J Korean Assoc Oral Maxillofac Surg.
2016 Feb;42(1):2-8. 10.5125/jkaoms.2016.42.1.2.
Low-level laser therapy affects osseointegration in titanium implants: resonance frequency, removal torque, and histomorphometric analysis in rabbits
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, On General Hospital, Busan, Korea.
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry, Pusan National University, Yangsan, Korea. ydkimdds@pusan.ac.kr
- 3Department of Oral Anatomy, School of Dentistry, Pusan National University, Yangsan, Korea.
- 4Institute of Translational Dental Sciences and Dental Research Institute, Pusan National University Dental Hospital, Yangsan, Korea.
- KMID: 2189400
- DOI: http://doi.org/10.5125/jkaoms.2016.42.1.2
Abstract
OBJECTIVES
The purpose of this study was to investigate the effects of low-level laser therapy (LLLT) with a diode gallium-aluminum-arsenide (Ga-Al-As) low-level laser device on the healing and attachment of titanium implants in bone.
MATERIALS AND METHODS
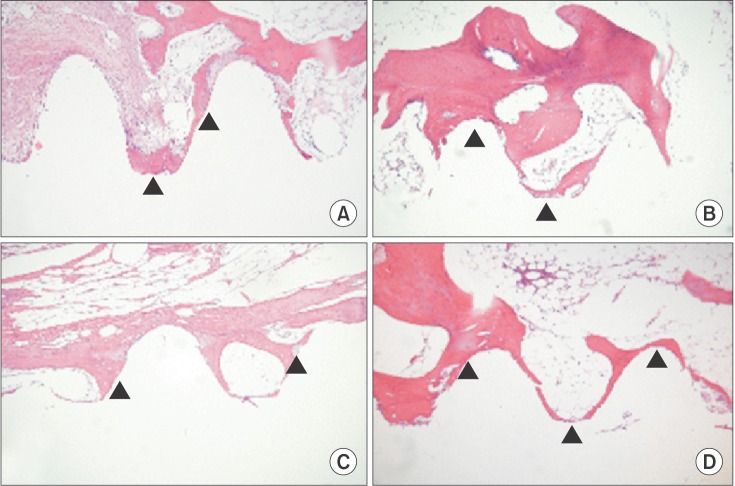
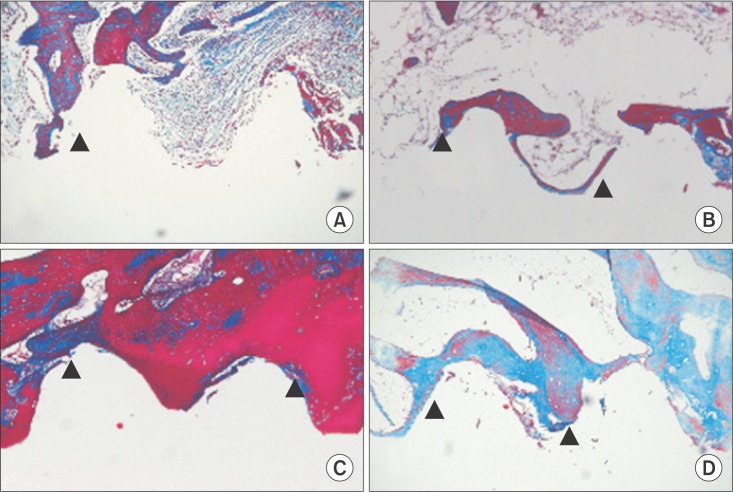
Thirteen New Zealand white male rabbits weighing 3.0+/-0.5 kg were used for this study. Dental titanium implants (3.75 mm in diameter and 8.5 mm in length, US II RBM plus fixture; Osstem, Seoul, Korea) were implanted into both femurs of each rabbit. The rabbits were randomly divided into a LLLT group and a control group. The LLLT was initiated immediately after surgery and then repeated daily for 7 consecutive days in the LLLT group. Six weeks and 12 weeks after implantation, we evaluated and compared the osseointegration of the LLLT group and control group, using histomorphometric analysis, removal torque testing, and resonance frequency analysis (RFA). The results were statistically significant when the level of probability was 0.05 or less based on a non-parametric Mann-Whitney U-test.
RESULTS
The implant survival rate was about 96%. Histologically and histomorphometrically, we observed that the titanium implants were more strongly attached in LLLT group than in control group. However, there was no significant difference between the LLLT group and control group in removal torque or RFA.
