J Rhinol.
2016 May;23(1):55-59. 10.18787/jr.2016.23.1.55.
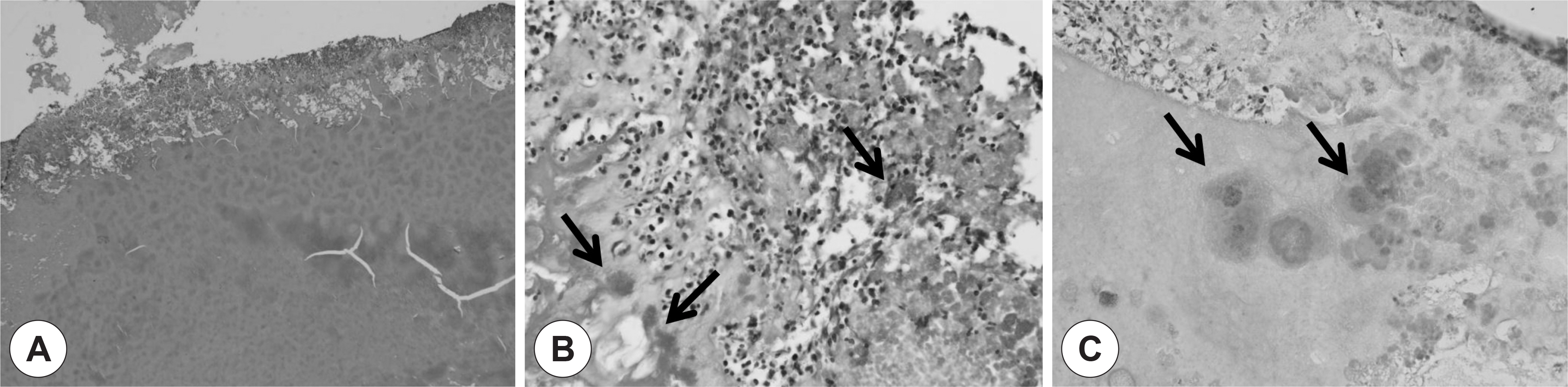
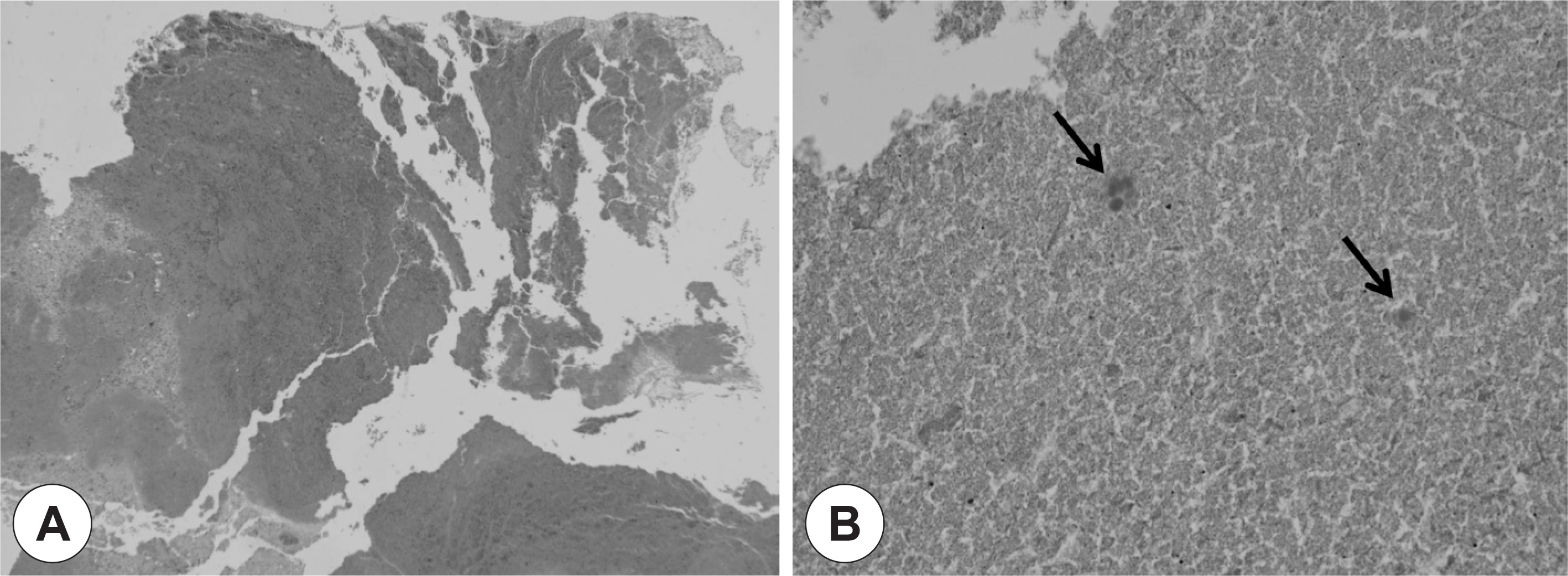
Bioballs Causing Asymptomatic or Recurrent Acute Rhinosinusitis: Two Cases
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, College of Medicine, Hanyang University, Seoul, Korea. shcho@hanyang.ac.kr
- 2Department of Pathology, College of Medicine, Hanyang University, Seoul, Korea.
