J Korean Med Sci.
2014 Oct;29(10):1391-1397. 10.3346/jkms.2014.29.10.1391.
Impact of Framingham Risk Score, Flow-Mediated Dilation, Pulse Wave Velocity, and Biomarkers for Cardiovascular Events in Stable Angina
- Affiliations
-
- 1Cardiovascular Division, Department of Internal Medicine, Hallym University Medical Center, Anyang, Korea. pkhmd@naver.com
- KMID: 2129630
- DOI: http://doi.org/10.3346/jkms.2014.29.10.1391
Abstract
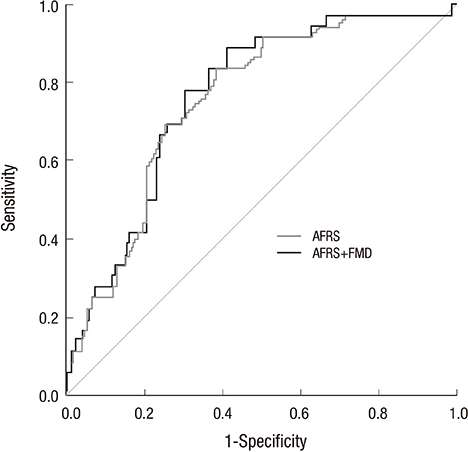
- Although the age-adjusted Framingham risk score (AFRS), flow-mediated dilation (FMD), brachial-ankle pulse wave velocity (baPWV), high-sensitivity C-reactive protein (hsCRP), fibrinogen, homocysteine, and free fatty acid (FFA) can predict future cardiovascular events (CVEs), a comparison of these risk assessments for patients with stable angina has not been reported. We enrolled 203 patients with stable angina who had been scheduled for coronary angiography (CAG). After CAG, 134 patients showed significant coronary artery disease. During 4.2 yr follow-up, 36 patients (18%) showed CVEs, including myocardial infarction, de-novo coronary artery revascularization, in-stent restenosis, stroke, and cardiovascular death. ROC analysis showed that AFRS, FMD, baPWV, and hsCRP could predict CVEs (with AUC values of 0.752, 0.707, 0.659, and 0.702, respectively, all P<0.001 except baPWV P=0.003). A Cox proportional hazard analysis showed that AFRS and FMD were independent predictors of CVEs (HR, 2.945; 95% CI, 1.572-5.522; P=0.001 and HR, 0.914; 95% CI, 0.826-0.989; P=0.008, respectively). However, there was no difference in predictive power between combining AFRS plus FMD and AFRS alone (AUC 0.752 vs. 0.763; z=1.358, P=0.175). In patients with stable angina, AFRS and FMD are independent predictors of CVEs. However, there is no additive value of FMD on the AFRS in predicting CVEs.
MeSH Terms
-
Adult
Aged
Angina, Stable/*physiopathology
Biological Markers/analysis/blood
Blood Flow Velocity
Coronary Artery Disease/*diagnosis
Endothelium, Vascular
Female
Heart/*physiopathology
Humans
Male
Middle Aged
Myocardial Infarction/physiopathology
Predictive Value of Tests
Proportional Hazards Models
Pulsatile Flow
Pulse Wave Analysis/*methods
ROC Curve
Risk Assessment
Risk Factors
Biological Markers
Figure
Cited by 1 articles
-
Potential Risk Factors Associated With Vascular Diseases in Patients Receiving Treatment for Hypertension
Hyunjung Kim, Joonhong Park, Hyojin Chae, Gun Dong Lee, Sang Yoon Lee, Jong Min Lee, Yong-Seog Oh, Myungshin Kim, Yonggoo Kim
Ann Lab Med. 2016;36(3):215-222. doi: 10.3343/alm.2016.36.3.215.
