Cancer Res Treat.
2023 Jul;55(3):851-864. 10.4143/crt.2022.1527.
Combination of the LARS1 Inhibitor, BC-LI-0186 with a MEK1/2 Inhibitor Enhances the Anti-Tumor Effect in Non–Small Cell Lung Cancer
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Yonsei Institute of Pharmaceutical Sciences, College of Pharmacy, Yonsei University, Incheon, Korea
- 3Department of Biotechnology, Yonsei University, Seoul, Korea
- KMID: 2544166
- DOI: http://doi.org/10.4143/crt.2022.1527
Abstract
- Purpose
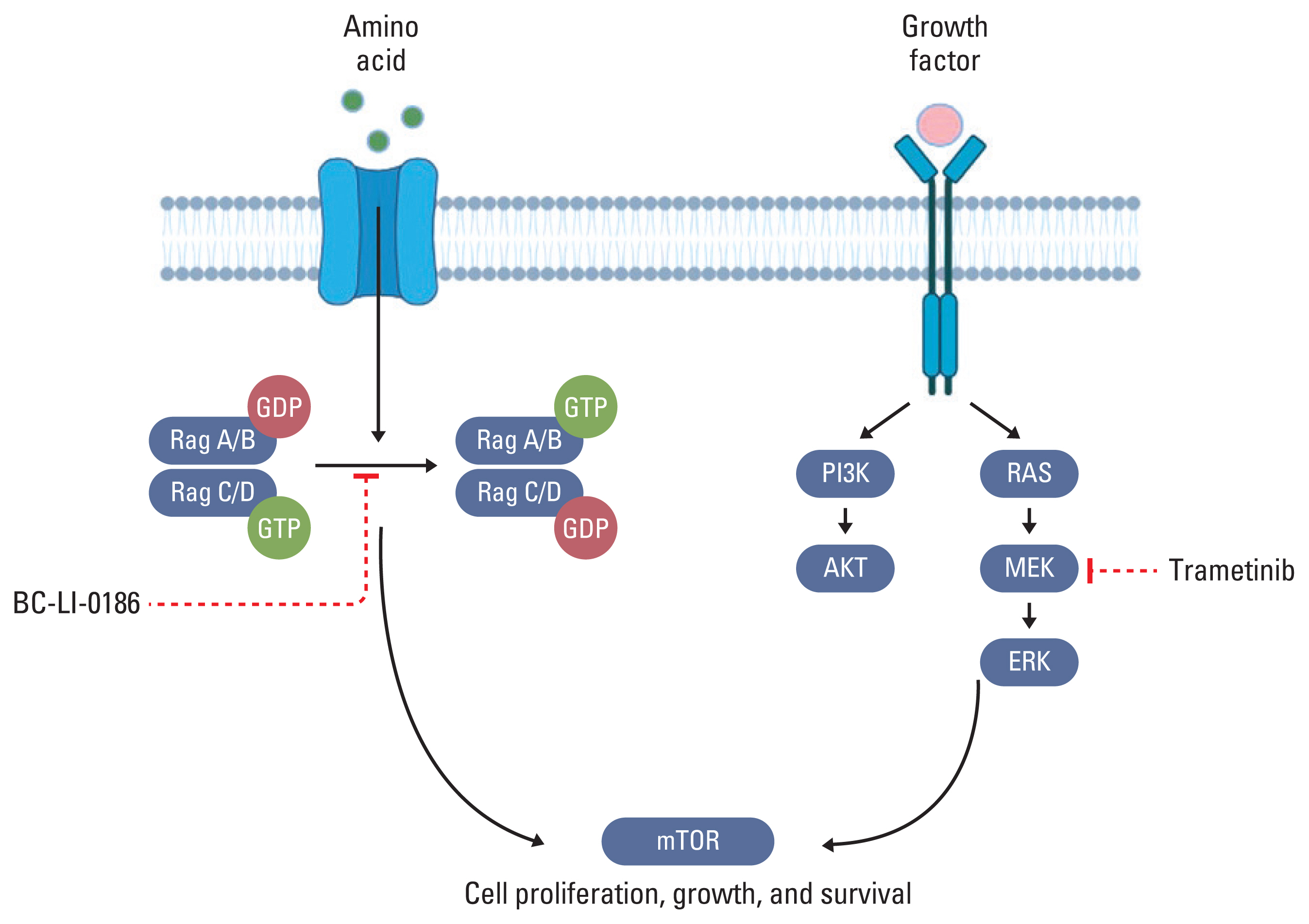
The mammalian target of rapamycin complex 1 (mTORC1) regulates cell growth and proliferation by growth factor coordination and amino acid availability. Leucyl-tRNA synthetase 1 (LARS1) senses the intracellular leucine concentration and mediates amino acid-induced activation of mTORC1. Thus, LARS1 inhibition could be useful in cancer treatment. However, the fact that mTORC1 can be stimulated by various growth factors and amino acids suggests that LARS1 inhibition alone has limitations in inhibiting cell growth and proliferation. We investigated the combined effects of BC-LI-0186, a LARS1 inhibitor, and trametinib, an MEK inhibitor, on non–small cell lung cancer (NSCLC).
