Korean J Urol.
2011 Oct;52(10):674-680. 10.4111/kju.2011.52.10.674.
Effect of Prostate Biopsy Hemorrhage on MRDW and MRS Imaging
- Affiliations
-
- 1Department of Urology, Chung-Ang University College of Medicine, Seoul, Korea. caucih@cau.ac.kr
- 2Department of Radiology, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2061429
- DOI: http://doi.org/10.4111/kju.2011.52.10.674
Abstract
- PURPOSE
To retrospectively evaluate the effect of post-prostate-biopsy hemorrhage on the interpretation of magnetic resonance diffusion-weighted (MRDW) and magnetic resonance spectroscopic (MRS) imaging in the detection of prostate cancer. We also investigated the optimal timing for magnetic resonance examination after prostate biopsy.
MATERIALS AND METHODS
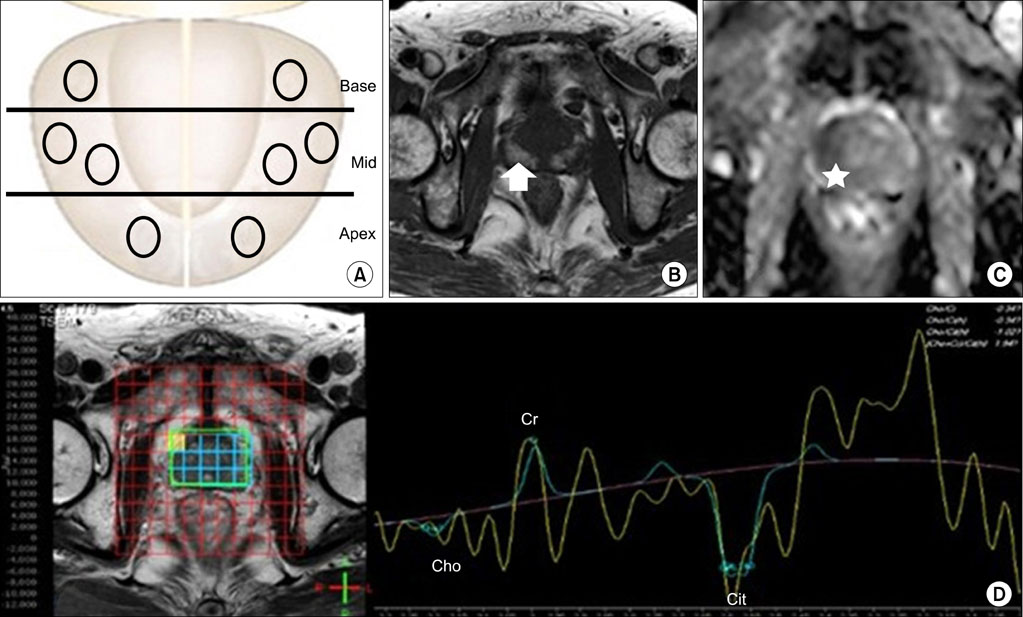
We reviewed the records of 135 men. All patients underwent prostate magnetic resonance imaging (MRI). The prostate was divided into eight regions according to the biopsy site. Subsequently, we measured hemorrhage on apparent diffusion coefficient (ADC) values and (choline+creatinine)/citrate ([Cho+Cr]/Cit) ratios in the same regions on the MRI. We investigated the effect of hemorrhage at ADC values and (Cho+Cr)/Cit ratios on MRI and the relationship between prostate biopsy results and MRI findings.
RESULTS
The mean patient age was 68.7 years and the mean time between biopsy and MRI was 23.5 days. The total hemorrhagic score demonstrated no significant associations with intervals from biopsy to MRI. Higher hemorrhagic scores were associated with higher ADC values, prostate cancer, and noncancer groups, respectively (p<0.001). ADC values were lower in tumors than in normal tissue (p<0.001), and ADC values were inversely correlated with tumor Gleason score in biopsy cores (p<0.001). However, (Cho+Cr)/Cit ratios did not exhibit any association with prostate biopsy results and hemorrhage.
CONCLUSIONS
Hemorrhage had no significant associations with the interval from biopsy to MRI. ADC values may help to detect prostate cancer and predict the aggressiveness of cancer; however, it is important to consider the bias effect of hemorrhage on the interpretation of MRDW imaging given that hemorrhage affects ADC values.