CONCLUSION
Histologically, LLLT might promote cell-level osseointegration of titanium implants, but there was no statistically significant effects.
Keyword
MeSH Terms
Figure
Reference
-
1. Kemmotsu O, Sato K, Furumido H, Harada K, Takigawa C, Kaseno S, et al. Efficacy of low reactive-level laser therapy for pain attenuation of postherpetic neuralgia. Laser Ther. 1991; 3:71–75.
Article2. Braverman B, McCarthy RJ, Ivankovich AD, Forde DE, Overfield M, Bapna MS. Effect of helium-neon and infrared laser irradiation on wound healing in rabbits. Lasers Surg Med. 1989; 9:50–58. PMID: 2927230.
Article3. Midamba E, Haanaes HR. Therapeutic effect of low level laser irradiation on inferior alveolar, mental and lingual nerve paresthesia. Laser Ther. 1993; 5:89–94.4. Takeda Y. Irradiation effect of low-energy laser on alveolar bone after tooth extraction. Experimental study in rats. Int J Oral Maxillofac Surg. 1988; 17:388–391. PMID: 3145957.
Article5. Khadra M, Rønold HJ, Lyngstadaas SP, Ellingsen JE, Haanaes HR. Low-level laser therapy stimulates bone-implant interaction: an experimental study in rabbits. Clin Oral Implants Res. 2004; 15:325–332. PMID: 15142095.
Article6. Khadra M, Lyngstadaas SP, Haanaes HR, Mustafa K. Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials. 2005; 26:3503–3509. PMID: 15621240.
Article7. Khadra M. The effect of low level laser irradiation on implant-tissue interaction: in vivo and in vitro studies. Swed Dent J Suppl. 2005; (172):1–63. PMID: 15906852.8. Guzzardella GA, Torricelli P, Nicoli-aldini N, Giardino R. Osseointegration of endosseous ceramic implants after postoperative low-power laser stimulation: an in vivo comparative study. Clin Oral Implants Res. 2003; 14:226–232. PMID: 12656884.9. Maluf AP, Maluf RP, Brito CR, França FM, De BRJ. Mechanical evaluation of the influence of low-level laser therapy in secondary stability of implants in mice shinbones. Lasers Med Sci. 2010; 25:693–698. PMID: 20393769.
Article10. Kim YD, Kim SS, Hwang DS, Kim SG, Kwon YH, Shin SH, et al. Effect of low-level laser treatment after installation of dental titanium implant-immunohistochemical study of RANKL, RANK, OPG: an experimental study in rats. Lasers Surg Med. 2007; 39:441–450. PMID: 17523169.
Article11. Pereira CL, Sallum EA, Nociti FH Jr, Moreira RW. The effect of low-intensity laser therapy on bone healing around titanium implants: a histometric study in rabbits. Int J Oral Maxillofac Implants. 2009; 24:47–51. PMID: 19344024.12. Becker W, Sennerby L, Bedrossian E, Becker BE, Lucchini JP. Implant stability measurements for implants placed at the time of extraction: a cohort, prospective clinical trial. J Periodontol. 2005; 76:391–397. PMID: 15857073.
Article13. Friberg B, Sennerby L, Linden B, Gröndahl K, Lekholm U. Stability measurements of one-stage Brånemark implants during healing in mandibles: a clinical resonance frequency analysis study. Int J Oral Maxillofac Surg. 1999; 28:266–272. PMID: 10416893.14. Oh JS, Kim SG. Clinical study of the relationship between implant stability measurements using Periotest and Osstell mentor and bone quality assessment. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:e35–e40. PMID: 22669155.
Article15. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998; 11:491–501. PMID: 9922740.16. Atsumi M, Park SH, Wang HL. Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants. 2007; 22:743–754. PMID: 17974108.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of removal torque of saline-soaking RBM implants and RBM implants in rabbit tibias
- Comparison of the removal torque and a histomorphometric evaluation of the RBM treated implants with the RBM followed by laser treated implants: an experimental study in rabbits
- On the effect of saline immersion to the removal torque for resorbable blasting media and acid treated implants
- Histomorphometric and Removal Torque Values Comparision of Rough Surface Titanium Implants
- Comparison of removal torques of SLActive® implant and blasted, laser-treated titanium implant in rabbit tibia bone healed with concentrated growth factor application