J Korean Soc Spine Surg.
2008 Mar;15(1):9-17. 10.4184/jkss.2008.15.1.9.
Polyaxial Screws with Thick Rod versus Monoaxial Screws with Thin Rod in Video-Assisted Thoracoscopic Scoliosis Surgery (VATS)
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. mes1007@yuhs.ac
- 2Department of Orhtopaedic Surgery, National Health Insurance Corporation Ilsan Hospital, Korea.
- KMID: 1482838
- DOI: http://doi.org/10.4184/jkss.2008.15.1.9
Abstract
-
STUDY DESIGN: Prospective controlled cohort study
OBJECTIVE
To analyze the clinical outcome of video-assisted thoracoscopic surgery (VATS) between two different types of implants. SUMMARY OF LITERATURE REVIEW: The problem of correction loss has been reported with VATS, and different screws and rods have been developed to overcome this problem. Different implants will have varying effects in correctional outcome after VATS.
MATERIALS AND METHODS
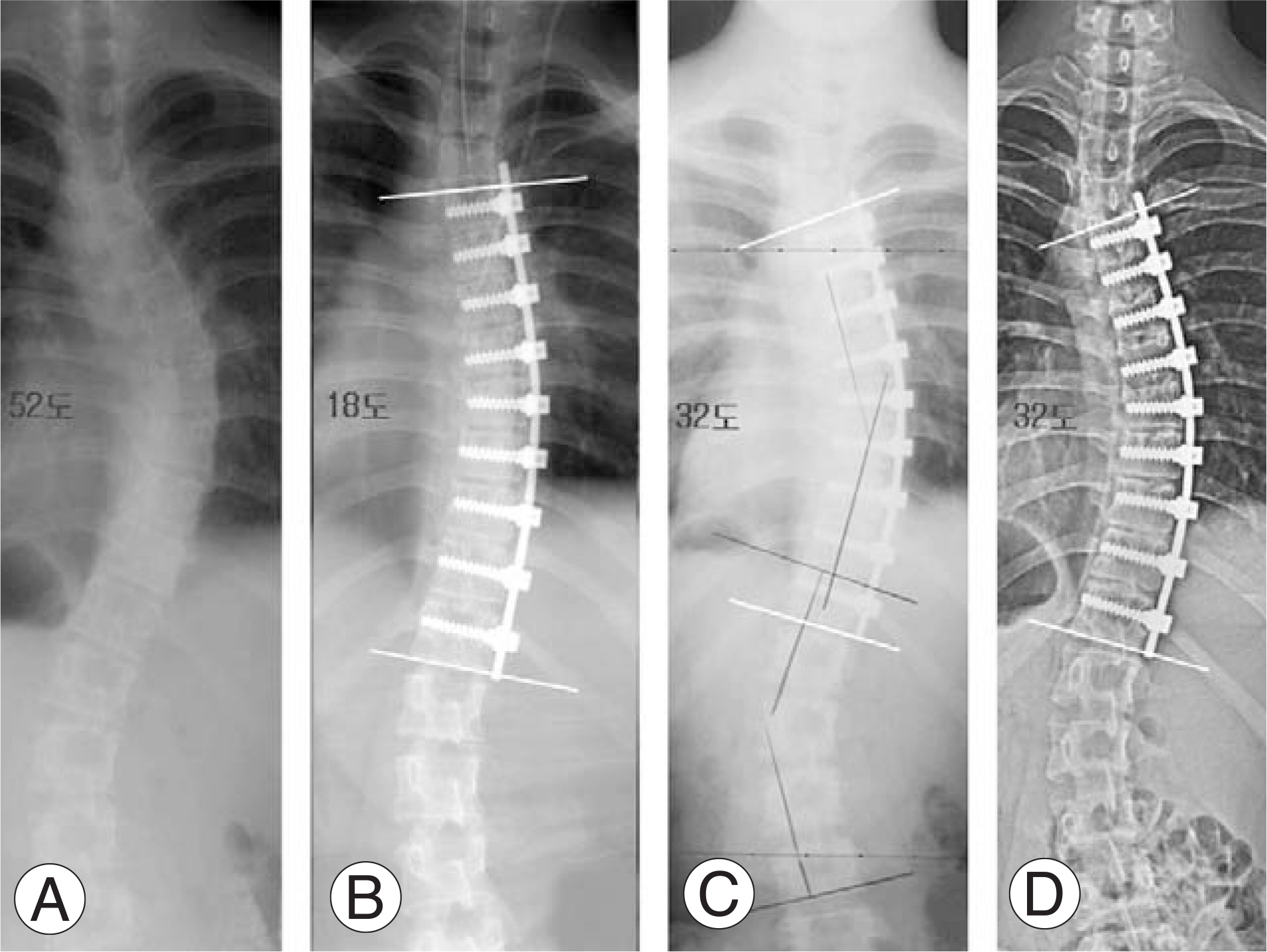
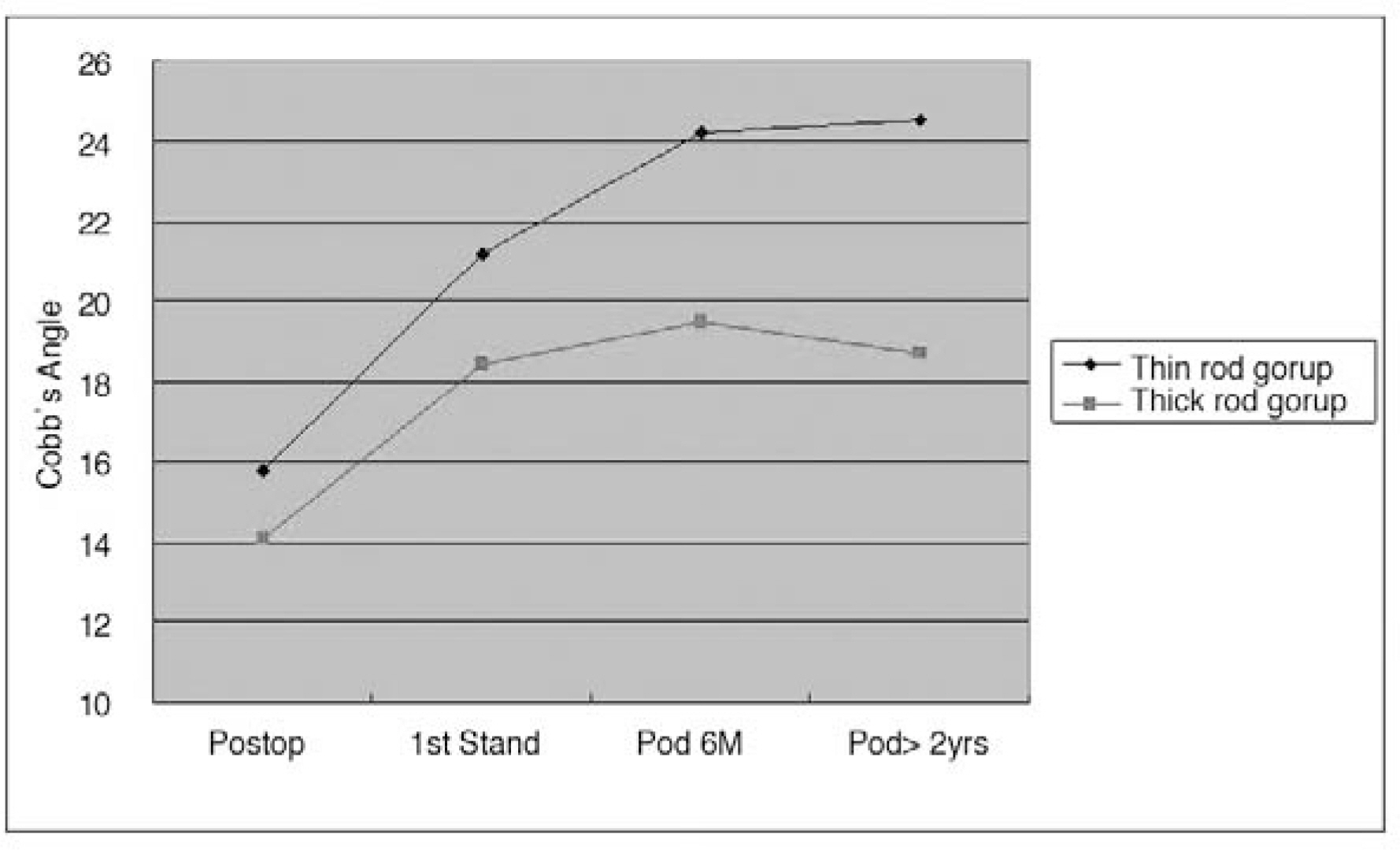
A total of 39 cases of idiopathic adolescent scoliosis treated with VATS between June 2001 and January 2005 were included in the study (mono-axial screws and a 4.5 mm rod: thin rod group=19 cases; poly-axial reduction screws and a 5.5 mm diameter rod: thick rod group=20 cases). All patients were followed for over 2 years postoperatively. For the comparison of surgical outcomes between the two groups, radiographic measurements were performed in the coronal and sagittal planes.
