Endocrinol Metab.
2020 Dec;35(4):925-932. 10.3803/EnM.2020.725.
Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Medical Informatics, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2511020
- DOI: http://doi.org/10.3803/EnM.2020.725
Abstract
- Background
Concomitant papillary thyroid cancer (PTC) and hyperparathyroidism (HPT) have been reported in several studies. Our study aimed to investigate the incidence of concomitant PTC in HPT patients upon preoperative diagnosis and present a clinical opinion on detecting thyroid malignancy in case of parathyroidectomy.
Methods
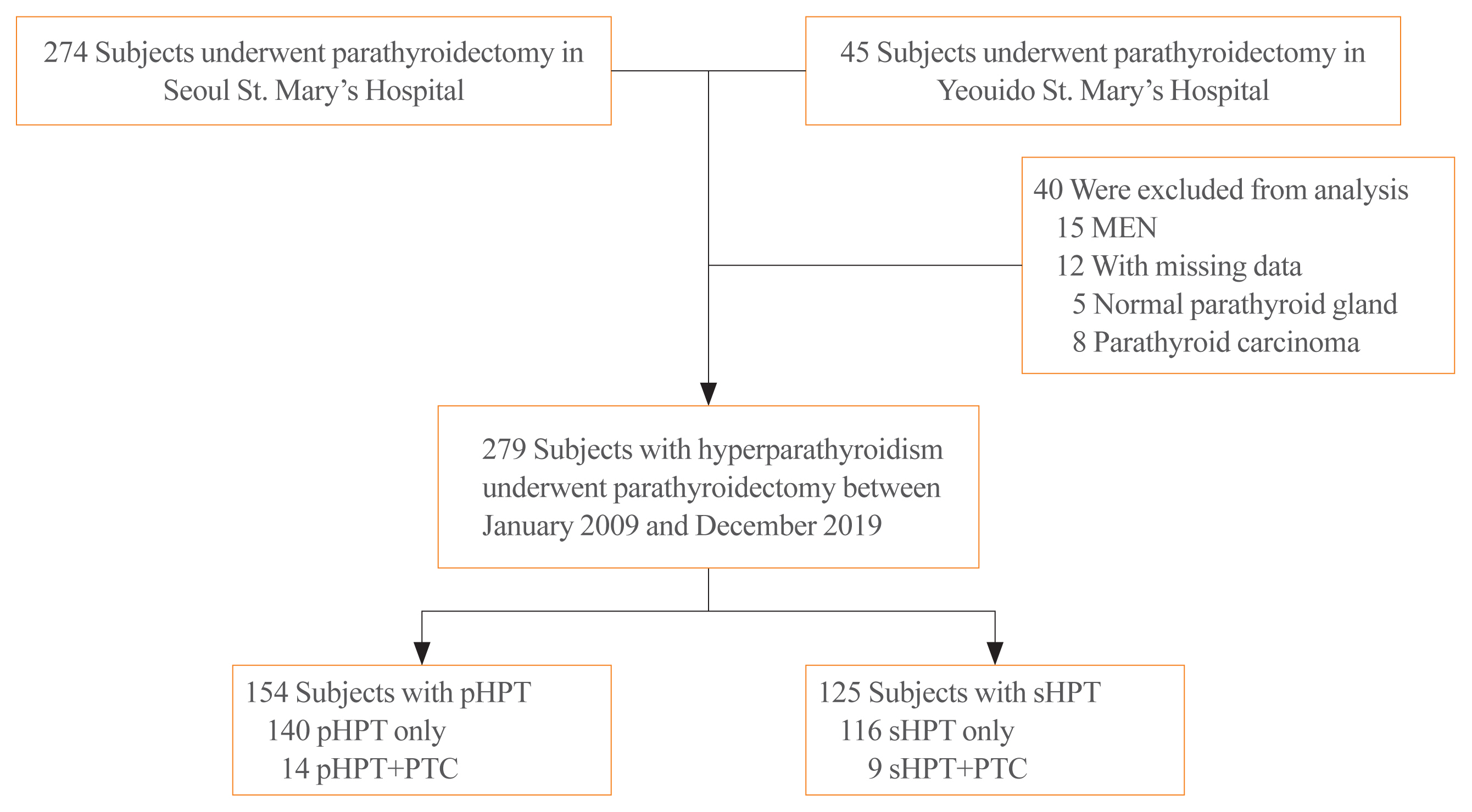
Patients who underwent parathyroidectomy between January 2009 and December 2019 in two medical centers were included. Of the 279 participants 154 were diagnosed as primary hyperparathyroidism (pHPT) and 125 as secondary hyperparathyroidism (sHPT). The incidence of concomitant PTC and its clinical characteristics were compared with 98 patients who underwent thyroidectomy and were diagnosed with classical PTC during the same period.
