Clin Exp Otorhinolaryngol.
2016 Jun;9(2):89-97. 10.21053/ceo.2014.01851.
The Efficacy of Corticosteroids in the Treatment of Peritonsillar Abscess: A Meta-Analysis
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea. yellobird@catholic.ac.kr
- KMID: 2165049
- DOI: http://doi.org/10.21053/ceo.2014.01851
Abstract
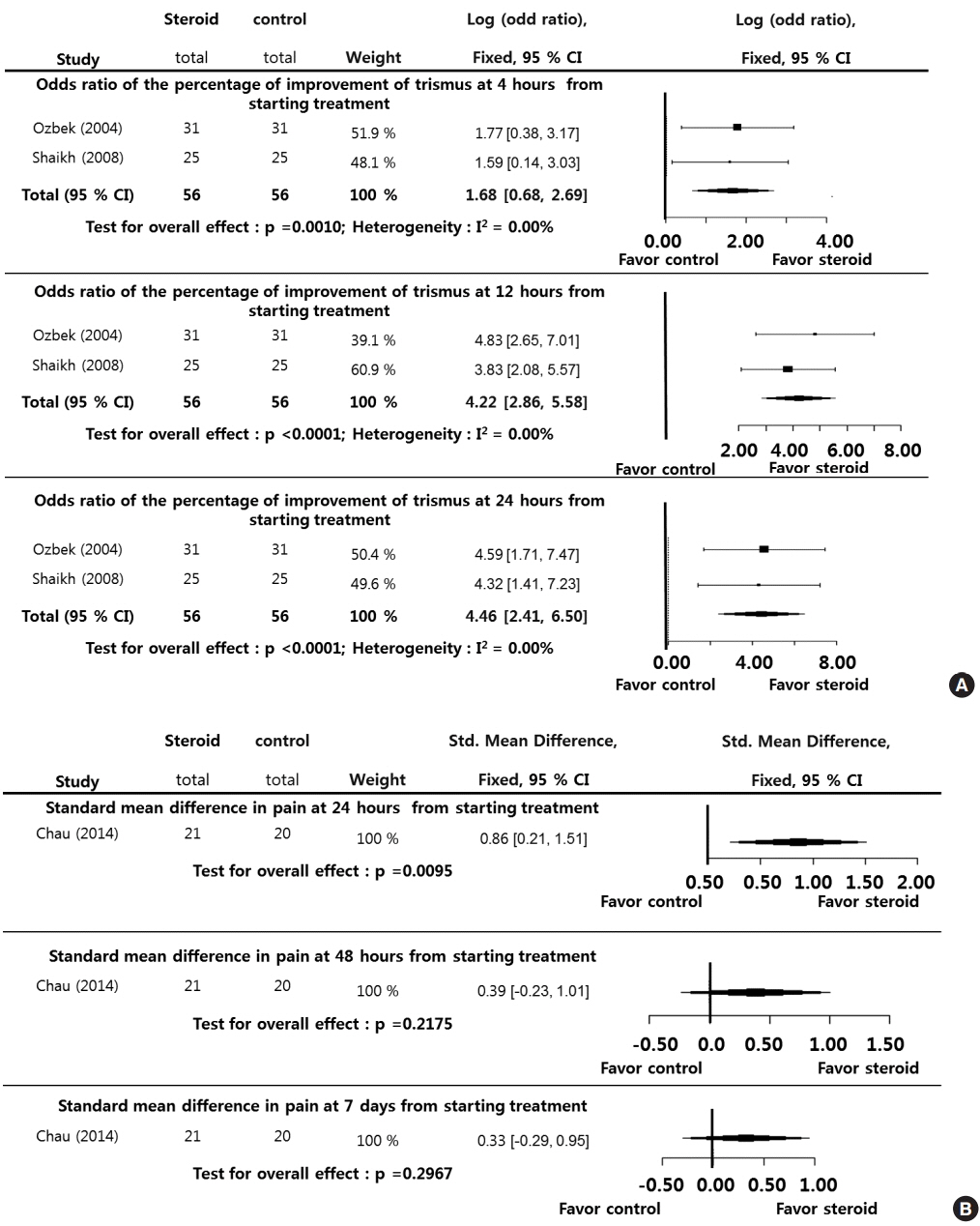
- Despite widespread use of antibiotics and surgical procedures for treating peritonsillar abscess (PTA), symptoms of severe inflammation such as pain and trismus during treatment result in patient dissatisfaction. The goal of this study was to perform a systematic review and meta-analysis of the efficacy of systemic steroids on the clinical course of PTA. Two reviewers independently searched the databases (MEDLINE, Scopus, and the Cochrane Database) from inception to December 2014. Studies comparing systemic administration of steroids (steroid group) with placebo (placebo group), where the outcomes of interest were pain, body temperature, hospitalization, and oral intake during the posttreatment period, were included. Baseline study characteristics, study quality data, numbers of patients in the steroid and control groups, and outcomes were extracted. Sufficient data for meta-analysis were retrieved for 3 trials with a total of 153 patients. Pain-related parameters (patient-reported scores and trismus), body temperature, and dysphagia during the first 24 hours after treatment were significantly improved in the steroid group compared with placebo group. The discharge rate during the first 5 days of the posttreatment period was significantly higher in the steroid group than the control group. However, although more patients in the steroid group returned to normal activities and dietary intake at 24 hours after treatment, the differences between the groups were not significant and disappeared after 48 hours. In the treatment of PTA, systemic administration of steroids with antibiotics could reduce pain-related symptoms, as well as provide a benefit with respect to the clinical course. However, further trials with well-designed research methodologies should be conducted to confirm our results.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Effects of Adjunctive Steroids in the Treatment of Peritonsillar Abscess
Junyong Choi, Dongsik Chang, Minwoo Kim, Jun Lee, Myoungsu Choi
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(8):563-567. doi: 10.3342/kjorl-hns.2020.00185.
Reference
-
