Blood Res.
2015 Dec;50(4):242-247. 10.5045/br.2015.50.4.242.
Intraocular lymphoma in Korea: the Consortium for Improving Survival of Lymphoma (CISL) study
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea. drosy@dau.ac.kr
- 2Division of Hematology-Oncology, Department of Medicine, Seonam University of Medicine Myongji Hospital, Goyang, Korea.
- 3Department of Internal Medicine, Yonsei University College of Medicine, Severance Hospital, Seoul, Korea.
- 4Division of Hematology/Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Ophthalmology, Dong-A University College of Medicine, Busan, Korea.
- 6Department of Ophthalmology, Gyeongsang National University School of Medicine and Gyeongsang National University Hospital, Jinju, Korea.
- 7Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- 8Department of Hemato-Oncology, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 9Department of Hemato-Oncology, Korea Institute of Radiological and Medical Sciences, Seoul, Korea.
- 10Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. csuh@amc.seoul.kr
- KMID: 2133759
- DOI: http://doi.org/10.5045/br.2015.50.4.242
Abstract
- BACKGROUND
Intraocular lymphoma (IOL) is a rare malignant lymphoma that most closely resembles a diffuse large B-cell lymphoma, and it is a subtype of primary central nervous system lymphoma (PCNSL). IOL is located inside the eye in the retina, uvea, and/or optic nerve. We retrospectively analyzed IOL patient data to identify treatment patterns and survival rates in Korea.
METHODS
Cytological confirmation for a diagnosis of IOL was performed for all patients. The clinical data collected from medical records included Ann Arbor stage, International Prognostic Index, performance status, date of diagnosis, treatment modality and response, date of relapse, and date of last follow-up.
RESULTS
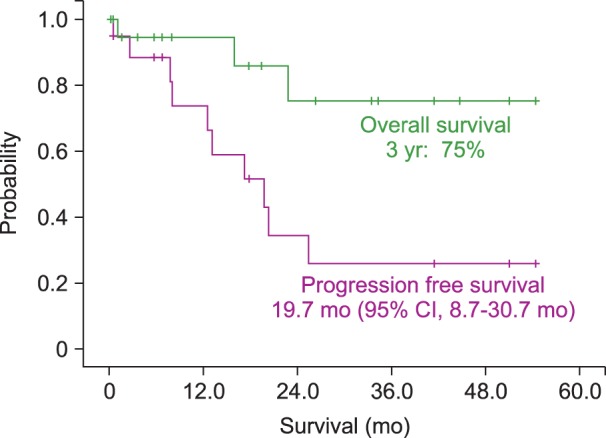
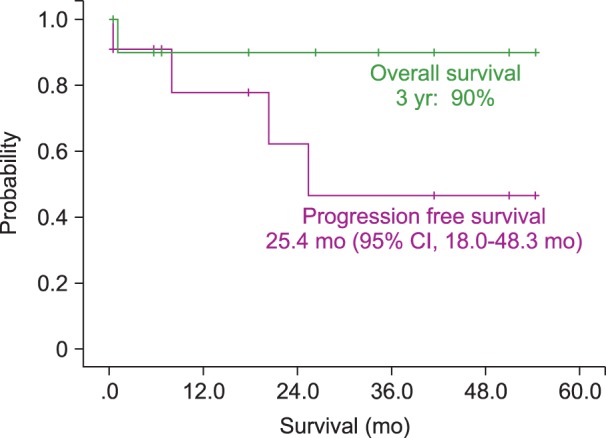
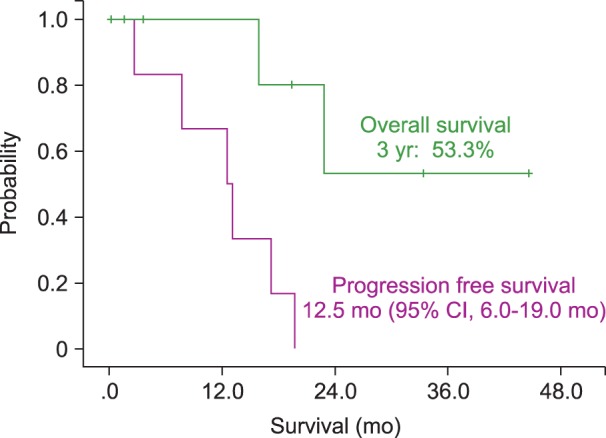
Twenty patients who were diagnosed with IOL, between December 2007 and June 2014 at multiple centers in Korea, were included in the analysis. Four patients were diagnosed with IOL alone, not involving the CNS. Two patients with isolated IOL later developed PCNSL. Nine patients developed CNS lesions before the onset of ocular lymphoma. Five patients had simultaneous onset in the eye and CNS. Twelve patients were treated by intravitreal injection of methotrexate for IOL. The median progression-free survival (PFS) for patients was 19.7 months (95% CI, 8.7-30.7 mo). The estimated 3-year overall survival (OS) for all patients was 75.1%.