Results
Concurrent PTC was detected in 14 patients (9.1%) with pHPT and in nine patients (7.2%) with sHPT. Ten (71.4%) and seven (77.8%) PTCs were microcarcinomas in the pHPT and sHPT cases respectively. In the pHPT patients, vitamin D was lower in the pHPT+PTC group (13.0±3.7 ng/mL) than in the pHPT-only group (18.5±10.4 ng/mL; P=0.01). Vitamin D levels were also lower in the sHPT+PTC group (12.3±5.6 ng/mL) than in the sHPT-only group (18.0±10.2 ng/mL; P=0.12). In the concomitant PTC group, lymph node ratio was higher than in the classical PTC group (P=0.00).
Conclusion
A high prevalence of concomitant PTC was seen in patients with pHPT and sHPT. Those concomitant PTCs were mostly microcarcinomas and had more aggressive features, suggesting that efforts should be made to detect concomitant malignancies in the preoperative parathyroidectomy evaluation.
Keyword
Figure
Cited by 2 articles
-
Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (
Endocrinol Metab 2020;35:925–32, Chaiho Jeong et al.)
Chaiho Jeong, Jeonghoon Ha, Moo Il Kang
Endocrinol Metab. 2021;36(1):205-206. doi: 10.3803/EnM.2021.100.Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (
Endocrinol Metab 2020;35:925–32, Chaiho Jeong et al.)
Burcu Candemir, Coşkun Meriç
Endocrinol Metab. 2021;36(1):203-204. doi: 10.3803/EnM.2021.963.
Reference
-
1. Heath DA. Primary hyperparathyroidism. Clinical presentation and factor influencing clinical management. Endocrinol Metab Clin North Am. 1989; 18:631–46.2. Darba J, Marsa A. Epidemiology and management of parathyroid gland disorders in Spain over 15 years: a retrospective multicentre analysis. PLoS One. 2020; 15:e0230130.
Article3. Collier A, Portelli M, Ghosh S, Nowell S, Clark D. Primary hyperparathyroidism: increasing prevalence, social deprivation, and surgery. Endocr Res. 2017; 42:31–5.
Article4. Fraser WD. Hyperparathyroidism. Lancet. 2009; 374:145–58.
Article5. Pitt SC, Sippel RS, Chen H. Secondary and tertiary hyperparathyroidism, state of the art surgical management. Surg Clin North Am. 2009; 89:1227–39.
Article6. Kim SM, Long J, Montez-Rath ME, Leonard MB, Norton JA, Chertow GM. Rates and outcomes of parathyroidectomy for secondary hyperparathyroidism in the United States. Clin J Am Soc Nephrol. 2016; 11:1260–7.
Article7. Ogburn PL, Black BM. Primary hyperparathyroidism and papillary adenocarcinoma of the thyroid: report of four cases. Proc Staff Meet Mayo Clin. 1956; 31:295–8.8. Yazici P, Mihmanli M, Bozdag E, Aygun N, Uludag M. Incidental finding of papillary thyroid carcinoma in the patients with primary hyperparathyroidism. Eurasian J Med. 2015; 47:194–8.
Article9. Cinamon U, Levy D, Marom T. Is primary hyperparathyroidism a risk factor for papillary thyroid cancer? An exemplar study and literature review. Int Arch Otorhinolaryngol. 2015; 19:42–5.10. Burmeister LA, Sandberg M, Carty SE, Watson CG. Thyroid carcinoma found at parathyroidectomy: association with primary, secondary, and tertiary hyperparathyroidism. Cancer. 1997; 79:1611–6.11. Smit PC, Borel Rinkes IH, van Dalen A, van Vroonhoven TJ. Direct, minimally invasive adenomectomy for primary hyperparathyroidism: an alternative to conventional neck exploration? Ann Surg. 2000; 231:559–65.12. Wright MC, Jensen K, Mohamed H, Drake C, Mohsin K, Monlezun D, et al. Concomitant thyroid disease and primary hyperparathyroidism in patients undergoing parathyroidectomy or thyroidectomy. Gland Surg. 2017; 6:368–74.
Article13. Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014; 99:3561–9.
Article14. Lau WL, Obi Y, Kalantar-Zadeh K. Parathyroidectomy in the management of secondary hyperparathyroidism. Clin J Am Soc Nephrol. 2018; 13:952–61.15. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; 17:370–95.
Article16. Ha J, Lee J, Jo K, Han JS, Kim MH, Jung CK, et al. Calcification patterns in papillary thyroid carcinoma are associated with changes in thyroid hormones and coronary artery calcification. J Clin Med. 2018; 7:183.
Article17. Yi KH, Lee EK, Kang HC, Koh Y, Kim SW, Kim IJ, et al. 2016 Revised Korean Thyroid Association management guidelines for patients with thyroid nodules and thyroid cancer. Int J Thyroidol. 2016; 9:59–126.