RESULTS
Preoperative scoliosis angle (thin rod group 49.8degrees, thick rod group 47.1degrees), age, BMI, Risser stage, union time, operative time, and blood loss showed no statistical difference between the two groups. Postoperative average correction rate of scoliosis angle was 69% (15.8degrees) in the thin rod group and 70% (14.1degrees) in the thick rod group. However, correction rate after 2 years was 51% (24.5degrees) in the thin rod group and 60% (18.7degrees) in the thick rod group, showing statistically significant difference. There was a tendency toward correction loss in the thin rod group (8.7degrees vs. 4.6degrees p=0.0057).
CONCLUSION
Postoperative correction rate was satisfactory in both groups. However, the thin rod group showed substantial correction loss. Therefore, poly-axial screws and thick rods are more suitable in VATS correction of scoliosis.
Keyword
MeSH Terms
Figure
Reference
-
1). Arlet V. Anterior thoracoscopic spine release in deformity surgery: a metaanalysis and review. Eur Spine J. 2000; 9:17–23.
Article2). Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine. 2003; 28:36–43.
Article3). Lenke LG, Newton PO, Marks MC, et al. Prospective pulmonary function comprarison of open versus endoscopic anterior fusion combined with posterior fusion in adolescent idiopathic scoliosis. Spine. 2004; 29:2055–2060.4). Picetti GD 3rd, Ertl JP, Bueff HU. Endoscopic instrumentation, correction, and fusion of idiopathic scoliosis. Spine J. 2001; 1:190–197.
Article5). Son-Hing JP, Blakemore LC, Poe-Kochert C, Thopson GH. Video-assisted thoracoscopic surgery in idiopathic scoliosis: evaluation of the learining curve. Spine. 2007; 32:703–707.6). Sucato DJ. Thoracoscopic anterior instrumentation and fusion for idiopathic scoliosis. J Am Acad Orhop Surg. 2003; 11:221–227.
Article7). Karami M, Ilharreborde B, Morel E, Fitoussi F, Pen-necot GF, Mazda K. Video-assisted thoracoscopic surgery (VATS) for the treatment of scoliotic rib hump deformity. Eur Spine J. 2007; 16:1373–1377.8). Kim HS, Lee CS, Jeon BH, Park JO. Sagittal plane analysis of adolescent idiopathic scoliosis after VATS (video-assisted thoracoscopic surgery) anterior instrumentations. Yonsei Med J. 2007; 48:90–96.
Article9). Lonner BS, Kondrachov D, Siddiqi F, Hayes V, Scharf C. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. Surgical technique. J Bone Joint Surg Am. 2007; 89:142–156.10). Newton PO, Marks M, Faro F, et al. Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine. 2003; 28:249–254.
Article11). Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of lenke type I adolescent idiopathic scoliosis curves. Spine. 2005; 30:1859–1866.
Article12). Wong HK, Hee HT, Yu Z, Wong D. Results of thoracoscopic instrumented fusion versus conventional posterior instrumented fusion in adolescent idiopathic scoliosis undergoing selective thoracic fusion. Spine. 2004; 29:2031–2038.