Keyword
MeSH Terms
Figure
Reference
-
1. Levi F, Lucchini F, Negri E, Boyle P, La Vecchia C. Leveling of prostate cancer mortality in Western Europe. Prostate. 2004. 60:46–52.2. Bangma CH, Kranse R, Blijenberg BG, Schrőder FH. The value of screening tests in the detection of prostate cancer. Part I: Results of a retrospective evaluation of 1726 men. Urology. 1995. 46:773–778.3. Pepe P, Panella P, D'Arrigo L, Savoca F, Pennisi M, Aragona F. Should men with serum prostate-specific antigen < or =4 ng/ml and normal digital rectal examination undergo a prostate biopsy? A literature review. Oncology. 2006. 70:81–89.4. Schiebler ML, Schnall MD, Pollack HM, Lenkinski RE, Tomaszewski JE, Wein AJ, et al. Current role of MR imaging in the staging of adenocarcinoma of the prostate. Radiology. 1993. 189:339–352.5. White S, Hricak H, Forstner R, Kurhanewicz J, Vigneron DB, Zaloudek CJ, et al. Prostate cancer: effect of postbiopsy hemorrhage on interpretation of MR images. Radiology. 1995. 195:385–390.6. Westphalen AC, Coakley FV, Qayyum A, Swanson M, Simko JP, Lu Y, et al. Peripheral zone prostate cancer: accuracy of different interpretative approaches with MR and MR spectroscopic imaging. Radiology. 2008. 246:177–184.7. Bostwick DG, Graham SD Jr, Napalkov P, Abrahamsson PA, di Sant'agnese PA, Algaba F, et al. Staging of early prostate cancer: a proposed tumor volume-based prognostic index. Urology. 1993. 41:403–411.8. Park SY, Kim JJ, Kim TH, Lim SH, Han DH, Park BK, et al. The role of endorectal magnetic resonance imaging in predicting extraprostatic extension and seminal vesicle invasion in clinically localized prostate cancer. Korean J Urol. 2010. 51:308–312.9. Casciani E, Gualdi GF. Prostate cancer: value of magnetic resonance spectroscopy 3D chemical shift imaging. Abdom Imaging. 2006. 31:490–499.10. Kurhanewicz J, Vigneron DB, Hricak H, Narayan P, Carroll P, Nelson SJ. Three-dimensional H-1 MR spectroscopic imaging of the in situ human prostate with high (0.24-0.7-cm3) spatial resolution. Radiology. 1996. 198:795–805.11. Yacoe ME, Sommer G, Peehl D. In vitro proton spectroscopy of normal and abnormal prostate. Magn Reson Med. 1991. 19:429–438.12. Lee KC, Sud S, Meyer CR, Moffat BA, Chenevert TL, Rehemtulla A, et al. An imaging biomarker of early treatment response in prostate cancer that has metastasized to the bone. Cancer Res. 2007. 67:3524–3528.13. Tamada T, Sone T, Jo Y, Yamamoto A, Yamashita T, Egashira N, et al. Prostate cancer: relationships between postbiopsy hemorrhage and tumor detectability at MR diagnosis. Radiology. 2008. 248:531–539.14. Hong SK, Kim DS, Lee WK, Park H, Kim JK, Doo SH, et al. Significance of postbiopsy hemorrhage observed on preoperative magnetic resonance imaging in performing robot-assisted laparoscopic radical prostatectomy. World J Urol. 2010. 28:721–726.15. Schiebler ML, Tomaszewski JE, Bezzi M, Pollack HM, Kressel HY, Cohen EK, et al. Prostatic carcinoma and benign prostatic hyperplasia: correlation of high-resolution MR and histopathologic findings. Radiology. 1989. 172:131–137.16. Ikonen S, Karkkainen P, Kivisaari L, Salo JO, Taari K, Vehmas T, et al. Magnetic resonance imaging of prostatic cancer: does detection vary between high and low gleason score tumors? Prostate. 2000. 43:43–48.17. Stokes SH, Real JD, Adams PW, Clements JC, Wuertzer S, Kan W. Transperineal ultrasound-guided radioactive seed implantation for organ-confined carcinoma of the prostate. Int J Radiat Oncol Biol Phys. 1997. 