1. Herzon FS, Harris P. Mosher Award thesis. Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope. 1995; Aug. 105(8 Pt 3 Suppl 74):1–17.2. Johnson RF, Stewart MG, Wright CC. An evidence-based review of the treatment of peritonsillar abscess. Otolaryngol Head Neck Surg. 2003; Mar. 128(3):332–43.
Article3. Steyer TE. Peritonsillar abscess: diagnosis and treatment. Am Fam Physician. 2002; Jan. 65(1):93–6.4. Khayr W, Taepke J. Management of peritonsillar abscess: needle aspiration versus incision and drainage versus tonsillectomy. Am J Ther. 2005; Jul-Aug. 12(4):344–50.5. Galioto NJ. Peritonsillar abscess. Am Fam Physician. 2008; Jan. 77(2):199–202.6. Hayward G, Thompson M, Heneghan C, Perera R, Del Mar C, Glasziou P. Corticosteroids for pain relief in sore throat: systematic review and meta-analysis. BMJ. 2009; Aug. 339:b2976.
Article7. van Cauwenberge P, Van Hoecke H, Vandenbulcke L, Van Zele T, Bachert C. Glucocorticosteroids in allergic inflammation: clinical benefits in allergic rhinitis, rhinosinusitis, and otitis media. Immunol Allergy Clin North Am. 2005; Aug. 25(3):489–509.
Article8. Lamkin RH, Portt J. An outpatient medical treatment protocol for peritonsillar abscess. Ear Nose Throat J. 2006; Oct. 85(10):658. 660.
Article9. Ozbek C, Aygenc E, Tuna EU, Selcuk A, Ozdem C. Use of steroids in the treatment of peritonsillar abscess. J Laryngol Otol. 2004; Jun. 118(6):439–42.
Article10. Shaikh KR. Treatment of peritonsillar abscess and role of steriods. J Liaquat Univ Med Health Sci. 2008; Jan-Apr. 7(1):31–3.11. Chau JK, Seikaly HR, Harris JR, Villa-Roel C, Brick C, Rowe BH. Corticosteroids in peritonsillar abscess treatment: a blinded placebo-controlled clinical trial. Laryngoscope. 2014; Jan. 124(1):97–103.
Article12. Powell EL, Powell J, Samuel JR, Wilson JA. A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation. J Antimicrob Chemother. 2013; Sep. 68(9):1941–50.
Article13. Cope D, Bova R. Steroids in otolaryngology. Laryngoscope. 2008; Sep. 118(9):1556–60.
Article14. Acion L, Peterson JJ, Temple S, Arndt S. Probabilistic index: an intuitive non-parametric approach to measuring the size of treatment effects. Stat Med. 2006; Feb. 25(4):591–602.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Peritonsillar Abscess Following Tonsillectomy
- Peritonsillar Abscess in a 40-Day-Old Infant
- Diagnosis of Peritonsillar Abscess Using Gray Scale Image and Color DopplerImage of Intraoral Ultrasonography
- Diagnosis and Treatment of Peritonsillar Abscess with Single Enhanced Computed Tomography
- Peritonsillar Involvement in Pyoderma Gangrenosum associated with Ulcerative Colitis