Article13). Crawford AH, Wall EJ, Wolf R. Video-assisted thoracoscopy. Orthop Clin North Am. 1999; 30:367–385.
Article14). Ohtsuka T, Ohnishi I, Nakamura K, Takamoto S. New instrumentation for video-assisted anterior spine release. Surg Endosc. 2000; 14:682–684.
Article15). Brodner W, Mun Yue W, Moller HB, Hendricks KJ, Burd TA, Gaines RW. Short segment bone-on-bone instrumentation for single curve idiopathic scoliosis. Spine. 2003; 28:224–233.
Article16). Smith JA, Deviren V, Berven S, Bradford DS. Does instrumented anterior scoliosis surgery lead to kyphosis, pseudoarthrosis, or inadequate correction in adults? Spine. 2002; 27:529–534.17). Betz RR, Harms J, Clements DH, et al. Comparision of anterior and posterior instrumentation for correction of adolescent idiopathic scoliosis. Spine. 1999; 24:225–239.18). Spiegel DA, Flynn JM, Drummond DS. Anterior instrumentation in the treatment of scoliosis. UPOJ. 1998; 11:19–26.19). Sweet FA, Lenke LG, Bridwell KH, Clements DH, Lowe TG, Blanke K. Prospective radiographic and clinical outcomes and complications of single rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine. 2001; 26:1956–1965.20). Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosisL a new classification to determine exent of spinal arthrodesis. J Bone Joint Surg Am. 2001; 83:1169–1181.21). Bital FD, Neuwirth MG, Kuflik PL, Casden A, Bloom N, Siddiqui S. The use of short and rigid anterior instrumentation in the treatment of idiopathic thoracolumbar scoliosis. Spine. 2002; 27:1553–1557.
Article22). Bullmann V, Halm HF, Niemeyer T, Hackenberg L, Liljenqvist U. Dural-rod correction and instrumentation of idiopathic scoliosis with the Halm-Zielke instrumentation. Spine. 2003; 28:1306–1313.23). Lowe TG, Alongi PR, Smith DA, O'Brien MF, Mitchell SL, Pinteric RJ. Anterior single rod instrumentation for thoracolumbar adolescent idiopathic scoliosis with and without the use of structural interbody support. Spine. 2003; 28:2232–2242.
Article24). Bernhardt M, Bridwell K. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spine and the thoracolumbar junction. Spine. 1989; 14:717–721.25). Bullmann V, Fallenberg EM, Meier N, et al. Anterior dual rod instrumentation in idiopathic thoracic scoliosis.: a computed tomography analysis of screw placement relative to the aorta and the spinal canal. Spine. 2005; 30:2078–2083.26). Liljenqvist UR, Bullmann V, Schulte TL, Hackenberg L, Halm HF. Anterior dual rod instrumentation in idiopathic thoracic scoliosis. Eur Spine J. 2006; 15:1118–1127.
Article27). Muschik MT, Kimmich H, Demmel T. Comparison of anterior and posterior duble-rod instrumentation for thoracic idiopathic scoliosis: results of 141 patients. Eur Spine J;. 2006. 1128–1138.28). Newton PO, Parent S, Marks M, Pawelek J. Prospective evaluation of 50 consecutive scoliosis patients surgically treated with thoracoscopic anterior instrumentation. Spine. 2005; 30:100–109.
Article29). Dick JC, Bourgeault CA. Notch sensitivity of titanium alloy, commercially pure titanium, and stainless steel spinal implants. Spine. 2001; 26:1668–1672.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Video-Assisted Thoracoscopic Surgery for Correction of Adolescent Idiopatic Scoliosis: Comparison of 4.5 mm versus 5.5 mm Rod Constructs
- An Innovative Universal Screw Removal Instrument
- Spinopelvic Fixation
- Choice of Rods in Surgical Treatment of Adolescent Idiopathic Scoliosis: What Are the Clinical Implications of Biomechanical Properties? – A Review of the Literature
- Metal Failure in patients with Short-segmental Pedicle Screw Fixation and Fusion for Degenerative Lumbar Disease: Comparison Monoaxial with Polyaxial Screw