Clin Endosc.
2023 Sep;56(5):546-552. 10.5946/ce.2023.015.
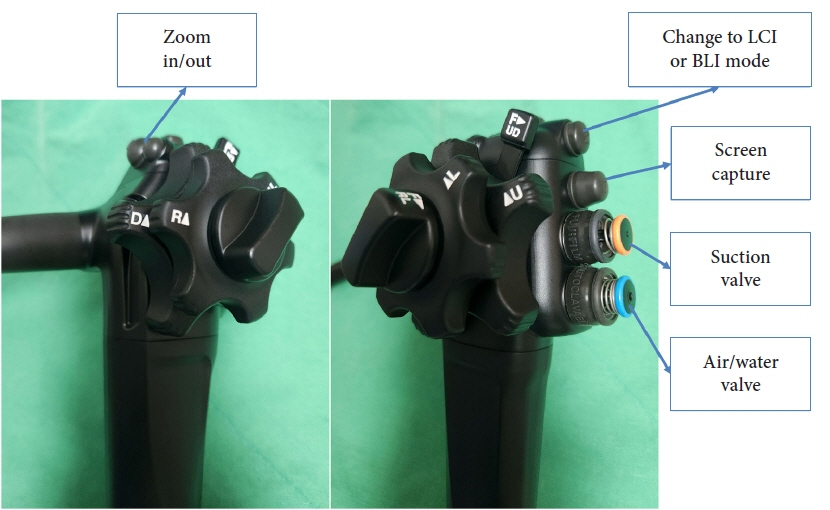
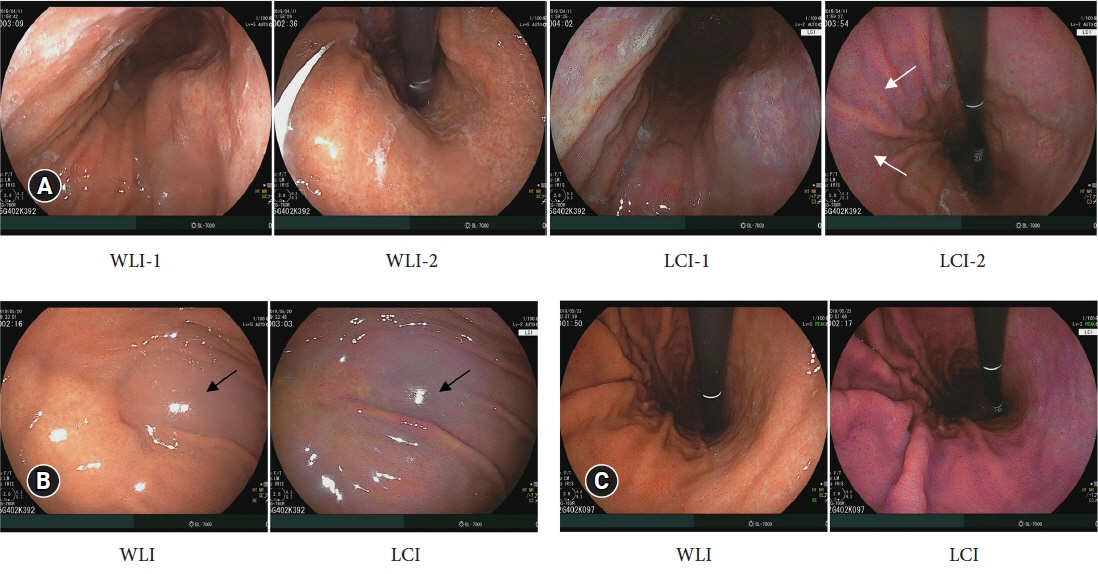
Role of linked color imaging for upper gastrointestinal disease: present and future
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea
- KMID: 2546132
- DOI: http://doi.org/10.5946/ce.2023.015
Abstract
- Techniques for upper gastrointestinal endoscopy are advancing to facilitate lesion detection and improve prognosis. However, most early tumors in the upper gastrointestinal tract exhibit subtle color changes or morphological features that are difficult to detect using white light imaging. Linked color imaging (LCI) has been developed to overcome these shortcomings; it expands or reduces color information to clarify color differences, thereby facilitating the detection and observation of lesions. This article summarizes the characteristics of LCI and advances in LCI-related research in the upper gastrointestinal tract field.