Reference
-
1. Neunteufl T, Katzenschlager R, Hassan A, Klaar U, Schwarzacher S, Glogar D, Bauer P, Weidinger F. Systemic endothelial dysfunction is related to the extent and severity of coronary artery disease. Atherosclerosis. 1997; 129:111–118.2. Kitta Y, Obata JE, Nakamura T, Hirano M, Kodama Y, Fujioka D, Saito Y, Kawabata K, Sano K, Kobayashi T, et al. Persistent impairment of endothelial vasomotor function has a negative impact on outcome in patients with coronary artery disease. J Am Coll Cardiol. 2009; 53:323–330.3. Yamashina A, Tomiyama H, Arai T, Hirose K, Koji Y, Hirayama Y, Yamamoto Y, Hori S. Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens Res. 2003; 26:615–622.4. Orlova IA, Nuraliev EY, Yarovaya EB, Ageev FT. Prognostic value of changes in arterial stiffness in men with coronary artery disease. Vasc Health Risk Manag. 2010; 6:1015–1021.5. de Ferranti S, Rifai N. C-reactive protein and cardiovascular disease: a review of risk prediction and interventions. Clin Chim Acta. 2002; 317:1–15.6. Gach O, Legrand V, Biessaux Y, Chapelle JP, Vanbelle S, Pierard LA. Long-term prognostic significance of high-sensitivity C-reactive protein before and after coronary angioplasty in patients with stable angina pectoris. Am J Cardiol. 2007; 99:31–35.7. Fibrinogen Studies Collaboration. Danesh J, Lewington S, Thompson SG, Lowe GD, Collins R, Kostis JB, Wilson AC, Folsom AR, Wu K, et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA. 2005; 294:1799–1809.8. Homocysteine Studies Collaboration. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002; 288:2015–2022.9. Breitling LP, Rothenbacher D, Grandi NC, März W, Brenner H. Prognostic usefulness of free fatty acids in patients with stable coronary heart disease. Am J Cardiol. 2011; 108:508–513.10. Grundy SM, Balady GJ, Criqui MH, Fletcher G, Greenland P, Hiratzka LF, Houston-Miller N, Kris-Etherton P, Krumholz HM, LaRosa J, et al. Primary prevention of coronary heart disease: guidance from Framingham. A statement for healthcare professionals from the AHA Task Force on Risk Reduction. Circulation. 1998; 97:1876–1887.11. von Birgelen C, Hartmann M, Mintz GS, van Houwelingen KG, Deppermann N, Schmermund A, Böse D, Eggebrecht H, Neumann T, Gössl M, et al. Relationship between cardiovascular risk as predicted by established risk scores versus plaque progression as measured by serial intravascular ultrasound in left main coronary arteries. Circulation. 2004; 110:1579–1585.12. Pencina MJ, D'Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the Framingham heart study. Circulation. 2009; 119:3078–3084.13. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39:257–265.14. Wilson PW, Nam BH, Pencina M, D'Agostino RB Sr, Benjamin EJ, O'Donnell CJ. C-reactive protein and risk of cardiovascular disease in men and women from the Framingham Heart Study. Arch Intern Med. 2005; 165:2473–2478.15. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.16. Troche CJ, Tacke J, Hinzpeter B, Danner M, Lauterbach KW. Cost-effectiveness of primary and secondary prevention in cardiovascular diseases. Eur Heart J. 1998; 19:C59–C65.17. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, Ebrahim S, Faergeman O, Graham I, Mancia G, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2003; 24:1601–1610.18. Lopes NH, Paulitsch Fda S, Gois AF, Pereira AC, Stolf NA, Dallan LO, Ramires JA, Hueb WA. Impact of number of vessels disease on outcome of patients with stable coronary artery disease: 5-year follow-up of the Medical, Angioplasty, and bypass Surgery study (MASS). Eur J Cardiothorac Surg. 2008; 33:349–354.19. Ryan TJ, Faxon DP, Gunnar RM, Kennedy JW, King SB 3rd, Loop FD, Peterson KL, Reeves TJ, Williams DO, Winters WL Jr, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation. 1988; 78:486–502.20. Smith SC Jr, Blair SN, Criqui MH, Fletcher GF, Fuster V, Gersh BJ, Gotto AM, Gould KL, Greenland P, Grundy SM, et al. Preventing heart attack and death in patients with coronary disease. Circulation. 1995; 92:2–4.21. Grover SA, Paquet S, Levinton C, Coupal L, Zowall H. Estimating the benefits of modifying risk factors of cardiovascular disease: a comparison of primary vs secondary prevention. Arch Intern Med. 1998; 158:655–662.22. Genest J, Pedersen TR. Prevention of cardiovascular ischemic events: high-risk and secondary prevention. Circulation. 