CONCLUSION
Treatment for IOL patients included radiotherapy and intraocular chemotherapy. IOL patients showed favorable PFS and OS. These patients would require long-term follow-up to identify relapse and adverse effects of radiotherapy or intraocular chemotherapy.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Consortium for Improving Survival of Lymphoma (CISL): recent achievements and future perspective
Cheolwon Suh, Byeong-Bae Park, Won Seog Kim
Blood Res. 2017;52(1):3-6. doi: 10.5045/br.2017.52.1.3.Consortium for Improving Survival of Lymphoma (CISL): a model of multicenter collaboration for lymphoma studies in Korea
Seok Jin Kim
Blood Res. 2015;50(4):187-188. doi: 10.5045/br.2015.50.4.187.
Reference
-
1. Stübiger N, Kakkassery V, Gundlach E, Winterhalter S, Pleyer U. Diagnostics and treatment of primary vitreoretinal lymphoma. Ophthalmologe. 2015; 112:223–230. PMID: 25698590.2. Levasseur SD, Wittenberg LA, White VA. Vitreoretinal lymphoma: a 20-year review of incidence, clinical and cytologic features, treatment, and outcomes. JAMA Ophthalmol. 2013; 131:50–55. PMID: 23307208.4. Cooper EL, Riker JL. Malignant lymphoma of the uveal tract. Am J Ophthalmol. 1951; 34:1153–1158. PMID: 14857107.
Article5. Kimura K, Usui Y, Goto H. Japanese Intraocular Lymphoma Study Group. Clinical features and diagnostic significance of the intraocular fluid of 217 patients with intraocular lymphoma. Jpn J Ophthalmol. 2012; 56:383–389. PMID: 22661396.
Article6. Chan CC, Wallace DJ. Intraocular lymphoma: update on diagnosis and management. Cancer Control. 2004; 11:285–295. PMID: 15377987.
Article7. Chan CC, Buggage RR, Nussenblatt RB. Intraocular lymphoma. Curr Opin Ophthalmol. 2002; 13:411–418. PMID: 12441846.
Article8. Mulay K, Narula R, Honavar SG. Primary vitreoretinal lymphoma. Indian J Ophthalmol. 2015; 63:180–186. PMID: 25971162.
Article9. Grimm SA, Pulido JS, Jahnke K, et al. Primary intraocular lymphoma: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Ann Oncol. 2007; 18:1851–1855. PMID: 17804469.
Article10. Suh C, Kim WS, Kim JS, Park BB. Review of the clinical research conducted by the Consortium for Improving Survival of Lymphoma of the Korean Society of Hematology Lymphoma Working Party. Blood Res. 2013; 48:171–177. PMID: 24086936.
Article11. Hoffman PM, McKelvie P, Hall AJ, Stawell RJ, Santamaria JD. Intraocular lymphoma: a series of 14 patients with clinicopathological features and treatment outcomes. Eye (Lond). 2003; 17:513–521. PMID: 12802353.
Article12. Freeman LN, Schachat AP, Knox DL, Michels RG, Green WR. Clinical features, laboratory investigations, and survival in ocular reticulum cell sarcoma. Ophthalmology. 1987; 94:1631–1639. PMID: 3323986.
Article13. Klingele TG, Hogan MJ. Ocular reticulum cell sarcoma. Am J Ophthalmol. 1975; 79:39–47. PMID: 1089097.
Article14. Ohta K, Sano K, Imai H, Kikuchi T. Cytokine and molecular analyses of intraocular lymphoma. Ocul Immunol Inflamm. 2009; 17:142–147. PMID: 19585355.
Article15. Merle-Béral H, Davi F, Cassoux N, et al. Biological diagnosis of primary intraocular lymphoma. Br J Haematol. 2004; 124:469–473. PMID: 14984496.
Article16. Wolf LA, Reed GF, Buggage RR, Nussenblatt RB, Chan CC. Vitreous cytokine levels. Ophthalmology. 2003; 110:1671–1672. PMID: 12917196.
Article17. Baehring JM, Androudi S, Longtine JJ, et al. Analysis of clonal immunoglobulin heavy chain rearrangements in ocular lymphoma. Cancer. 2005; 104:591–597. PMID: 15973665.
Article18. Pe'er J, Hochberg FH, Foster CS. Clinical review: treatment of vitreoretinal lymphoma. Ocul Immunol Inflamm. 2009; 17:299–306. PMID: 19831557.19. Smith JR, Rosenbaum JT, Wilson DJ, et al. Role of intravitreal methotrexate in the management of primary central nervous system lymphoma with ocular involvement. Ophthalmology. 2002; 109:1709–1716. PMID: 12208721.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of the clinical research conducted by the Consortium for Improving Survival of Lymphoma of the Korean Society of Hematology Lymphoma Working Party
- Consortium for Improving Survival of Lymphoma (CISL): a model of multicenter collaboration for lymphoma studies in Korea
- Organ-specific considerations for marginal zone lymphomas in Korea, based on Consortium for Improving Survival of Lymphoma (CISL) and Korean clinical studies
- The Consortium for Improving Survival of Lymphoma (CISL): recent achievements and future perspective
- Primary Intraocular T-cell Lymphoma