the ductus arteriosus: an indication for early delivery. Echocardiography. 2008; 25:650–652. PMID: 18422673.9. Zielinsky P, Piccoli AL Jr, Manica JL, et al. Maternal consumption of polyphenol-rich foods in late pregnancy and fetal ductus arteriosus flow dynamics. J Perinatol. 2010; 30:17–21. PMID: 19641513.10. Shima Y, Ishikawa H, Matsumura Y, Yashiro K, Nakajima M, Migita M. Idiopathic severe constriction of the fetal ductus arteriosus: a possible underestimated pathophysiology. Eur J Pediatr. 2011; 170:237–240. PMID: 20845046.11. Enzensberger C, Wienhard J, Weichert J, et al. Idiopathic constriction of the fetal ductus arteriosus: three cases and review of the literature. J Ultrasound Med. 2012; 31:1285–1291. PMID: 22837295.12. Gewillig M, Brown SC, De Catte L, et al. Premature foetal closure of the arterial duct: clinical presentations and outcome. Eur Heart J. 2009; 30:1530–1536. PMID: 19389789.13. Mielke G, Peukert U, Krapp M, Schneider-Pungs J, Gembruch U. Fetal and transient neonatal right heart dilatation with severe tricuspid valve insufficiency in association with abnormally S-shaped kinking of the ductus arteriosus. Ultrasound Obstet Gynecol. 1995; 5:338–341. PMID: 7614140.14. Chao RC, Ho ES, Hsieh KS. Doppler echocardiographic diagnosis of intrauterine closure of the ductus arteriosus. Prenat Diagn. 1993; 13:989–994. PMID: 8309905.15. Hofstadler G, Tulzer G, Altmann R, Schmitt K, Danford D, Huhta JC. Spontaneous closure of the human fetal ductus arteriosus--A cause of fetal congestive heart failure. Am J Obstet Gynecol. 1996; 174:879–883. PMID: 8633660.16. Leal SD, Cavallé-Garrido T, Ryan G, Farine D, Heilbut M, Smallhorn JF. Isolated ductal closure in utero diagnosed by fetal echocardiography. Am J Perinatol. 1997; 14:205–210. PMID: 9259929.17. Mielke G, Steil E, Breuer J, Goelz R. Circulatory changes following intrauterine closure of the ductus arteriosus in the human fetus and newborn. Prenat Diagn. 1998; 18:139–145. PMID: 9516015.18. Wei S, Ailu C, Ying Z, Yili Z. Idiopathic occlusion of the fetal ductus arteriosus without lumen narrowing. Echocardiography. 2011; 28:E85–E88. PMID: 21426387.19. Nygaard SI, Petersen OB, Garne E, Sørensen KE. Spontaneous prenatal ductal closure: postnatal diagnosis? Pediatr Cardiol. 2009; 30:176–180. PMID: 18779991.20. Ishida H, Inamura N, Kawazu Y, Kayatani F. Clinical features of the complete closure of the ductus arteriosus prenatally. Congenit Heart Dis. 2011; 6:51–56. PMID: 21269413.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital Constriction Band of the Face: A Case Report
- Fetal Death Secondary to Constriction and Torsion of Umbilical Cord: An autopsy case
- Fetus Papyraceus Caused by Velamentous Insertion of Cord to Dividing Membrane
- A Case of Single Fetal Death in Twin Pregnancy
- A Case of Amniotic Band Syndrome as a Cause of Anencephaly