- KMID: 2165156
- DOI: http://doi.org/10.18787/jr.2016.23.1.55
Abstract
- A variety of intrinsic and extrinsic factors have been studied to explain the pathogenesis of rhinosinusitis. Recently biofilms are emerging as an important cause. Biofilms are highly organized structures composed of a protective extracellular matrix and bacterial colonies, and provide the means for bacterial survival and virulence. Biofilms are known to be associated with intractable cases of rhinosinusitis and antibiotic resistance. Patients diagnosed with biofilm-related rhinosinusitis tend to suffer more severe disease that those without biofilms. Biofilm severity can also influence the prognosis of rhinosinusitis. We present two cases of pseudomonas-induced macroscopic biofilms (bioballs) of the maxillary sinuses. These bioballs cause intractable chronic rhinosinusitis as well, but unlike traditional biofilms, they can be surgically removed by endoscopy, and thus have a better prognosis than traditional biofilms. This is the first report of visible biofilms (bioballs) found in the maxillary sinuses.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Bacterial Ball as an Unusual Finding in Patients With Chronic Rhinosinusitis
Dong-Kyu Kim, Young Chan Wi, Su-Jin Shin, Youn Il Jang, Kyung Rae Kim, Seok Hyun Cho
Clin Exp Otorhinolaryngol. 2018;11(1):40-45. doi: 10.21053/ceo.2017.00332.Bacterial Ball in Concha Bullosa: Report of a Case With Unusual Location
Su-Jong Kim, Jee Won Moon, Yongmin Cho, Heung-Man Lee
Korean J Otorhinolaryngol-Head Neck Surg. 2023;66(5):335-339. doi: 10.3342/kjorl-hns.2021.01067.
Reference
-
References
1). Chung SK. Biofilm. J Rhinol. 2005; 12:5–9.2). Ferguson BJ, Stolz DB. Demonstration of biofilm in human bacterial chronic rhinosinusitis. Am J Rhinol. 2005; 19(5):452–7.
Article3). Sanclement JA, Webster P, Thomas J, Ramadan HH. Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis. Laryngoscope. 2005; 115(4):578–82.
Article4). Benninger MS, Ferguson BJ, Hadley JA, Hamilos DL, Jacobs M, Kennedy DW, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathology. Otolaryngol Head Neck Surg. 2003; 129(3):21–32.5). Prince AA, Steiger JD, Khalid AN, Dogrhamji L, Reger C, Eau Claire S, et al. Prevalence of biofilm-forming bacteria in chronic rhinosinusitis. Am J Rhinol. 2008; 22(3):239–45.