Figure
Reference
-
1. Osawa H, Miura Y, Takezawa T, et al. Linked color imaging and blue laser imaging for upper gastrointestinal screening. Clin Endosc. 2018; 51:513–526.2. Sakamoto T, Cho H, Saito Y. Clinical applications of linked color imaging and blue laser/light imaging in the screening, diagnosis, and treatment of superficial colorectal tumors. Clin Endosc. 2021; 54:488–493.3. Kaise M, Kato M, Urashima M, et al. Magnifying endoscopy combined with narrow-band imaging for differential diagnosis of superficial depressed gastric lesions. Endoscopy. 2009; 41:310–315.4. Nakayoshi T, Tajiri H, Matsuda K, et al. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004; 36:1080–1084.5. Yao K, Oishi T, Matsui T, et al. Novel magnified endoscopic findings of microvascular architecture in intramucosal gastric cancer. Gastrointest Endosc. 2002; 56:279–284.6. Hiraoka Y, Miura Y, Osawa H, et al. Appropriate color enhancement settings for blue laser imaging facilitates the diagnosis of early gastric cancer with high color contrast. J Gastric Cancer. 2021; 21:142–154.7. Ishimura N, Okimoto E, Shibagaki K, et al. Endoscopic diagnosis and screening of Barrett's esophagus: inconsistency of diagnostic criteria between Japan and Western countries. DEN Open. 2021; 2:e73.8. Takeda T, Nagahara A, Ishizuka K, et al. Improved visibility of Barrett’s esophagus with linked color imaging: inter- and intra-rater reliability and quantitative analysis. Digestion. 2018; 97:183–194.9. de Groof AJ, Fockens KN, Struyvenberg MR, et al. Blue-light imaging and linked-color imaging improve visualization of Barrett’s neoplasia by nonexpert endoscopists. Gastrointest Endosc. 2020; 91:1050–1057.10. Saito M, Koike T, Ohara Y, et al. Linked-color imaging may help improve the visibility of superficial Barrett’s esophageal adenocarcinoma by increasing the color difference. Intern Med. 2021; 60:3351–3358.11. Tokunaga M, Matsumura T, Ishikawa K, et al. The efficacy of linked color imaging in the endoscopic diagnosis of Barrett’s esophagus and esophageal adenocarcinoma. Gastroenterol Res Pract. 2020; 2020:9604345.12. Nakamura K, Urabe Y, Oka S, et al. Usefulness of linked color imaging in the early detection of superficial esophageal squamous cell carcinomas. Esophagus. 2021; 18:118–124.13. Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999; 45:172–180.14. Miwa H, Yokoyama T, Hori K, et al. Interobserver agreement in endoscopic evaluation of reflux esophagitis using a modified Los Angeles classification incorporating grades N and M: a validation study in a cohort of Japanese endoscopists. Dis Esophagus. 2008; 21:355–363.15. Amano Y, Ishimura N, Furuta K, et al. Interobserver agreement on classifying endoscopic diagnoses of nonerosive esophagitis. Endoscopy. 2006; 38:1032–1035.16. Takeda T, Asaoka D, Abe D, et al. Linked color imaging improves visibility of reflux esophagitis. BMC Gastroenterol. 2020; 20:356.17. Lee SP, Kae SH, Jang HJ, et al. Inter-observer variability of experts and trainees for the diagnosis of reflux esophagitis: comparison of linked color imaging, blue laser imaging, and white light imaging. J Dig Dis. 2021; 22:425–432.18. Ono S, Dohi O, Yagi N, et al. Accuracies of endoscopic diagnosis of Helicobacter pylori-gastritis: multicenter prospective study using white light imaging and linked color imaging. Digestion. 2020; 101:624–630.19. Chen H, Wang H, Wu X, et al. Predictability of gastric intestinal metaplasia by patchy lavender color seen on linked color imaging endoscopy. Lasers Med Sci. 2019; 34:1791–1797.20. Dohi O, Ono S, Kawada K, et al. Linked color imaging provides enhanced visibility with a high color difference in upper gastrointestinal neoplasms. J Gastroenterol Hepatol. 2023; 38:79–86.21. Yoshifuku Y, Sanomura Y, Oka S, et al. Evaluation of the visibility of early gastric cancer using linked color imaging and blue laser imaging. BMC Gastroenterol. 2017; 17:150.22. Fockens K, de Groof J, van der Putten J, et al. Linked color imaging improves identification of early gastric cancer lesions by expert and non-expert endoscopists. Surg Endosc. 