J Korean Med Sci.
2013 Jul;28(7):1015-1020. 10.3346/jkms.2013.28.7.1015.
Changes in Body Composition Predict Homocysteine Changes and Hyperhomocysteinemia in Korea
- Affiliations
-
- 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon, Korea.
- 2Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, NC 27710, USA. anastasia.georgiades@duke.edu
- KMID: 1777496
- DOI: http://doi.org/10.3346/jkms.2013.28.7.1015
Abstract
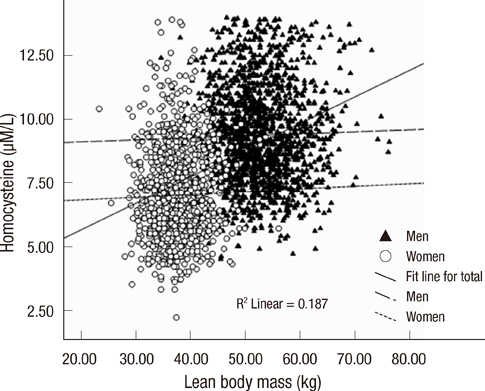
- Cardiovascular disease (CVD) is the primary cause of death in Korea. Hyperhomocysteinemia confers an independent risk for CVD comparable to the risk of smoking and hyperlipidemia. The purpose of this study was to assess the effect of cardiovascular risk factors and body composition change on homocysteine (Hcy) levels in Korean men and women. The association between body composition and Hcy levels was investigated in a 2-yr prospective cohort study of 2,590 Koreans (mean age 45.5+/-9.6 yr). There were 293 cases of hyperhomocysteinemia (>14 microM/L) at follow-up. Increases in total body fat proportion and decreases in lean body mass (LBM) were significantly associated with increases in Hcy concentration after controlling for confounding factors. Further adjustments for behavioral factors showed that decreases in LBM were associated with Hcy increase. Decrease in LBM also predicted hyperhomocysteinemia at follow-up, after controlling for confounding factors. There was no significant association between change in body mass index (BMI) and Hcy concentrations over time. Hcy changes over time were related to change in LBM and body fat content, whereas BMI or weight change did not predict change in Hcy levels. Changes in ratio of LBM to total fat mass may contribute to hyperhomocysteinemia.
MeSH Terms
Figure
Cited by 1 articles
-
Associations of Metabolic Syndrome with Total Testosterone and Homocysteine Levels in Male Korean Workers
Sook Hee Sung, Nam Hee Kim, Sun Pyo Hong, Jong-Keun Lee, Seung Jin Choi
Endocrinol Metab. 2019;34(2):158-168. doi: 10.3803/EnM.2019.34.2.158.
Reference
-
1. Graham IM, Daly LE, Refsum HM, Robinson K, Brattström LE, Ueland PM, Palma-Reis RJ, Boers GH, Sheahan RG, Israelsson B, et al. Plasma homocysteine as a risk factor for vascular disease: the European Concerted Action Project. JAMA. 1997. 277:1775–1781.2. Upchurch GR Jr, Welch GN, Fabian AJ, Pigazzi A, Keaney JF Jr, Loscalzo J. Stimulation of endothelial nitric oxide production by homocyst(e)ine. Atherosclerosis. 1997. 132:177–185.3. Ventura E, Durant R, Jaussent A, Picot MC, Morena M, Badiou S, Dupuy AM, Jeandel C, Cristol JP. Homocysteine and inflammation as main determinants of oxidative stress in the elderly. Free Radic Biol Med. 2009. 46:737–744.4. Vollset SE, Refsum H, Nygård O, Ueland PM. Carmel R, Jacobsen DW, editors. Lifestyle factors associated with hyperhomocysteinemia. Homocysteine in health and disease. 2001. Cambridge: Cambridge University Press;341–355.5. Weiss N. Mechanisms of increased vascular oxidant stress in hyperhomocys-teinemia and its impact on endothelial function. Curr Drug Metab. 2005. 6:27–36.6. Stühlinger MC, Stanger O. Asymmetric dimethyl-L-arginine (ADMA): a possible link between homocyst(e)ine and endothelial dysfunction. Curr Drug Metab. 2005. 6:3–14.7. Nurk E, Tell GS, Vollset SE, Nygård O, Refsum H, Nilsen RM, Ueland PM. Changes in lifestyle and plasma total homocysteine: the Hordaland Homocysteine Study. Am J Clin Nutr. 2004. 79:812–819.8. Henning BF, Tepel M, Riezler R, Gillessen A, Doberauer C. Vitamin supplementation during weight reduction: favourable effect on homocysteine metabolism. Res Exp Med (Berl). 1998. 198:37–42.9. Manore MM. Effect of physical activity on thiamine, riboflavin, and vitamin B-6 requirements. Am J Clin Nutr. 2000. 72:598S–606S.10. Giltay EJ, Hoogeveen EK, Elbers JM, Gooren LJ, Asscheman H, Stehouwer CD. Insulin resistance is associated with elevated plasma total homocysteine levels in healthy, non-obese subjects. Atherosclerosis. 1998. 139:197–198.11. Perrone RD, Madias NE, Levey AS. Serum creatinine as an index of renal function: new insights into old concepts. Clin Chem. 1992. 