Article6). Psaltis AJ, Ha KR, Beule AG, Tan LW, Wormald PJ. Confocal scanning laser microscopy evidence of biofilms0 in patients with chronic rhinosinusitis. Laryngoscope. 2007; 117(7):1302–6.7). Christopher J., Paul S, Luanne HS, Garth DE. The role of biofilms in otolaryngologic infections. Curr Opin Otolaryngol Head Neck Surg. 2004; 12:185–90.8). Christian JH, Rizwan M, Dale HR. Biofilm and persistent inflammation in endoscopic sinus surgery. Otolaryngology-Head and Neck Surgery. 2010; 143:697–8.9). Cryer J, Schipor I, Perloff JR, et al. Evidence of bacterial biofilms in human chronic sinusitis. ORL J Otorhinolaryngol Relat Spec. 2004; 66:155–8.
Article10). Ferguson BJ, Stolz DB. Demonstration of biofilm in human bacterial chronic rhinosinusitis. Am J Rhinol. 2005; 19:452–7.
Article11). Sanderson AR, Leid JG, Hunsaker D. Bacterial biofilms on the sinus mucosa of human subjects with chronic rhinosinusitis. Laryngoscope. 2006; 116:1121–6.
Article12). Psaltis AJ, Weitzel EK, Ha KR, Wormald PJ. The effect of bacterial biofilms on post-sinus surgical outcomes. Am J Rhinol. 2008; 22:1–6.
Article13). Park YH, Kim EH, Seo ST, Lee SH, Kim JM, Koo BS. Formation of Biofilm in Patients with Chronic Otitis Media and Cholesteatoma. Korean J Otorhinolarygol. 2009; 52:124–8.
Article14). Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM. Microbial biofilms. Annu Rev Microbiol. 1995; 49:711–45.
Article15). Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999; 284(5418):1318–22.
Article16). Vlastarakos PV, Nikolopoulos TP, Maragoudakis P, Tzagaroulakis A, Ferekidis E. Biofilms in ear, nose, and throat infections: How important are they? Laryngoscope. 2007; 117(4):669–73.
Article17). Ymele-Leki P, Ross JM. Erosion from Staphylococcus aureus biofilms grown under physiologically relevant fluid shear forces yields bacterial cells with reduced avidity to collagen. Appl Environ Microbiol. 2007; 73(6):1834–41.18). Psaltis AJ, Ha KR, Beule AG, Tan LW, Wormald PJ. Confocal scanning laser microscopy evidence of biofilms in patients with chronic rhinosinusitis. Laryngoscope. 2007; 117(7):1302–6.
Article19). Sanclement JA, Webster P, Thomas J, Ramadan HH. Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis. Laryngoscope. 2005; 115(4):578–82.
Article20). Choi JW, Seo ST, Kim SG, Kim YM, Rha KS. The Demonstration of Bacterial Biofilm and It's Impact on Postoperative Course in Patients with Chronic Rhinosinusitis. Korean J Otorhinolaryngol. 2010; 53:349–53.
Article21). Khosravi Y, Ling LC, Loke MF, Shailendra S, Prepageran N, Vadi-velu J. Determination of the biofilm formation capacity of bacterial pathogens associated with otorhinolaryngologic diseases in the Ma-laysian population. Eur Arch Otorhinolaryngol. 2014; 271:1227–33.
Article22). Hayes SM, Howlin R, Johnston DA, et al. Intracellular residency of Staphylococcus aureus within mast cells in nasal polyps: A novel observation. J Allergy Clin Immunol. 2015; 135(6):1648–51.
Article23). Biel MA, Pedigo L, Gibbs A, Loebel N. Photodynamic therapy of antibiotic-resistant biofilms in a maxillary sinus model. Int Forum Allergy Rhinol. 2013; 3:468–73.
Article24). Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinol Suppl. 2012; 23:1–298.25). Min YG, Jung HW. Postoperative care of paranasal sinusitis. J Rhinol. 1995; 2:83–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Huge Pneumatized Uncinate Process Causing Obstruction in Patient with Chronic Rhinosinusitis
- Factors associated with chronic and recurrent rhinosinusitis in preschool children with obstructive sleep apnea syndrome
- Clinical Characteristics and Treatment of Fungal Rhinosinusitis
- Medical treatment according to phenotypes of chronic rhinosinusitis
- Predisposing Factors Associated With Chronic and Recurrent Rhinosinusitis in Childhood