Investig Magn Reson Imaging.
2017 Sep;21(3):139-147. 10.13104/imri.2017.21.3.139.
Multiparametric MRI of Prostate Cancer after Biopsy: Little Impact of Hemorrhage on Tumor Staging
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. sejung@catholic.ac.kr
- 2Catholic Cancer Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Urology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Hospital Pathology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2392684
- DOI: http://doi.org/10.13104/imri.2017.21.3.139
Abstract
- PURPOSE
To evaluate differences in staging accuracy of prostate cancer according to the extent of hemorrhage on multiparametric MRI performed after biopsy.
MATERIALS AND METHODS
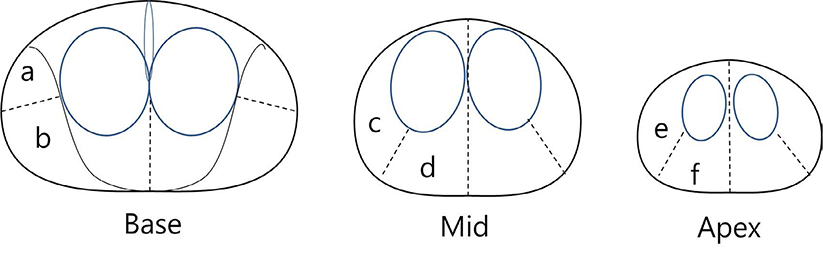
We enrolled 71 consecutive patients with biopsy-proven prostate cancer. Patients underwent MRI followed by a prostatectomy at our institution in 2014. Two radiologists reviewed the MRI to determine the tumor stage. Correlation between biopsy-MRI interval and extent of hemorrhage was evaluated. Regression analyses were used to determine factors associated with accuracy of tumor staging.
RESULTS
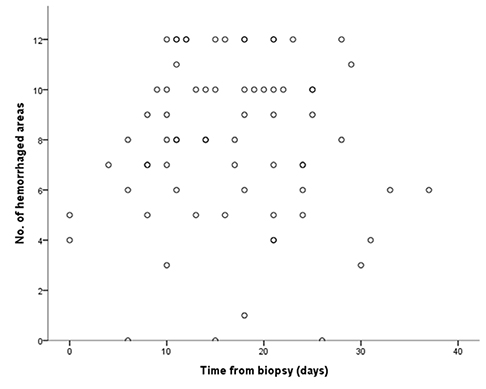
The mean interval between biopsy and MRI was 17.4 ± 10.2 days (range, 0-73 days). The interval between prostate biopsy and MRI and the extent of hemorrhage were not significantly correlated (P = 0.880). There was no significant difference in the accuracy rate of staging between the small and large hemorrhage groups.
CONCLUSION
Biopsy-induced hemorrhage in the prostate gland is not sufficiently absorbed over time. The extent of hemorrhage and the short interval between biopsy and MRI may not impair tumor detection or staging on multiparametric MRI.
MeSH Terms
Figure
Reference
-
1. Bittencourt LK, de Hollanda ES, de Oliveira RV. Multiparametric MR imaging for detection and locoregional staging of prostate cancer. Top Magn Reson Imaging. 2016; 25:109–117.2. Chamie K, Sonn GA, Finley DS, et al. The role of magnetic resonance imaging in delineating clinically significant prostate cancer. Urology. 2014; 83:369–375.3. Delongchamps NB, Rouanne M, Flam T, e t. Multiparametric magnetic resonance imaging for the detection and localization of prostate cancer: combination of T2-weighted, dynamic contrast-enhanced and diffusion-weighted imaging. BJU Int. 2011; 107:1411–1418.4. Dickinson L, Ahmed HU, Allen C, et al. Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: recommendations from a European consensus meeting. Eur Urol. 2011; 59:477–494.5. Hoeks CM, Barentsz JO, Hambrock T, et al. Prostate cancer: multiparametric MR imaging for detection, localization, and staging. Radiology. 2011; 261:46–66.6. Turkbey B, Brown AM, Sankineni S, Wood BJ, Pinto PA, Choyke PL. Multiparametric prostate magnetic resonance imaging in the evaluation of prostate cancer. CA Cancer J Clin. 2016; 66:326–336.7. Turkbey B, Pinto PA, Mani H, et al. Prostate cancer: value of multiparametric MR imaging at 3 T for detection--histopathologic correlation. Radiology. 2010; 255:89–99.8. Ueno Y, Tamada T, Bist V, et al. Multiparametric magnetic resonance imaging: Current role in prostate cancer management. Int J Urol. 2016; 23:550–557.9. Kim TH, Jeong JY, Lee SW, et al. Diffusion-weighted magnetic resonance imaging for prediction of insignificant prostate cancer in potential candidates for active surveillance. Eur Radiol. 2015; 25:1786–1792.10. Abd-Alazeez M, Ahmed HU, Arya M, et al. The accuracy of multiparametric MRI in men with negative biopsy and elevated PSA level--can it rule out clinically significant prostate cancer? Urol Oncol. 