J Korean Med Assoc.
2015 Jan;58(1):7-14. 10.5124/jkma.2015.58.1.7.
Medical imaging of prostate cancer
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. hakjlee@snu.ac.kr
- KMID: 2149277
- DOI: http://doi.org/10.5124/jkma.2015.58.1.7
Abstract
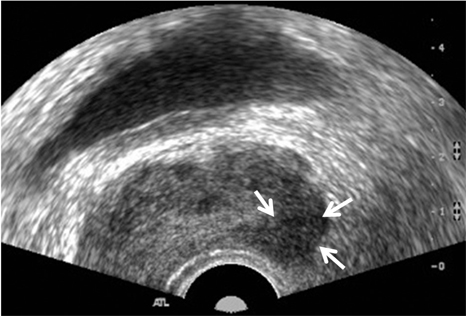
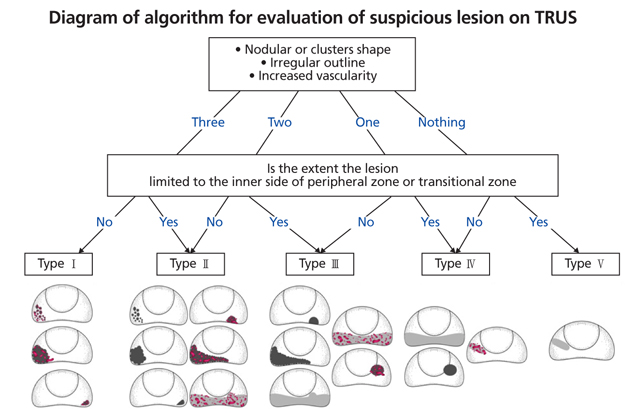
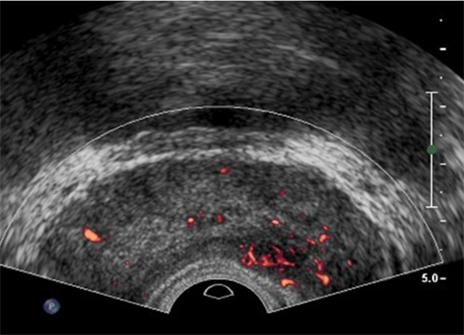
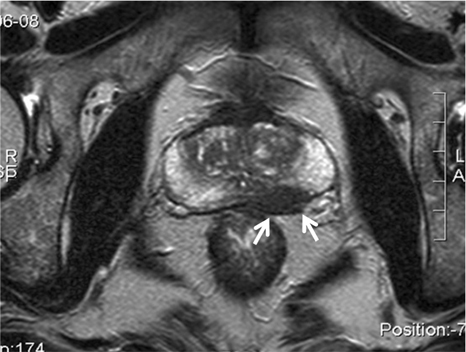
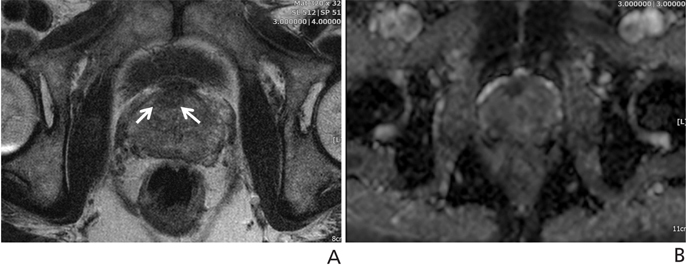
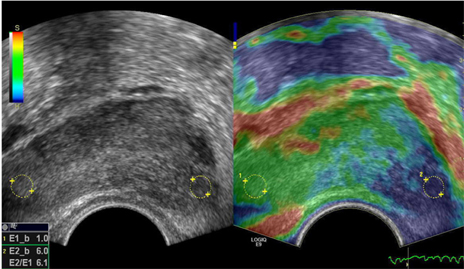
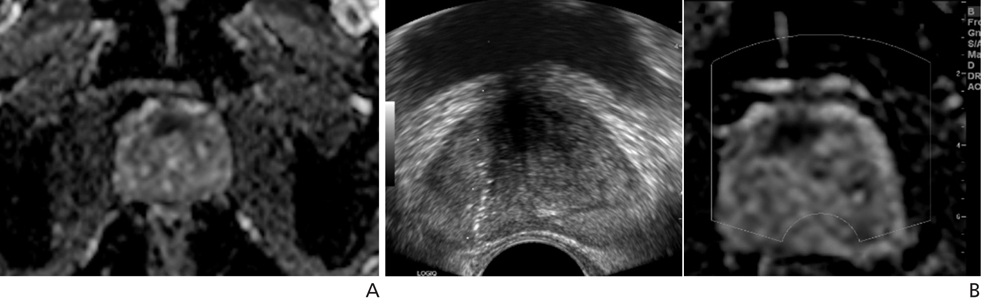
- The clinical significance of prostate cancer is increasing markedly with an increased population of aged persons and Westernized behavior patterns. Accordingly, the role of prostate imaging is also becoming important in the early diagnosis of prostate cancer. Transrectal prostate ultrasound (TRUS) is used for the estimation of prostate volume as well as the detection of prostate cancer, seen as focal hypoechoic lesions. Almost all prostate tissue biopsies are performed under the guidance of TRUS. One of the important issues in prostate imaging is the visualization of suspected prostate cancer lesions. In order to obtain detailed information regarding a suspected prostate lesion, contrast-enhanced imaging is utilized, using microbubbles and elastography. In addition, magnetic resonance imaging-ultra sonography (MRI-US) fusion imaging, in which the ultrasound machine archives magnetic resonance (MR) images and facilitates MRI-US fusion imaging-guided biopsy, has been revealed to be superior to conventional ultrasound-guided biopsy. Prostate MR is usually performed in patients with confirmed prostate cancer, after prostate biopsy for the evaluation of tumor staging or follow-up changes after chemotherapy, hormone therapy, or radiation therapy. In particular, the evaluation of seminal vesicles is crucial for accurate identification of tumor staging. Advanced functional MR techniques, including diffusion-weighted imaging, dynamic contrast-enhanced imaging, and MR spectroscopy, also have potential in the localization of prostate cancer. In summary, the role of prostate imaging in the diagnosis and localization of prostate cancer is increasing. Advanced technologies in ultrasound and MR imaging may have important roles in localization of prostate cancer and image-guided biopsy.