Materials and Methods
Protein expression and phosphorylation were observed by immunoblotting, and genes differentially expressed between BC-LI-0186–sensitive and –resistant cells were identified by RNA sequencing. The combined effect of the two drugs was inferred from the combination index values and a xenograft model.
Results
LARS1 expression was positively correlated with mTORC1 in NSCLC cell lines. BC-LI-0186 treatment of A549 and H460 cells maintained in media supplemented with fetal bovine serum revealed paradoxical phosphorylation of S6 and activation of mitogen- activated protein kinase (MAPK) signaling. Compared with BC-LI-0186–sensitive cells, –resistant cells showed enrichment of the MAPK gene set. The combination of trametinib and BC-LI-0186 inhibited the phosphorylation of S6, MEK, and extracellular signal-regulated kinase and their synergistic effects were confirmed in a mouse xenograft model.
Conclusion
The combination of BC-LI-0186 and trametinib inhibited the non-canonical mTORC1-activating function of LARS1. Our study demonstrated a new therapeutic approach for NSCLC without targetable driver mutations.
Keyword
Figure
Reference
-
References
1. Bade BC, Dela Cruz CS. Lung cancer 2020: epidemiology, etiology, and prevention. Clin Chest Med. 2020; 41:1–24.2. Kim EY, Lee JG, Lee JM, Kim A, Yoo HC, Kim K, et al. Therapeutic effects of the novel Leucyl-tRNA synthetase inhibitor BC-LI-0186 in non-small cell lung cancer. Ther Adv Med Oncol. 2019; 11:1758835919846798.
Article3. Mamdani H, Matosevic S, Khalid AB, Durm G, Jalal SI. Immunotherapy in lung cancer: current landscape and future directions. Front Immunol. 2022; 13:823618.
Article4. Alamgeer M, Ganju V, Watkins DN. Novel therapeutic targets in non-small cell lung cancer. Curr Opin Pharmacol. 2013; 13:394–401.
Article5. Savas P, Hughes B, Solomon B. Targeted therapy in lung cancer: IPASS and beyond, keeping abreast of the explosion of targeted therapies for lung cancer. J Thorac Dis. 2013; 5 Suppl 5:S579–92.6. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011; 144:646–74.
Article7. Xie J, Wang X, Proud CG. mTOR inhibitors in cancer therapy. F1000Res. 2016; 5:2078.
Article8. Tian T, Li X, Zhang J. mTOR signaling in cancer and mTOR inhibitors in solid tumor targeting therapy. Int J Mol Sci. 2019; 20:755.
Article9. Kim JH, Lee C, Lee M, Wang H, Kim K, Park SJ, et al. Control of leucine-dependent mTORC1 pathway through chemical intervention of leucyl-tRNA synthetase and RagD interaction. Nat Commun. 2017; 8:732.
Article10. Han JM, Jeong SJ, Park MC, Kim G, Kwon NH, Kim HK, et al. Leucyl-tRNA synthetase is an intracellular leucine sensor for the mTORC1-signaling pathway. Cell. 2012; 149:410–24.
Article11. Odogwu L, Mathieu L, Blumenthal G, Larkins E, Goldberg KB, Griffin N, et al. FDA approval summary: dabrafenib and trametinib for the treatment of metastatic non-small cell lung cancers harboring BRAF V600E mutations. Oncologist. 2018; 23:740–5.12. Roman M, Baraibar I, Lopez I, Nadal E, Rolfo C, Vicent S, et al. KRAS oncogene in non-small cell lung cancer: clinical perspectives on the treatment of an old target. Mol Cancer. 2018; 17:33.
