Korean J Urol.
2007 May;48(5):489-493. 10.4111/kju.2007.48.5.489.
The Significance of Biopsy of the Erythematous Lesion at Cystoscopy
- Affiliations
-
- 1Department of Urology, Chonnam National University Medical School, Gwangju, Korea. sydad@hanmail.net
- 2Department of Pathology, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2061252
- DOI: http://doi.org/10.4111/kju.2007.48.5.489
Abstract
-
PURPOSE: At cystoscopy, bladder cancer shows various presentations; these are papillary, flat, elevated and ulcerated. Erythematous lesions could be carcinoma in situ (CIS), cancer or benign lesion, so biopsy should be done to exclude malignancy. However, this might cause many problems such as bleeding, inflammation and the added cost. The objectives of this study were to evaluate the significance of erythematous lesion biopsy at cystoscopy and to identify the factors related to the detection of bladder cancer.
MATERIALS AND METHODS
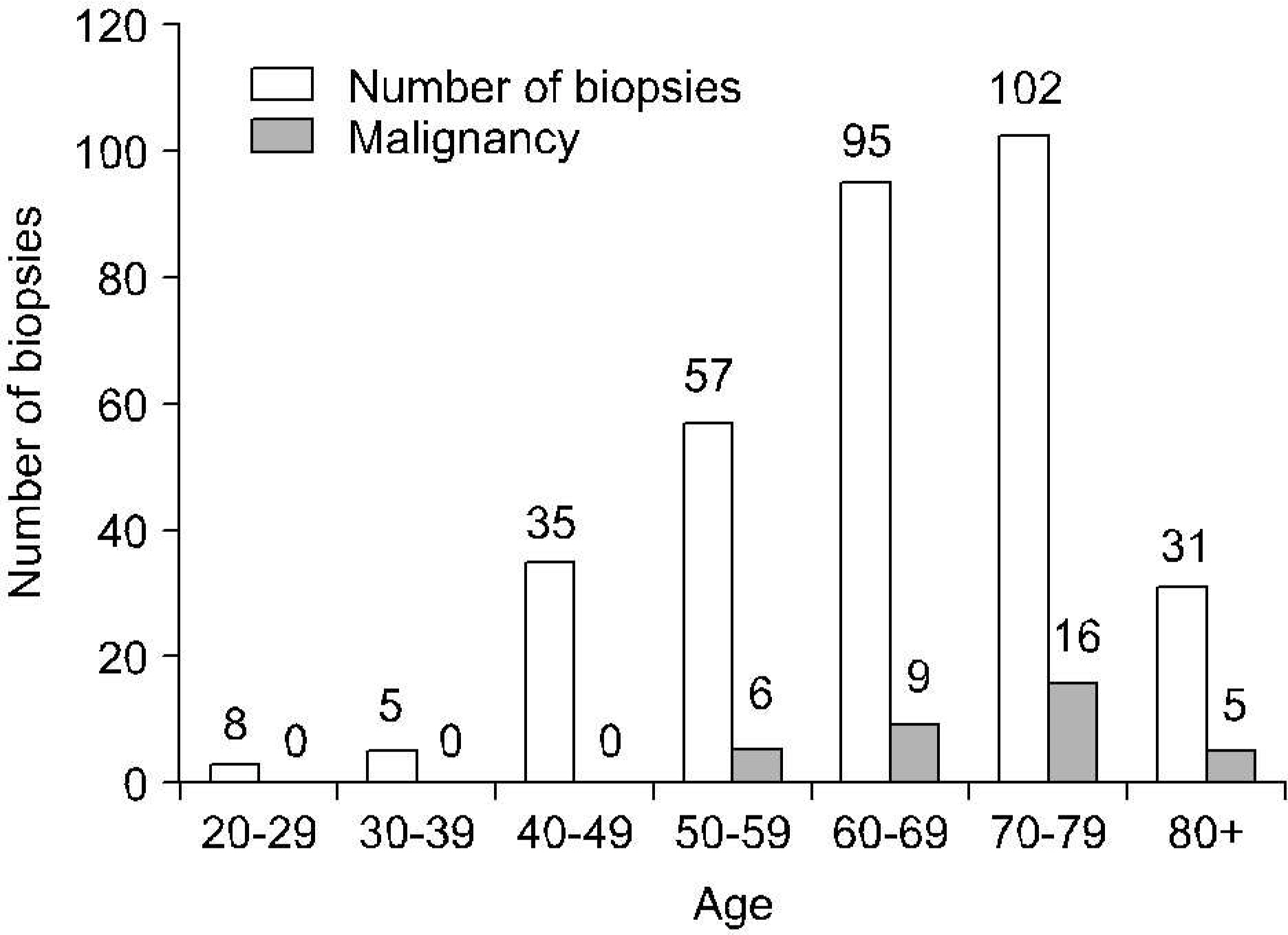
From January 1999 to June 2006, 337 biopsies were taken from the erythematous lesions seen at cystoscopy. We reviewed the pathologic results of the erythematous lesions. We also investigated the patients' histories of bladder cancer, the urine cytology performed at cystoscopy, the intravesical therapy for bladder cancer and the complications after biopsy. A logistic regression analysis was performed to determine the factors associated with the diagnosis of bladder cancer.