37:337–341.18. Amin Z, Lees WR, Bown SG. Technical note: interstitial laser photocoagulation for the treatment of prostatic cancer. Br J Radiol. 1993. 66:1044–1047.19. Lee F, Bahn DK, McHugh TA, Onik GM, Lee FT Jr. US-guided percutaneous cryoablation of prostate cancer. Radiology. 1994. 192:769–776.20. Chodak GW, Thisted RA, Gerber GS, Johansson JE, Adolfsson J, Jones GW, et al. Results of conservative management of clinically localized prostate cancer. N Engl J Med. 1994. 330:242–248.21. Douketis JD. Perioperative anticoagulation management in patients who are receiving oral anticoagulant therapy: a practical guide for clinicians. Thromb Res. 2002. 108:3–13.22. Ikonen S, Kivisaari L, Vehmas T, Tervahartiala P, Salo JO, Taari K, et al. Optimal timing of post-biopsy MR imaging of the prostate. Acta Radiol. 2001. 42:70–73.23. Qayyum A, Coakley FV, Lu Y, Olpin JD, Wu L, Yeh BM, et al. Organ-confined prostate cancer: effect of prior transrectal biopsy on endorectal MRI and MR spectroscopic imaging. AJR Am J Roentgenol. 2004. 183:1079–1083.24. Gibbs P, Pickles MD, Turnbull LW. Diffusion imaging of the prostate at 3.0 tesla. Invest Radiol. 2006. 41:185–188.25. Pickles MD, Gibbs P, Sreenivas M, Turnbull LW. Diffusion-weighted imaging of normal and malignant prostate tissue at 3.0T. J Magn Reson Imaging. 2006. 23:130–134.26. Issa B. In vivo measurement of the apparent diffusion coefficient in normal and malignant prostatic tissues using echo-planar imaging. J Magn Reson Imaging. 2002. 16:196–200.27. Zelhof B, Pickles M, Liney G, Gibbs P, Rodrigues G, Kraus S, et al. Correlation of diffusion-weighted magnetic resonance data with cellularity in prostate cancer. BJU Int. 2009. 103:883–888.28. Kozlowski P, Chang SD, Jones EC, Berean KW, Chen H, Goldenberg SL. Combined diffusion-weighted and dynamic contrast-enhanced MRI for prostate cancer diagnosis--correlation with biopsy and histopathology. J Magn Reson Imaging. 2006. 24:108–113.29. Scheidler J, Hricak H, Vigneron DB, Yu KK, Sokolov DL, Huang LR, et al. Prostate cancer: localization with three-dimensional proton MR spectroscopic imaging--clinicopathologic study. Radiology. 1999. 213:473–480.30. Shimofusa R, Fujimoto H, Akamata H, Motoori K, Yamamoto S, Ueda T, et al. Diffusion-weighted imaging of prostate cancer. J Comput Assist Tomogr. 2005. 29:149–153.31. Casciani E, Polettini E, Bertini L, Masselli G, Emiliozzi P, Amini M, et al. Contribution of the MR spectroscopic imaging in the diagnosis of prostate cancer in the peripheral zone. Abdom Imaging. 2007. Epub ahead of print.32. Atlas SW, DuBois P, Singer MB, Lu D. Diffusion measurements in intracranial hematomas: implications for MR imaging of acute stroke. AJNR Am J Neuroradiol. 2000. 21:1190–1194.33. Maldjian JA, Listerud J, Moonis G, Siddiqi F. Computing diffusion rates in T2-dark hematomas and areas of low T2 signal. AJNR Am J Neuroradiol. 2001. 22:112–118.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiparametric MRI of Prostate Cancer after Biopsy: Little Impact of Hemorrhage on Tumor Staging
- Prostate Biopsy: General Consideration and Systematic Biopsy
- Fatal Rectal Bleeding after Prostate Biopsy
- The Use of Magnetic Resonance Imaging in the Prostate Cancer Primary Diagnostic Pathway: Is It Ready for Primetime?
- Medical imaging of prostate cancer