Article13. Euhus DM, Hudd C, LaRegina MC, Johnson FE. Tumor measurement in the nude mouse. J Surg Oncol. 1986; 31:229–34.14. Tomayko MM, Reynolds CP. Determination of subcutaneous tumor size in athymic (nude) mice. Cancer Chemother Pharmacol. 1989; 24:148–54.
Article15. Chou TC. Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Res. 2010; 70:440–6.
Article16. Sanaei MJ, Razi S, Pourbagheri-Sigaroodi A, Bashash D. The PI3K/Akt/mTOR pathway in lung cancer; oncogenic alterations, therapeutic opportunities, challenges, and a glance at the application of nanoparticles. Transl Oncol. 2022; 18:101364.
Article17. Cheng H, Shcherba M, Pendurti G, Liang Y, Piperdi B, Perez-Soler R. Targeting the PI3K/AKT/mTOR pathway: potential for lung cancer treatment. Lung Cancer Manag. 2014; 3:67–75.
Article18. McCubrey JA, Steelman LS, Chappell WH, Abrams SL, Wong EW, Chang F, et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance. Biochim Biophys Acta. 2007; 1773:1263–84.19. Engelman JA, Chen L, Tan X, Crosby K, Guimaraes AR, Upadhyay R, et al. Effective use of PI3K and MEK inhibitors to treat mutant Kras G12D and PIK3CA H1047R murine lung cancers. Nat Med. 2008; 14:1351–6.
Article20. Sos ML, Fischer S, Ullrich R, Peifer M, Heuckmann JM, Koker M, et al. Identifying genotype-dependent efficacy of single and combined PI3K- and MAPK-pathway inhibition in cancer. Proc Natl Acad Sci U S A. 2009; 106:18351–6.
Article21. Grilley-Olson JE, Bedard PL, Fasolo A, Cornfeld M, Cartee L, Razak AR, et al. A phase Ib dose-escalation study of the MEK inhibitor trametinib in combination with the PI3K/mTOR inhibitor GSK2126458 in patients with advanced solid tumors. Invest New Drugs. 2016; 34:740–9.22. Soares HP, Ming M, Mellon M, Young SH, Han L, Sinnet-Smith J, et al. Dual PI3K/mTOR inhibitors induce rapid overactivation of the MEK/ERK pathway in human pancreatic cancer cells through suppression of mTORC2. Mol Cancer Ther. 2015; 14:1014–23.
Article23. Lawal B, Lo WC, Mokgautsi N, Sumitra MR, Khedkar H, Wu AT, et al. Erratum: A preclinical report of a cobimetinib-inspired novel anticancer small-molecule scaffold of isoflavones, NSC777213, for targeting PI3K/AKT/mTOR/MEK in multiple cancers. Am J Cancer Res. 2021; 11:5761.24. Blumenschein GR Jr, Smit EF, Planchard D, Kim DW, Cadranel J, De Pas T, et al. A randomized phase II study of the MEK1/MEK2 inhibitor trametinib (GSK1120212) compared with docetaxel in KRAS-mutant advanced non-small-cell lung cancer (NSCLC)dagger. Ann Oncol. 2015; 26:894–901.25. Ekman S, Wynes MW, Hirsch FR. The mTOR pathway in lung cancer and implications for therapy and biomarker analysis. J Thorac Oncol. 2012; 7:947–53.26. Paver E, O’Toole S, Cheng XM, Mahar A, Cooper WA. Updates in the molecular pathology of non-small cell lung cancer. Semin Diagn Pathol. 2021; 38:54–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implication of leucyl-tRNA synthetase 1 (LARS1) over-expression in growth and migration of lung cancer cells detected by siRNA targeted knock-down analysis
- Treatment Effect of Combining Lenvatinib and Vemurafenib for BRAF Mutated Anaplastic Thyroid Cancer
- Autophagy Inhibition with Monensin Enhances Cell Cycle Arrest and Apoptosis Induced by mTOR or Epidermal Growth Factor Receptor Inhibitors in Lung Cancer Cells
- Histone Deacetylase as a Valuable Predictive Biomarker and Therapeutic Target in Immunotherapy for Non-Small Cell Lung Cancer
- The Immunohistochemical analysis for the expression of survivin, an inhibitor of apoptosis protein, in non-small cell lung cancer