2014; 32:45.e17–45.e22.11. Futterer JJ, Briganti A, De Visschere P, et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol. 2015; 68:1045–1105.12. Park BK, Park JW, Park SY, et al. Prospective evaluation of 3-T MRI performed before initial transrectal ultrasound-guided prostate biopsy in patients with high prostate-specific antigen and no previous biopsy. AJR Am J Roentgenol. 2011; 197:W876–W881.13. Porpiglia F, Manfredi M, Mele F, et al. Diagnostic pathway with multiparametric magnetic resonance imaging versus standard pathway: results from a randomized prospective study in biopsy-naive patients with suspected prostate cancer. Eur Urol. 2017; 72:282–288.14. White S, Hricak H, Forstner R, et al. Prostate cancer: effect of postbiopsy hemorrhage on interpretation of MR images. Radiology. 1995; 195:385–390.15. Qayyum A, Coakley FV, Lu Y, et al. Organ-confined prostate cancer: effect of prior transrectal biopsy on endorectal MRI and MR spectroscopic imaging. AJR Am J Roentgenol. 2004; 183:1079–1083.16. Ko YH, Song PH, Moon KH, Jung HC, Cheon J, Sung DJ. The optimal timing of post-prostate biopsy magnetic resonance imaging to guide nerve-sparing surgery. Asian J Androl. 2014; 16:280–284.17. Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging - Reporting and Data System: 2015, Version 2. Eur Urol. 2016; 69:16–40.18. Tamada T, Sone T, Jo Y, et al. Prostate cancer: relationships between postbiopsy hemorrhage and tumor detectability at MR diagnosis. Radiology. 2008; 248:531–539.19. Barrett T, Vargas HA, Akin O, Goldman DA, Hricak H. Value of the hemorrhage exclusion sign on T1-weighted prostate MR images for the detection of prostate cancer. Radiology. 2012; 263:751–757.20. Iremashvili V, Pelaez L, Jorda M, et al. Prostate sampling by 12-core biopsy: comparison of the biopsy results with tumor location in prostatectomy specimens. Urology. 2012; 79:37–42.21. Noguchi M, Stamey TA, McNeal JE, Yemoto CM. Relationship between systematic biopsies and histological features of 222 radical prostatectomy specimens: lack of prediction of tumor significance for men with nonpalpable prostate cancer. J Urol. 2001; 166:104–109. discussion 109-110.22. Kim JW, Park HK, Kim HG, et al. Discordance between location of positive cores in biopsy and location of positive surgical margin following radical prostatectomy. Korean J Urol. 2015; 56:710–716.23. Baco E, Rud E, Vlatkovic L, et al. Predictive value of magnetic resonance imaging determined tumor contact length for extracapsular extension of prostate cancer. J Urol. 2015; 193:466–472.24. Barentsz JO, Richenberg J, Clements R, et al. ESUR prostate MR guidelines 2012. Eur Radiol. 2012; 22:746–757.25. Ikonen S, Kivisaari L, Vehmas T, et al. Optimal timing of post-biopsy MR imaging of the prostate. Acta Radiol. 2001; 42:70–73.26. Sharif-Afshar AR, Feng T, Koopman S, et al. Impact of post prostate biopsy hemorrhage on multiparametric magnetic resonance imaging. Can J Urol. 2015; 22:7698–7702.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiparametric MRI in the Detection of Clinically Significant Prostate Cancer
- Magnetic Resonance Imaging-Guided Prostate Biopsy: Present and Future
- Multiparametric MRI in Active Surveillance of Prostate Cancer: An Overview and a Practical Approach
- MRI-Targeted Prostate Biopsy: What Radiologists Should Know
- Comparison of Multiparametric and Biparametric MRI in First Round Cognitive Targeted Prostate Biopsy in Patients with PSA Levels under 10 ng/mL