Korean J Gastroenterol.
2020 Mar;75(3):157-161. 10.4166/kjg.2020.75.3.157.
Phlegmonous Gastritis Caused by Penetration of a Toothpick
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Konyang University College of Medicine, Daejeon, Korea. ismkim@kyuh.ac.kr
- KMID: 2471899
- DOI: http://doi.org/10.4166/kjg.2020.75.3.157
Abstract
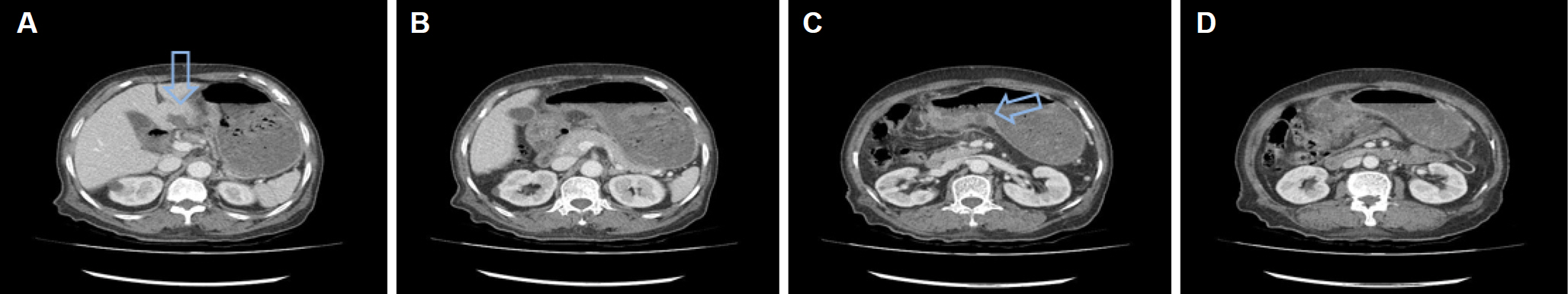
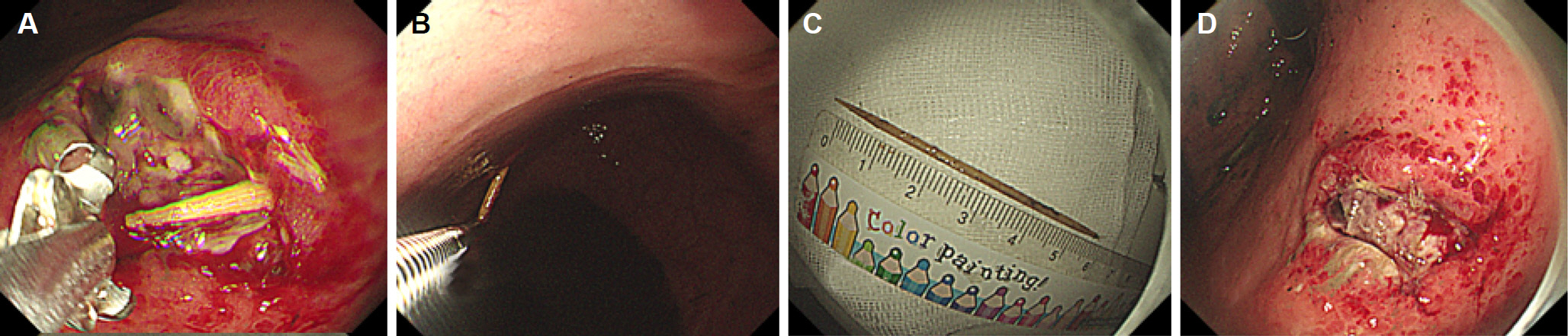
- Phlegmonous gastritis is a disease caused by a bacterial infection of the gastric wall. This condition is rare, but when it does occur, its prognosis appears to be poor. The underlying etiology is largely unknown, but an immunocompromised state is considered an important risk factor. An 85-year-old woman presented with a confused mentality, fever, epigastric pain, and melena. There was no history of alcohol drinking or smoking, nor of previous gastric surgery. On the other hand, there was a history of senile dementia and cognitive impairment. Initial contrast-enhanced abdominal CT revealed gastric wall edema at the antrum with mucosal hyper-enhancement and an abscess in the thickened antrum. Upper gastrointestinal endoscopy on the fourth hospital day showed dark-colored fluid retention in the stomach. The gastric mucosa was inflamed and friable, with several ulcerative lesions showing purulent discharge. A toothpick was found in the process of identifying the base of the ulcerative lesion and was removed. Eventually, phlegmonous gastritis due to the penetration of a toothpick was diagnosed. After endoscopic toothpick removal, the patient's symptoms improved dramatically. Serial endoscopy revealed improvement in the gastric mucosa. This case is an example of phlegmonous gastritis caused by a foreign substance in the gastric wall of a patient with senile dementia. During upper gastrointestinal endoscopy in this case, identification of the base of ulcerative lesion played a critical role in the diagnosis.
