Korean Circ J.
2012 Mar;42(3):143-150. 10.4070/kcj.2012.42.3.143.
Constrictive Pericarditis as a Never Ending Story: What's New?
- Affiliations
-
- 1Cardiovascular Center, Seoul National University Hospital, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. dwsohn@snu.ac.kr
- KMID: 2225027
- DOI: http://doi.org/10.4070/kcj.2012.42.3.143
Abstract
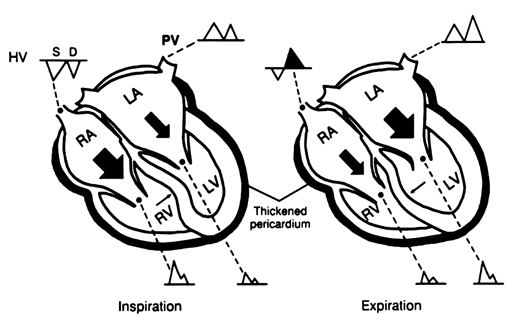
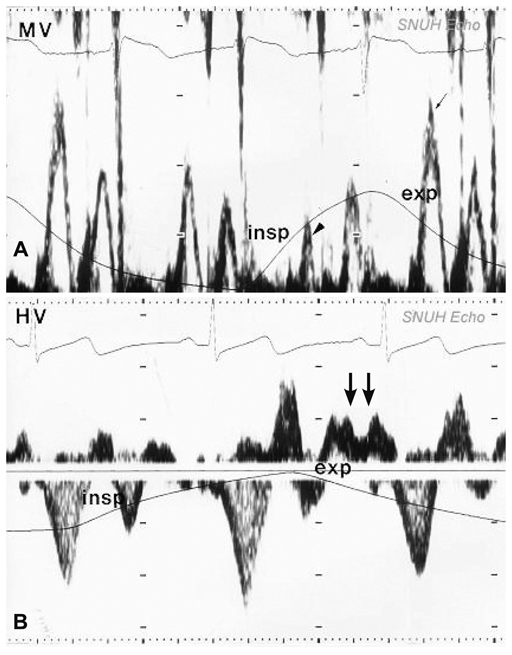
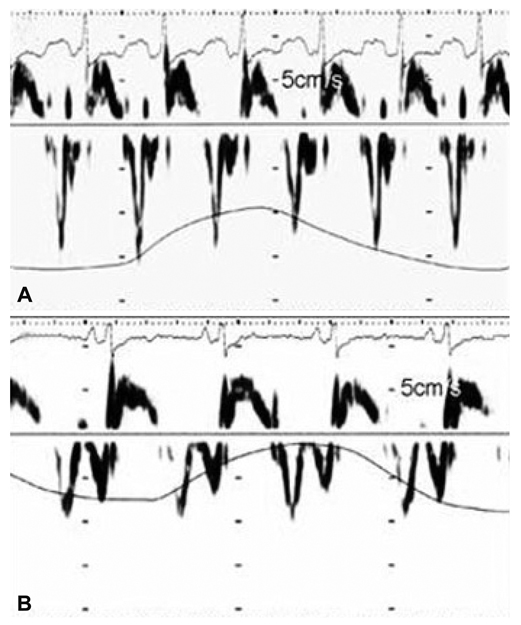
- Nowadays, we have a better understanding of the natural history of constrictive pericarditis such as transient constriction. In addition, we have acquired the correct understanding of hemodynamic features that are unique to constrictive pericarditis. This understanding has allowed us to diagnose constrictive pericarditis reliably with Doppler echocardiography and differentiation between constrictive pericarditis and restrictive cardiomyopathy is no longer a clinical challenge. The advent of imaging modalities such as CT or MR is another advance in the diagnosis of constrictive pericarditis. We can accurately measure pericardial thickness and additional information such as the status of coronary artery and the presence of myocardial fibrosis can be obtained. We no longer perform cardiac catheterization for the diagnosis of constrictive pericarditis. However, these advances are useless unless we suspect and undergo work-up for constrictive pericarditis. In constrictive pericarditis, the most important diagnostic tool is clinical suspicion. In a patient with signs and symptoms of increased systemic venous pressure i.e. right sided heart failure, that are disproportionate to pulmonary or left sided heart disease, possibility of constrictive pericarditis should always be included in the differential diagnosis.
