Intest Res.
2014 Apr;12(2):153-156. 10.5217/ir.2014.12.2.153.
Peritonsillar Involvement in Pyoderma Gangrenosum associated with Ulcerative Colitis
- Affiliations
-
- 1Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea. leejun@chosun.ac.kr
- KMID: 2284901
- DOI: http://doi.org/10.5217/ir.2014.12.2.153
Abstract
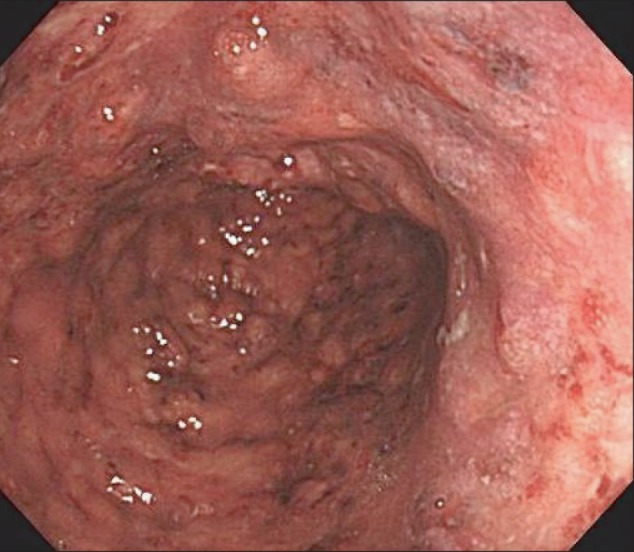
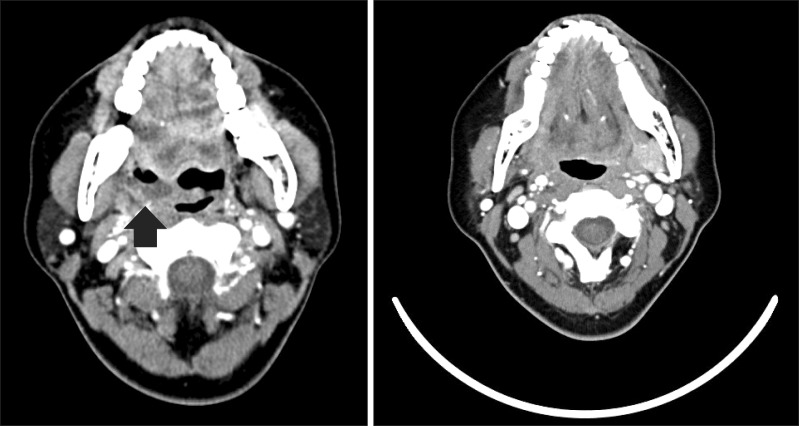
- Peritonsillar abscess is a common deep throat infection. Early diagnosis and prompt, appropriate management of a peritonsillar abscess prevents mortality. A 45-year-old woman on steroids for an ulcerative colitis (UC) exacerbation presented with sore throat and multiple skin ulcers on her left forearm and right foot. Computed tomography of the neck revealed a peritonsillar abscess. Gram staining and culture of the abscess were negative, and a skin biopsy suggested pyoderma gangrenosum (PG). The final diagnosis was peritonsillar involvement of steroid-refractory PG-associated UC. The patient showed a complete response to infliximab. Here, we report a case of successful infliximab treatment for peritonsillar involvement of steroid-refractory PG-associated UC.
MeSH Terms
Figure
Cited by 1 articles
-
Multiple Pyoderma Gangrenosum in Ulcerative Colitis
Sung Bum Kim, Si Hyung Lee
Korean J Gastroenterol. 2018;72(3):155-158. doi: 10.4166/kjg.2018.72.3.155.
Reference
-
1. Johnson JL, West DA, Haggstrom AN. Pyoderma gangrenosum associated with an aseptic splenic abscess in a patient with neurofibromatosis. Pediatr Dermatol. doi: 10.1111/pde.12129. Published online ahead of print 28 March 2013.
Article2. Allen CP, Hull J, Wilkison N, Burge SM. Pediatric pyoderma gangrenosum with splenic and pulmonary involvement. Pediatr Dermatol. 2013; 30:497–499. PMID: 23627664.
Article3. Tavarela Veloso F. Review article: skin complications associated with inflammatory bowel disease. Aliment Pharmacol Ther. 2004; 20(Suppl 4):50–53. PMID: 15352894.5. von den Driesch P. Pyoderma gangrenosum: a report of 44 cases with follow-up. Br J Dermatol. 1997; 137:1000–1005. PMID: 9470924.
Article6. Crowson AN, Mihm MC Jr, Magro C. Pyoderma gangrenosum: a review. J Cutan Pathol. 2003; 30:97–107. PMID: 12641787.
Article7. Yoo YW, Jung SH, Lee YJ, et al. A case of pyoderma gangrenosum associated with ulcerative colitis. Intest Res. 2008; 6:80–84.8. Van Assche G, Dignass A, Bokemeyer B, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013; 7:1–33. PMID: 23040453.
Article9. Paramkusam G, Meduri V, Gangeshetty N. Pyoderma gangrenosum with oral involvement - case report and review of the literature. Int J Oral Sci. 2010; 2:111–116. PMID: 20737938.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Post-traumatic Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Pyoderma Gangrenosum Associated with Ulcerative Colitis
- Multiple Pyoderma Gangrenosum in Ulcerative Colitis
- A Case of Simultaneous Presentation of Bullous and Ulcerative Types of Pyoderma Gangrenosum in an Ulcerative Colitis Patient
- Saddle Nose Deformity as a Result of an Aseptic Nasal Abscess Accompanied by Ulcerative Colitis and Pyoderma Gangrenosum