MeSH Terms
Figure
Reference
-
1. Benson MC, Whang IS, Pantuck A, Ring K, Kaplan SA, Olsson CA, Cooner WH. Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer. J Urol. 1992; 147:815–816.
Article2. McNeal JE. Regional morphology and pathology of the prostate. Am J Clin Pathol. 1968; 49:347–357.
Article3. Choi BI. Ultrasound diagnosis of the abdomen. In : Moon MH, Kim SH, editors. Prostate. Seoul: Ilchokak;2006. p. 346–360.4. Lee HY, Lee HJ, Byun SS, Lee SE, Hong SK, Kim SH. Classification of focal prostatic lesions on transrectal ultrasound (TRUS) and the accuracy of TRUS to diagnose prostate cancer. Korean J Radiol. 2009; 10:244–251.
Article5. Littrup PJ, Bailey SE. Prostate cancer: the role of transrectal ultrasound and its impact on cancer detection and management. Radiol Clin North Am. 2000; 38:87–113.
Article6. Lee SE, Byun SS, Lee HJ, Song SH, Chang IH, Kim YJ, Gill MC, Hong SK. Impact of variations in prostatic apex shape on early recovery of urinary continence after radical retropubic prostatectomy. Urology. 2006; 68:137–141.
Article7. Lee SE, Byun SS, Hong SK, Lee HJ, Kim YJ, Chang IH, Gill MC. Anatomical analysis of prostate and surrounding struc-tures: points to consider during radical retropubic prostatectomy. Korean J Urol. 2006; 47:568–577.
Article8. Lee HJ, Chung JH. The application of contrast enhanced ultrasound in molecular imaging. J Korean Soc Ultrasound Med. 2009; 28:139–145.9. Seitz M, Gratzke C, Schlenker B, Buchner A, Karl A, Roosen A, Singer BB, Bastian PJ, Ergün S, Stief CG, Reich O, Tilki D. Contrast-enhanced transrectal ultrasound (CE-TRUS) with cadence-contrast pulse sequence (CPS) technology for the identification of prostate cancer. Urol Oncol. 2011; 29:295–301.
Article10. Jiang J, Chen Y, Zhu Y, Yao X, Qi J. Contrast-enhanced ultrasonography for the detection and characterization of prostate cancer: correlation with microvessel density and Gleason score. Clin Radiol. 2011; 66:732–737.
Article11. Weidner N, Carroll PR, Flax J, Blumenfeld W, Folkman J. Tumor angiogenesis correlates with metastasis in invasive prostate carcinoma. Am J Pathol. 1993; 143:401–409.12. Li Y, Tang J, Fei X, Gao Y. Diagnostic performance of contrast enhanced ultrasound in patients with prostate cancer: a meta-analysis. Acad Radiol. 2013; 20:156–164.
Article13. Mitterberger M, Pinggera GM, Horninger W, Bartsch G, Strasser H, Schafer G, Brunner A, Halpern EJ, Gradl J, Pallwein L, Frauscher F. Comparison of contrast enhanced color Doppler targeted biopsy to conventional systematic biopsy: impact on Gleason score. J Urol. 2007; 178:464–468.
Article14. Pallwein L, Mitterberger M, Struve P, Horninger W, Aigner F, Bartsch G, Gradl J, Schurich M, Pedross F, Frauscher F. Comparison of sonoelastography guided biopsy with systematic biopsy: impact on prostate cancer detection. Eur Radiol. 2007; 17:2278–2285.
Article15. Brock M, von Bodman C, Palisaar RJ, Loppenberg B, Sommerer F, Deix T, Noldus J, Eggert T. The impact of real-time elastography guiding a systematic prostate biopsy to improve cancer detection rate: a prospective study of 353 patients. J Urol. 2012; 187:2039–2043.
Article16. Barr RG, Memo R, Schaub CR. Shear wave ultrasound elastography of the prostate: initial results. Ultrasound Q. 2012; 28:13–20.17. Fiard G, Hohn N, Descotes JL, Rambeaud JJ, Troccaz J, Long JA. Targeted MRI-guided prostate biopsies for the detection of prostate cancer: initial clinical experience with real-time 3-dimensional transrectal ultrasound guidance and magnetic resonance/transrectal ultrasound image fusion. Urology. 2013; 81:1372–1378.
Article18. Sonn GA, Natarajan S, Margolis DJ, MacAiran M, Lieu P, Huang J, Dorey FJ, Marks LS. Targeted biopsy in the detection of prostate cancer using an office based magnetic resonance ultrasound fusion device. J Urol. 2013; 189:86–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiparametric MRI in the Detection of Clinically Significant Prostate Cancer
- Added values of transrectal ultrasonography to magnetic resonance imaging in characterizing prostate cancer: A narrative review
- Prostate Biopsy: General Consideration and Systematic Biopsy
- RE: Diffusion-Weighted Imaging of Prostate Cancer: How Can We Use It Accurately?
- The Use of Magnetic Resonance Imaging in the Prostate Cancer Primary Diagnostic Pathway: Is It Ready for Primetime?