38:1933–1953.12. Battezzati A, Bertoli S, San Romerio A, Testolin G. Body composition: an important determinant of homocysteine and methionine concentrations in healthy individuals. Nutr Metab Cardiovasc Dis. 2007. 17:525–534.13. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report: National Institutes of Health. Obes Res. 1998. 6:51S–209S.14. Nakhai Pour HR, Grobbee DE, Muller M, Emmelot-Vonk M, van der Schouw YT. Serum sex hormone and plasma homocysteine levels in middle-aged and elderly men. Eur J Endocrinol. 2006. 155:887–893.15. Ingenbleek Y, Hardillier E, Jung L. Subclinical protein malnutrition is a determinant of hyperhomocysteinemia. Nutrition. 2002. 18:40–46.16. Ingenbleek Y, Young VR. The essentiality of sulfur is closely related to nitrogen metabolism: a clue to hyperhomocysteinaemia. Nutr Res Rev. 2004. 17:135–151.17. Krebs HA, Hems R, Tyler B. The regulation of folate and methionine metabolism. Biochem J. 1976. 158:341–353.18. Kutzbach C, Stokstad EL. Mammalian methylenetetrahydrofolate reductase: partial purification, properties, and inhibition by S-adenosylmethionine. Biochim Biophys Acta. 1971. 250:459–477.19. Rauh M, Verwied S, Knerr I, Dörr HG, Sönnichsen A, Koletzko B. Homocysteine concentrations in a German cohort of 500 individuals: reference ranges and determinants of plasma levels in healthy children and their parents. Amino Acids. 2001. 20:409–418.20. De Laet C, Wautrecht JC, Brasseur D, Dramaix M, Boeynaems JM, Decuyper J, Kahn A. Plasma homocysteine concentration in a Belgian school-age population. Am J Clin Nutr. 1999. 69:968–972.21. Clifton PM, Keogh JB, Noakes M. Long-term effects of a high-protein weight-loss diet. Am J Clin Nutr. 2008. 87:23–29.22. Nair KS. Aging muscle. Am J Clin Nutr. 2005. 81:953–963.23. Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, et al. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean Sarcopenic Obesity Study. Int J Obes (Lond). 2009. 33:885–892.24. Björck J, Hellgren M, Råstam L, Lindblad U. Associations between serum insulin and homocysteine in a Swedish population-a potential link between the metabolic syndrome and hyperhomocysteinemia: the Skaraborg project. Metabolism. 2006. 55:1007–1013.25. Schäfer SA, Müssig K, Stefan N, Häring HU, Fritsche A, Balletshofer BM. Plasma homocysteine concentrations in young individuals at increased risk of type 2 diabetes are associated with subtle differences in glomerular filtration rate but not with insulin resistance. Exp Clin Endocrinol Diabetes. 2006. 114:306–309.26. Martos R, Valle M, Morales R, Cañete R, Gavilan MI, Sánchez-Margalet V. Hyperhomocysteinemia correlates with insulin resistance and low-grade systemic inflammation in obese prepubertal children. Metabolism. 2006. 55:72–77.27. Skov AR, Toubro S, Bülow J, Krabbe K, Parving HH, Astrup A. Changes in renal function during weight loss induced by high vs low-protein low-fat diets in overweight subjects. Int J Obes Relat Metab Disord. 1999. 23:1170–1177.28. Pancharuniti N, Lewis CA, Sauberlich HE, Perkins LL, Go RC, Alvarez JO, Macaluso M, Acton RT, Copeland RB, Cousins AL, et al. Plasma homocyst(e)ine, folate, and vitamin B-12 concentrations and risk for early-onset coronary artery disease. Am J Clin Nutr. 1994. 59:940–948.29. Lussier-Cacan S, Xhignesse M, Piolot A, Selhub J, Davignon J, Genest J Jr. Plasma total homocysteine in healthy subjects: sex-specific relation with biological traits. Am J Clin Nutr. 1996. 64:587–593.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Analysis of Methylenetetrahydrofolate Reductase Mutation in Recurrent Spontaneous Abortion Associated with Hyperhomocysteinemia
- A Case of Hyperhomocysteinemia Manifested by Deep Vein Thrombosis and Pulmonary Embolism
- Association between Elevated Plasma Homocysteine and Low Skeletal Muscle Mass in Asymptomatic Adults
- Clinical Significance of Hyperhomocysteinemia Between Alzheimer's Disease and Vascular Dementia
- A Case of Pulmonary Thromboembolism in a Patient with Hyperhomocysteinemia