Korean Circ J.
2009 Mar;39(3):116-120. 10.4070/kcj.2009.39.3.116.
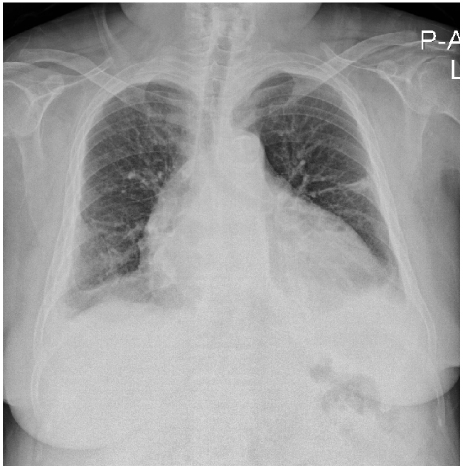
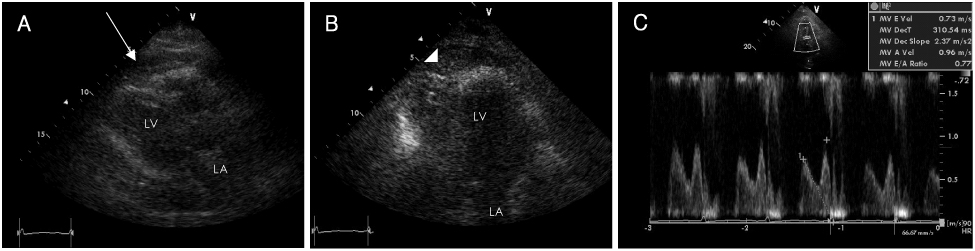
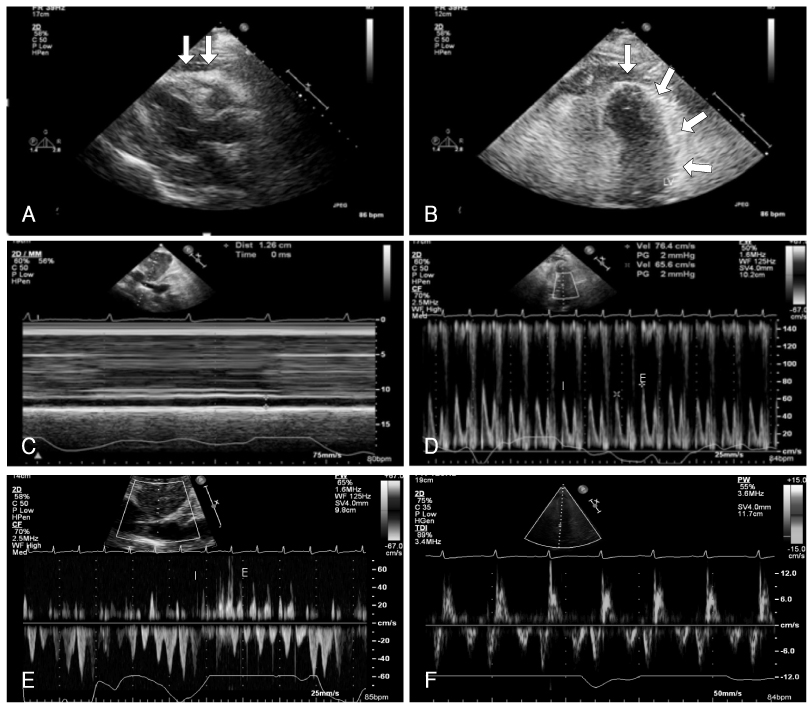
A Case of Constrictive Pericarditis Associated With Huge Epicardial Fat Volume
- Affiliations
-
- 1Department of Internal Medicine, Ulsan University Hospital, College of Medicine, University of Ulsan, Ulsan, Korea. kimsc226@lycos.co.kr
- 2Department of Radiology, Ulsan University Hospital, College of Medicine, University of Ulsan, Ulsan, Korea.