RESULTS
In 337 erythematous lesion biopsies, malignancy was found in 36 (10.9%), and 19 of 36 (52.8%) were CIS. Among the benign lesions, chronic cystitis was most common. Bladder cancer was detected more often in patient with a history of transitional cell carcinoma (TCC) and in patients over the age of 65 years. Especially, a history of TCC was an independent risk factor for bladder cancer [odds ratio: 2.974, 95% confidence interval (CI): 1.163-7.604]. After biopsy, hematuria that was needed management occurred in 3.6% of the lesions.
CONCLUSIONS
Erythematous lesion biopsy yields a positive finding of malignancy in 10.9% of the lesions and could be a valuable exam, particularly for the follow-up for TCC, and for patients over the age of 65 years.
Keyword
MeSH Terms
Figure
Reference
-
1.Amling CL. Diagnosis and management of superficial bladder cancer. Curt Probl Cancer. 2001. 25:219–78.
Article2.Messing MM. Urothelial tumors of the bladder. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. editors.Campbell-Walsh urology. 9th ed.Philadelphia: W.B. Saunders;2006. p. 2407–46.3.Satoh E., Miyao N., Tachiki H., Fujisawa Y. Prediction of muscle invasion of bladder cancer by cystoscopy. Eur Urol. 2002. 41:178–81.
Article4.Grignon DJ. Neoplasms of the urinary bladder. Bostwick DG, Eble JN, editors. editors.Urologic surgical pathology. 1st ed.St. Louis: Mosby;1997. p. 215–305.5.Kwon SD., Lee JG., Cho JH. The significance of random mucosal biopsy in bladder cancer. Korean J Urol. 1991. 32:883–5.6.Walker L., Liston TG., Loyd-Davies RW. Does flexible cystoscopy miss more tumours than rod-lens examination? Br J Urol. 1993. 72:449–50.
Article7.Hedelin H., Holmang S., Wiman L. The cost of bladder tumour treatment and follow-up. Scand J Urol Nephrol. 2002. 36:344–7.
Article8.Svatek RS., Lee D., Lotan Y. Correlation of office-based cystoscopy and cytology with histologic diagnosis: how good is the reference standard? Urology. 2005. 66:65–8.
Article9.Cina SJ., Epstein JI., Endrizzi JM., Harmon WJ., Seay TM., Schoenberg MP. Correlation of cystoscopic impression widi histologic diagnosis of biopsy specimens of die bladder. Hum Pathol. 2001. 32:630–7.10.Swinn MJ., Walker MM., Harbin LJ., Adshead JM., Witherow RO., Vale JA, et al. Biopsy of the red patch at cystoscopy: Is it worthwhile? Eur Urol. 2004. 45:471–4.
Article11.Dalbagni G., Rechtschaffen T., Herr HW. Is transurethral biopsy of the bladder necessary after 3 months to evaluate response to bacillus Calmette-Guerin therapy? J Urol. 1999. 162:708–9.
Article12.Skemp NM., Fernandes ET. Routine bladder biopsy after bacille Calmette-Guerin treatment: Is it necessary? Urology. 2002. 59:224–6.13.Kim BH., Park CH., Kim CI. The significance of repeat bladder biopsy after intravesical Bacillus Calmette-Guerin therapy for high risk superficial transitional cell carcinoma of bladder. Korean J Urol. 2005. 46:37–42.14.Kim WJ., Chung JI., Hong JH., Kim CS., Jung SI., Yoon DK. Epidemiological study for urologic cancer in Korea (1998-2002). Korean J Urol. 2004. 45:1081–8.15.Wiener HG., Mian C., Haitel A., Pycha A., Schatzl G., Marberger M. Can urine bound diagnostic tests replace cystoscopy in the management of bladder cancer? J Urol. 1998. 159:1876–80.
Article16.Konety BR., Metro MJ., Melham MF., Salup RR. Diagnostic value of voided urine and bladder barbotage cytology in detecting transitional cell carcinoma of the urinary tract. Urol Int. 1999. 62:26–30.
Article17.Mungan NA., Kulacoglu S., Basar M., Sahin M., Witjes JA. Can sensitivity of voided urinary cytology or bladder wash cytology be improved by the use of different urinary portions? Urol Int. 1999. 62:209–12.
Article18.Pode D., Zylber-Katz E., Shapiro A. Intravesical lidocaine: topical anesthesia for bladder mucosal biopsies. J Urol. 1992. 148:795–6.
Article19.Beaghler M., Grasso M 3rd. Flexible cystoscopic bladder biopsies: a technique for outpatient evaluation of the lower urinary tract urothelium. Urology. 1994. 44:756–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The significance of cystoscopy in staging cervical cancer
- The Significance of Repeat Bladder Biopsy after Intravesical Bacillus Calmette-Guerin Therapy for High Risk Superficial Transitional Cell Carcinoma of Bladder
- Value of Cystoscopy in Cervix Cancer Staging - Analysis of 1,049 Cases -
- Urothelial Carcinoma Arising from a Large Ureteral Polyp
- Three Cases of Cystitis Confused with Bladder Tumor on the Cystogram