MeSH Terms
Figure
Reference
-
1. Fowler NO. Constrictive pericarditis: its history and current status. Clin Cardiol. 1995. 18:341–350.2. Imazio M, Brucato A, Maestroni S, et al. Risk of constrictive pericarditis after acute pericarditis. Circulation. 2011. 124:1270–1275.3. Imazio M, Brucato A, Adler Y, et al. Prognosis of idiopathic recurrent pericarditis as determined from previously published reports. Am J Cardiol. 2007. 100:1026–1028.4. Robertson R, Arnold CR. Constrictive pericarditis with particular reference to etiology. Circulation. 1962. 26:525–529.5. Bertog SC, Thambidorai SK, Parakh K, et al. Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy. J Am Coll Cardiol. 2004. 43:1445–1452.6. Ling LH, Oh JK, Schaff HV, et al. Constrictive pericarditis in the modernera: evolving clinical spectrum and impact on outcome after pericardiectomy. Circulation. 1999. 100:1380–1386.7. Masui T, Finck S, Higgins CB. Constrictive pericarditis and restrictive cardiomyopathy: evaluation with MR imaging. Radiology. 1992. 182:369–373.8. Breen JF. Imaging of the pericardium. J Thorac Imaging. 2001. 16:47–54.9. Maisch B, Seferović PM, Ristić AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the Task Force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004. 25:587–610.10. Kojima S, Yamada N, Goto Y. Diagnosis of constrictive pericarditis by tagged cine magnetic resonance imaging. N Engl J Med. 1999. 341:373–374.11. Verhaert D, Gabriel RS, Johnston D, Lytle BW, Desai MY, Klein AL. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010. 3:333–343.12. Connolly DC, Wood EH. Cardiac catheterization in heart failure and cardiac constriction. Trans Am Coll Cardiol. 1957. 7:191–201.13. Meaney E, Shabetai R, Bhargava V, et al. Cardiac amyloidosis, contrictive pericarditis and restrictive cardiomyopathy. Am J Cardiol. 1976. 38:547–556.14. Hatle LK, Appleton CP, Popp RL. Differentiation of constrictive pericarditis and restrictive cardiomyopathy by Doppler echocardiography. Circulation. 1989. 79:357–370.15. Oh JK, Hatle LK, Seward JB, et al. Diagnostic role of Doppler echocardiography in constrictive pericarditis. J Am Coll Cardiol. 1994. 23:154–162.16. Sun JP, Abdalla IA, Yang XS, et al. Respiratory variation of mitral and pulmonary venous Doppler flow velocities in constrictive pericarditis before and after pericardiectomy. J Am Soc Echocardiogr. 2001. 14:1119–1126.17. Ha JW, Oh JK, Ommen SR, Ling LH, Tajik AJ. Diagnostic value of mitral annular velocity for constrictive pericarditis in the absence of respiratory variation in mitral inflow velocity. J Am Soc Echocardiogr. 2002. 15:1468–1471.18. Sohn DW, Kim YJ, Kim HS, Kim KB, Park YB, Choi YS. Unique features of early diastolic mitral annulus velocity in constrictive pericarditis. J Am Soc Echocardiogr. 2004. 17:222–226.19. Oh JK, Tajik AJ, Appleton CP, Hatle LK, Nishimura RA, Seward JB. Preload reduction to unmask the characteristic Doppler features of constrictive pericarditis: a new observation. Circulation. 1997. 95:796–799.20. Garcia MJ, Rodriguez L, Ares M, Griffin BP, Thomas JD, Klein AL. Differentiation of constrictive pericarditis from restrictive cardiomyopathy: assessment of left ventricular diastolic velocities in longitudinal axis by Doppler tissue imaging. J Am Coll Cardiol. 1996. 27:108–114.21. Reuss CS, Wilansky SM, Lester SJ, et al. Using mitral 'annulus reversus' to diagnose constrictive pericarditis. Eur J Echocardiogr. 2009. 10:372–375.22. Choi JH, Choi JO, Ryu DR, et al. Mitral and tricuspid annular velocities in constrictive pericarditis and restrictive cardiomyopathy: correlation with pericardial thickness on computed tomography. JACC Cardiovasc Imaging. 2011. 4:567–575.23. Ha JW, Oh JK, Ling LH, Nishimura RA, Seward JB, Tajik AJ. Annulus paradoxus: transmitral flow velocity to mitral annular velocity ratio is in versely proportional to pulmonary capillary wedge pressure inpatients with constrictive pericarditis. Circulation. 2001. 104:976–978.24. Ling LH, Oh JK, Tei C, et al. Pericardial thickness measured with transesophageal echocardiography: feasibility and potential clinical usefulness. J Am Coll Cardiol. 1997. 29:1317–1323.25. Pandian NG, Skorton DJ, Kieso RA, Kerber RE. Diagnosis of constrictive pericarditis by two-dimensional echocardiography: studies in a new experimental model and in patients. J Am Coll Cardiol. 1984. 4:1164–1173.26. Candell-Riera J, García del Castillo H, Permanyer-Miralda G, Soler-Soler J. Echocardiographic features of the interventricular septum in chronic constrictive pericarditis. Circulation. 1978. 57:1154–1158.27. Chowdhury UK, Subramaniam GK, Kumar AS, et al. Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques. Ann Thorac Surg. 2006. 81:522–529.28. DeValeria PA, Baumgartner WA, Casale AS, et al. Current indications, risks, and outcome after pericardiectomy. Ann Thorac Surg. 1991. 52:219–224.29. Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK. Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol. 2004. 43:271–275.30. Feng D, Glockner J, Kim K, et al. Cardiac magnetic resonance imaging pericardial late gadolinium enhancement and elevated inflammatory markers can predict the reversibility of constrictive pericarditis after antiinflammatory medical therapy: a pilot study. Circulation. 2011. 124:1830–1837.31. Bush CA, Stang JM, Wooley CF, Kilman JW. Occult constrictive pericardial disease: diagnosis by rapid volume expansion and correction by pericardiectomy. Circulation. 1977. 56:924–930.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Constrictive Pericarditis Following Acute Idiopathic Pericarditis
- Echocardiographic Evaluation of Constrictive Pericarditis
- Tuberculous Constrictive Pericarditis: A Classical Case and Review
- A Case of Constrictive Pericarditis with Localized Pericardial Effusion Simulating a Cystic Mass
- A Case of Effusive-Constrictive Pericarditis in and Infant Treated by Pericardiectomy