Keyword
MeSH Terms
-
Abscess
Aged, 80 and over
Alcohol Drinking
Alzheimer Disease
Bacterial Infections
Cellulitis*
Cognition Disorders
Dementia
Diagnosis
Edema
Endoscopy
Endoscopy, Gastrointestinal
Female
Fever
Foreign Bodies
Gastric Mucosa
Gastritis*
Hand
Humans
Melena
Prognosis
Risk Factors
Smoke
Smoking
Stomach
Tomography, X-Ray Computed
Ulcer
Smoke
Figure
Reference
-
References
1. Starr A, Wilson JM. Phlegmonous gastritis. Ann Surg. 1957; 145:88–93.
Article2. Kim GY, Ward J, Henessey B, et al. Phlegmonous gastritis: case report and review. Gastrointest Endosc. 2005; 61:168–174.
Article3. Miller AI, Smith B, Rogers AI. Phlegmonous gastritis. Gastroenterology. 1975; 68:231–238.
Article4. Joko T, Tanaka H, Hirakata H, et al. Phlegmonous gastritis in a haemodialysis patient with secondary amyloidosis. Nephrol Dial Transplant. 1999; 14:196–198.
Article5. Radhi J, Kamouna M, Nyssen J. Phlegmonous gastritis following coronary bypass surgery. Can J Gastroenterol. 1999; 13:837–839.
Article6. Yu QQ, Tariq A, Unger SW, Cabello-Inchausti B, Robinson MJ. Phlegmonous gastritis associated with Kaposi sarcoma: a case report and review of the literature. Arch Pathol Lab Med. 2004; 128:801–803.
Article7. Lee BS, Kim SM, Seong JK, et al. Phlegmonous gastritis after endoscopic mucosal fresection. Endoscopy. 2005; 37:490–493.8. Lee TH, Lee GS, Im EH, et al. A case of acute phlegmonous gastritis treated with antibiotics alone. Korean J Gastrointest Endosc. 2005; 31:44–48.9. Min JS, Cho CH, Cho KS, et al. Diffuse phlegmonous gastritis. Korean J Gastroenterol. 1980; 12:73–77.10. Choong NW, Levy MJ, Rajan E, Kolars JC. Intramural gastric abscess: case history and review. Gastrointest Endosc. 2003; 58:627–629.11. Wakayama T, Watanabe H, Ishizaki Y, et al. A case of phlegmonous esophagitis associated with diffuse phlegmonous gastritis. Am J Gastroenterol. 1994; 89:804–806.12. Lee BK, Park KT, Kim ES, et al. A case of phlegmonous gastritis. Korean J Med. 1988; 34:421–425.13. Choi KM, Kwon YJ, Park MG, et al. Two cases of acute phlegmonous gastritis. Korean J Gastrointest Endosc. 1995; 15:79–83.14. Waseem S, Moshiree B, Draganov PV. Gastroparesis: current diagnostic challenges and management considerations. World J Gastroenterol. 2009; 15:25–37.
Article15. Kan-no Y, Irisawa A, Takagi T, et al. Endosonographic diagnosis and follow-up of phlegmonous gastritis. J Clin Ultrasound. 2007; 35:524–526.
Article16. Iwakiri Y, Kabemura T, Yasuda D, et al. A case of acute phlegmonous gastritis successfully treated with antibiotics. J Clin Gastroenterol. 1999; 28:175–177.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Phlegmonous Gastritis Diagnosed Early Endoscopically and Treated Successfully with Antibiotics
- Two Cases of Acute Phlegmonous Gastritis
- A Case of Acute Phlegmonous Gastritis Diagnosed with Endoscopic Submucosal Biopsy and Bacterial Culture and Improved by Antibiotics Treatment
- A Case of Phlegmonous Gastritis Associated with Marked Gastric Distension
- Acute Phlegmonous Gastritis Developing after Endoscopic Submucosal Dissection That Was Successfully Treated by Antibiotics Alone