2003; 107:2059–2065.23. Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE. Endothelium-dependent dilation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol. 1994; 24:1468–1474.24. Anderson TJ. Prognostic significance of brachial flow-mediated vasodilation. Circulation. 2007; 115:2373–2375.25. Patti G, Pasceri V, Melfi R, Goffredo C, Chello M, D'Ambrosio A, Montesanti R, Di Sciascio G. Impaired flow-mediated dilation and risk of restenosis in patients undergoing coronary stent implantation. Circulation. 2005; 111:70–75.26. Witte DR, Westerink J, de Koning EJ, van der Graaf Y, Grobbee DE, Bots ML. Is the association between flow-mediated dilation and cardiovascular risk limited to low-risk populations? J Am Coll Cardiol. 2005; 45:1987–1993.27. Tomiyama H, Koji Y, Yambe M, Shiina K, Motobe K, Yamada J, Shido N, Tanaka N, Chikamori T, Yamashina A. Brachial -- ankle pulse wave velocity is a simple and independent predictor of prognosis in patients with acute coronary syndrome. Circ J. 2005; 69:815–822.28. Park KH, Kim MK, Kim HS, Park WJ, Cho GY, Choi YJ. Clinical significance of Framingham risk score, flow-mediated dilation and pulse wave velocity in patients with stable angina. Circ J. 2011; 75:1177–1183.29. Ridker PM. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: moving an inflammatory hypothesis toward consensus. J Am Coll Cardiol. 2007; 49:2129–2138.30. Rana JS, Cote M, Després JP, Sandhu MS, Talmud PJ, Ninio E, Wareham NJ, Kastelein JJ, Zwinderman AH, Khaw KT, et al. Inflammatory biomarkers and the prediction of coronary events among people at intermediate risk: the EPIC-Norfolk prospective population study. Heart. 2009; 95:1682–1687.31. Folsom AR, Chambless LE, Ballantyne CM, Coresh J, Heiss G, Wu KK, Boerwinkle E, Mosley TH Jr, Sorlie P, Diao G, et al. An assessment of incremental coronary risk prediction using C-reactive protein and other novel risk markers: the atherosclerosis risk in communities study. Arch Intern Med. 2006; 166:1368–1373.32. Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, Jacques PF, Rifai N, Selhub J, Robins SJ, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006; 355:2631–2639.33. Soga J, Nishioka K, Nakamura S, Umemura T, Jitsuiki D, Hidaka T, Teragawa H, Takemoto H, Goto C, Yoshizumi M, et al. Measurement of flow-mediated vasodilation of the brachial artery: a comparison of measurements in the seated and supine positions. Circ J. 2007; 71:736–740.34. Warnholtz A, Wild P, Ostad MA, Elsner V, Stieber F, Schinzel R, Walter U, Peetz D, Lackner K, Blankenberg S, et al. Effects of oral niacin on endothelial dysfunction in patients with coronary artery disease: results of the randomized, double-blind, placebo-controlled INEF study. Atherosclerosis. 2009; 204:216–221.35. Kuvin JT, Patel AR, Sliney KA, Pandian NG, Rand WM, Udelson JE, Karas RH. Peripheral vascular endothelial function testing as a noninvasive indicator of coronary artery disease. J Am Coll Cardiol. 2001; 38:1843–1849.36. Treasure CB, Klein JL, Weintraub WS, Talley JD, Stillabower ME, Kosinski AS, Zhang J, Boccuzzi SJ, Cedarholm JC, Alexander RW. Beneficial effects of cholesterol-lowering therapy on the coronary endothelium in patients with coronary artery disease. N Engl J Med. 1995; 332:481–487.37. Rajagopalan S, Harrison DG. Reversing endothelial dysfunction with ACE inhibitors: a new trend. Circulation. 1996; 94:240–243.38. Sola S, Mir MQ, Cheema FA, Khan-Merchant N, Menon RG, Parthasarathy S, Khan BV. Irbesartan and lipoic acid improve endothelial function and reduce markers of inflammation in the metabolic syndrome: results of the Irbesartan and Lipoic Acid in Endothelial Dysfunction (ISLAND) study. Circulation. 2005; 111:343–348.39. Modena MG, Bonetti L, Coppi F, Bursi F, Rossi R. Prognostic role of reversible endothelial dysfunction in hypertensive postmenopausal women. J Am Coll Cardiol. 2002; 40:505–510.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-invasive Methods for Cardiovascular Risk Assessment in Asymptomatic Type 2 Diabetes Mellitus
- The Relation of Pulse Wave Velocity with Framingham Risk Score and SCORE Risk Score
- Imaging Markers of Subclinical Atherosclerosis
- Association Between Arterial Stiffness and Carotid Atherosclerosis in the Elderly
- Association Between the extent of Subclinical Atheroscelrosis and Pulse Wave Velocity in the Elderly