Article18. Preda C, Branisteanu D, Armasu I, Danila R, Velicescu C, Ciobanu D, et al. Coexistent papillary thyroid carcinoma diagnosed in surgically treated patients for primary versus secondary hyperparathyroidism: same incidence, different characteristics. BMC Surg. 2019; 19:94.
Article19. Pickard AL, Gridley G, Mellemkjae L, Johansen C, Kofoed-Enevoldsen A, Cantor KP, et al. Hyperparathyroidism and subsequent cancer risk in Denmark. Cancer. 2002; 95:1611–7.
Article20. Geara AS, Castellanos MR, Bassil C, Schuller-Levis G, Park E, Smith M, et al. Effects of parathyroid hormone on immune function. Clin Dev Immunol. 2010; 2010:418695.
Article21. McCarty MF. Parathyroid hormone may be a cancer promoter: an explanation for the decrease in cancer risk associated with ultraviolet light, calcium, and vitamin D. Med Hypotheses. 2000; 54:475–82.22. Maiorano E, Ambrosi A, Giorgino R, Fersini M, Pollice L, Ciampolillo A. Insulin-like growth factor 1 (IGF-1) in multinodular goiters: a possible pathogenetic factor. Pathol Res Pract. 1994; 190:1012–6.
Article23. Vargas-Ortega G, Balcazar-Hernandez L, Gonzalez-Virla B, Ramirez-Renteria C, Nieto-Guzman O, Garrido-Mendoza AP, et al. Symptomatic primary hyperparathyroidism as a risk factor for differentiated thyroid cancer. J Thyroid Res. 2018; 2018:9461079.
Article24. Beebeejaun M, Chinnasamy E, Wilson P, Sharma A, Beharry N, Bano G. Papillary carcinoma of the thyroid in patients with primary hyperparathyroidism: is there a link? Med Hypotheses. 2017; 103:100–4.
Article25. Kim D. The role of vitamin D in thyroid diseases. Int J Mol Sci. 2017; 18:1949.
Article26. Roskies M, Dolev Y, Caglar D, Hier MP, Mlynarek A, Majdan A, et al. Vitamin D deficiency as a potentially modifiable risk factor for thyroid cancer. J Otolaryngol Head Neck Surg. 2012; 41:160–3.27. Kim JR, Kim BH, Kim SM, Oh MY, Kim WJ, Jeon YK, et al. Low serum 25 hydroxyvitamin D is associated with poor clinicopathologic characteristics in female patients with papillary thyroid cancer. Thyroid. 2014; 24:1618–24.
Article28. Wee JH, Cho SW, Kim JW, Rhee CS. Serum vitamin D levels in a healthy Korean population. J Allergy Clin Immunol. 2018; 141(2 Suppl):AB77.
Article29. Jeon MJ, Chung MS, Kwon H, Kim M, Park S, Baek JH, et al. Features of papillary thyroid microcarcinoma associated with lateral cervical lymph node metastasis. Clin Endocrinol (Oxf). 2017; 86:845–51.
Article30. Jeon MJ, Kim WG, Choi YM, Kwon H, Lee YM, Sung TY, et al. Features predictive of distant metastasis in papillary thyroid microcarcinomas. Thyroid. 2016; 26:161–8.
Article31. Kim SK, Park I, Woo JW, Lee JH, Choe JH, Kim JH, et al. Predictive factors for lymph node metastasis in papillary thyroid microcarcinoma. Ann Surg Oncol. 2016; 23:2866–73.
Article32. Lee J, Lee SG, Kim K, Yim SH, Ryu H, Lee CR, et al. Clinical value of lymph node ratio integration with the 8th edition of the UICC TNM classification and 2015 ATA risk stratification systems for recurrence prediction in papillary thyroid cancer. Sci Rep. 2019; 9:13361.
Article33. Cetin K, Sikar HE, Temizkan S, Ofluoglu CB, Ozderya A, Aydin K, et al. Does primary hyperparathyroidism have an association with thyroid papillary cancer? A retrospective cohort study. World J Surg. 2019; 43:1243–8.
Article34. Haser GC, Tuttle RM, Su HK, Alon EE, Bergman D, Bernet V, et al. Active surveillance for papillary thyroid microcarcinoma: new challenges and opportunities for the health care system. Endocr Pract. 2016; 22:602–11.
Article35. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016; 151:959–68.
Article36. Vaiman M, Nagibin A, Olevson J. Complications in primary and completed thyroidectomy. Surg Today. 2010; 40:114–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Nodules in Patients with Secondary Hyperparathyroidism
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (Endocrinol Metab 2020;35:925-32, Chaiho Jeong et al.)
- Synchronous parathyroid carcinoma and papillary thyroid carcinoma in a patient with long-standing schizophrenia
- Primary Hyperparathyroidism, Concomitant Thyroid Papillary and Follicular Carcinomas on the Background of Hashimoto's: Interplay?