- KMID: 1825969
- DOI: http://doi.org/10.4070/kcj.2009.39.3.116
Abstract
- Massive deposits of fat around heart are seen in overweight persons and are associated with coronary artery disease. Investigators have focused on the clinical significance of epicardial fat with respect to metabolic effects such as insulin resistance and inflammation, but the mechanical effects, such as constriction, have been largely ignored. We present an unusual case of a 59-year-old woman with obesity and diabetes mellitus who had been undergoing peritoneal dialysis due to end-stage renal disease, and who developed constrictive pericarditis, possibly secondary to extensive epicardial fatty accumulation.
Keyword
MeSH Terms
Figure
Reference
-
1. Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J. 2007. 153:907–917.2. Iacobellis G, Ribaudo MC, Assael F, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003. 88:5163–5168.3. Ahn SG, Lim HS, Joe DY, et al. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease. Heart. 2008. 94:e7.4. Yang HS, Song JK, Song JM, et al. Clinical characteristics of constrictive pericarditis diagnosed by echo-Doppler technique in Korea. J Korean Med Sci. 2001. 16:558–566.5. Park SY. The usefulness of pericardial biopsy to evaluate the causes of pericardial disease. Korean Circ J. 1999. 29:517–522.6. Katagiri H, Yamada T, Oka Y. Adiposity and cardiovascular disorders: disturbance of the regulatory system consisting of humoral and neuronal signals. Circ Res. 2007. 101:27–39.7. Mazurek T, Zhang L, Zalewski A, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003. 108:2460–2466.8. Iacobellis G, Leonetti F, Singh N, M Sharma A. Relationship of epicardial adipose tissue with atrial dimensions and diastolic function in morbidly obese subjects. Int J Cardiol. 2007. 115:272–273.9. LeWinter MM. Libby P, Bonow PL, Mann DL, Zipes DP, editors. Pericardial disease. Braunwald's Heart Disease: A Text Book of Cardiovascular Medicine. 2008. 8th ed. Philadelphia: Saunders Elsevier;1833.10. Sarin S, Wenger C, Marwaha A, et al. Clinical significance of epicardial fat measured using cardiac multislice computed tomography. Am J Cardiol. 2008. 102:767–771.11. Salanitri JC, Pereles FS. Cardiac lipoma and lipomatous hypertrophy of the interatrial septum: cardiac magnetic resonance imaging findings. J Comput Assist Tomogr. 2004. 28:852–856.12. Ha JW, Ommen SR, Tajik AJ, et al. Differentiation of constrictive pericarditis from restrictive cardiomyopathy using mitral annular velocity by tissue Doppler echocardiography. Am J Cardiol. 2004. 94:316–319.13. Sengupta PP, Krishnamoorthy VK, Abhayaratna WP, et al. Comparison of usefulness of tissue Doppler imaging versus brain natriuretic peptide for differentiation of constrictive pericardial disease from restrictive cardiomyopathy. Am J Cardiol. 2008. 102:357–362.14. Oyama N, Oyama N, Komuro K, Nambu T, Manning WJ, Miyasaka K. Computed tomography and magnetic resonance imaging of the pericardium: anatomy and pathology. Magn Reson Med Sci. 2004. 3:145–152.15. Talreja DR, Nishimura RA, Oh JK, Holmes DR. Constrictive pericarditis in the modern era: novel criteria for diagnosis in the cardiac catheterization laboratory. J Am Coll Cardiol. 2008. 51:315–319.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Constrictive Pericarditis Following Acute Idiopathic Pericarditis
- Tuberculous Constrictive Pericarditis: A Classical Case and Review
- A Case of Constrictive Pericarditis with Localized Pericardial Effusion Simulating a Cystic Mass
- Echocardiographic Evaluation of Constrictive Pericarditis
- Constrictive Pericarditis as a Never Ending Story: What's New?