2022; 36:8316–8325.23. Ono S, Kawada K, Dohi O, et al. Linked color imaging focused on neoplasm detection in the upper gastrointestinal tract: a randomized trial. Ann Intern Med. 2021; 174:18–24.24. Gao J, Zhang X, Meng Q, et al. Linked color imaging can improve detection rate of early gastric cancer in a high-risk population: a multi-center randomized controlled clinical trial. Dig Dis Sci. 2021; 66:1212–1219.25. Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015; 64:1353–1367.26. Belair PA, Metz DC, Faigel DO, et al. Receiver operator characteristic analysis of endoscopy as a test for gastritis. Dig Dis Sci. 1997; 42:2227–2233.27. Okamura T, Iwaya Y, Kitahara K, et al. Accuracy of endoscopic diagnosis for mild atrophic gastritis infected with Helicobacter pylori. Clin Endosc. 2018; 51:362–367.28. Redéen S, Petersson F, Jönsson KA, et al. Relationship of gastroscopic features to histological findings in gastritis and Helicobacter pylori infection in a general population sample. Endoscopy. 2003; 35:946–950.29. Dohi O, Yagi N, Onozawa Y, et al. Linked color imaging improves endoscopic diagnosis of active Helicobacter pylori infection. Endosc Int Open. 2016; 4:E800–E805.30. Takeda T, Asaoka D, Nojiri S, et al. Linked color imaging and the Kyoto classification of gastritis: evaluation of visibility and inter-rater reliability. Digestion. 2020; 101:598–607.31. Chen TH, Hsu CM, Cheng HT, et al. Linked color imaging can help gastric Helicobacter pylori infection diagnosis during endoscopy. J Chin Med Assoc. 2018; 81:1033–1037.32. Jiang ZX, Nong B, Liang LX, et al. Differential diagnosis of Helicobacter pylori-associated gastritis with the linked-color imaging score. Dig Liver Dis. 2019; 51:1665–1670.33. Sakae H, Kanzaki H, Satomi T, et al. Linked color imaging (LCI) emphasizes the color changes in the gastric mucosa after Helicobacter pylori eradication. Dig Dis Sci. 2022; 67:2375–2384.34. Lee SP, Lee J, Kae SH, et al. The role of linked color imaging in endoscopic diagnosis of Helicobacter pylori associated gastritis. Scand J Gastroenterol. 2020; 55:1114–1120.35. Yasuda T, Hiroyasu T, Hiwa S, et al. Potential of automatic diagnosis system with linked color imaging for diagnosis of Helicobacter pylori infection. Dig Endosc. 2020; 32:373–381.36. Nakashima H, Kawahira H, Kawachi H, et al. Endoscopic three-categorical diagnosis of Helicobacter pylori infection using linked color imaging and deep learning: a single-center prospective study (with video). Gastric Cancer. 2020; 23:1033–1040.37. Nakashima H, Kawahira H, Kawachi H, et al. Artificial intelligence diagnosis of Helicobacter pylori infection using blue laser imaging-bright and linked color imaging: a single-center prospective study. Ann Gastroenterol. 2018; 31:462–468.38. Bang CS, Lee JJ, Baik GH. Artificial intelligence for the prediction of Helicobacter pylori infection in endoscopic images: systematic review and meta-analysis of diagnostic test accuracy. J Med Internet Res. 2020; 22:e21983.39. Haruma K, Kato M, Kawada K, et al. Diagnostic ability of linked color imaging in ultraslim endoscopy to identify neoplastic lesions in the upper gastrointestinal tract. Endosc Int Open. 2022; 10:E88–E95.40. Hiraoka Y, Miura Y, Osawa H, et al. Linked color imaging demonstrates characteristic findings in semi-pedunculated gastric adenocarcinoma in Helicobacter pylori-negative normal mucosa. Clin Endosc. 2021; 54:136–138.41. Kim SH, Hong SJ. Current status of image-enhanced endoscopy for early identification of esophageal neoplasms. Clin Endosc. 2021; 54:464–476.42. Lee W. Application of current image-enhanced endoscopy in gastric diseases. Clin Endosc. 2021; 54:477–487.43. Abe Y, Sasaki Y, Yagi M, et al. Linked color imaging improves the diagnostic accuracy of eosinophilic esophagitis. DEN Open. 2022; 3:e146.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Linked Color Imaging and Blue Laser Imaging for Upper Gastrointestinal Screening
- Detection of Gastrointestinal Cancer using Linked Color Imaging and Blue Light Imaging
- Image-enhanced endoscopy in upper gastrointestinal disease: focusing on texture and color enhancement imaging and red dichromatic imaging
- Role of endoscopy in gastroesophageal reflux disease
- Advanced Imaging Technology Other than Narrow Band Imaging