Korean J Radiol.
2019 Dec;20(12):1616-1626. 10.3348/kjr.2019.0363.
Intraindividual Comparison between Gadoxetate-Enhanced Magnetic Resonance Imaging and Dynamic Computed Tomography for Characterizing Focal Hepatic Lesions: A Multicenter, Multireader Study
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. kimnex@yuhs.ac
- 2Department of Radiology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 3Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4Department of Radiology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 5Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 7Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 8Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 9Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 10Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2471674
- DOI: http://doi.org/10.3348/kjr.2019.0363
Abstract
OBJECTIVE
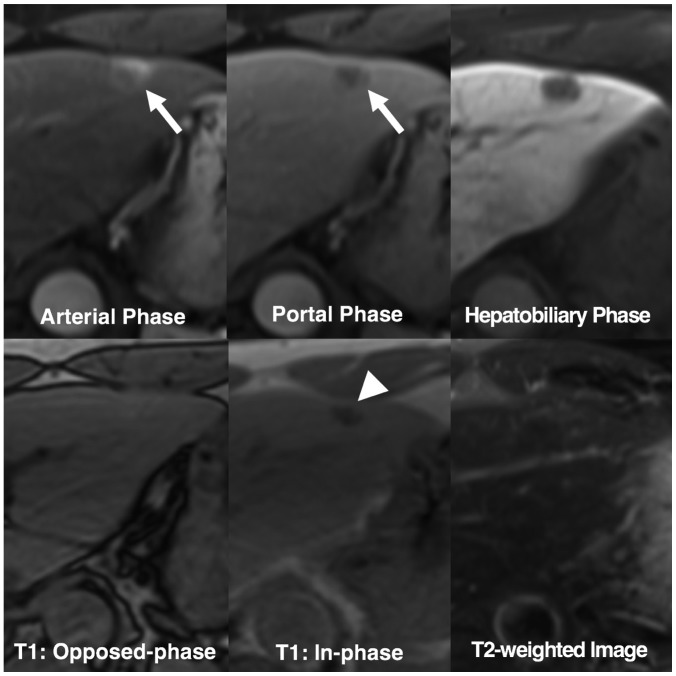
To compare the diagnostic accuracy of dynamic computed tomography (CT) and gadoxetate-enhanced magnetic resonance imaging (MRI) for characterization of hepatic lesions by using the Liver Imaging Reporting and Data System (LI-RADS) in a multicenter, off-site evaluation.
MATERIALS AND METHODS
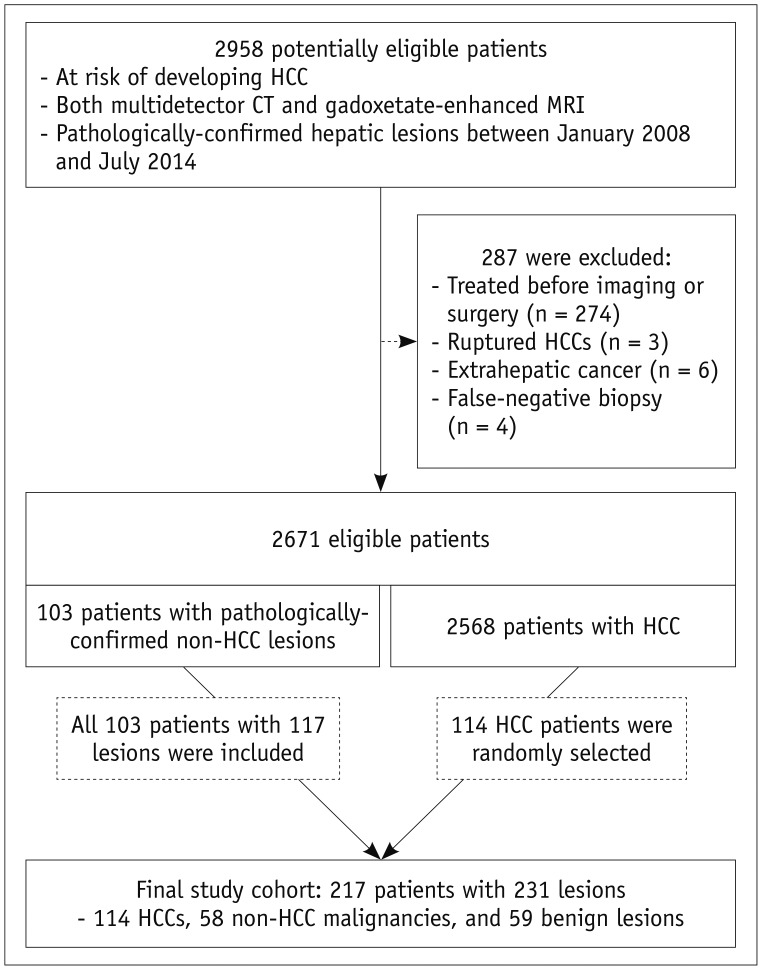
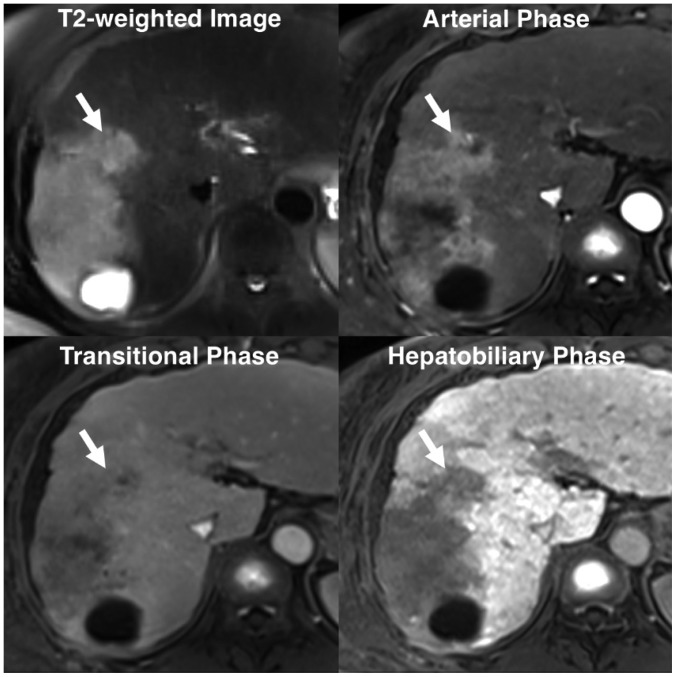
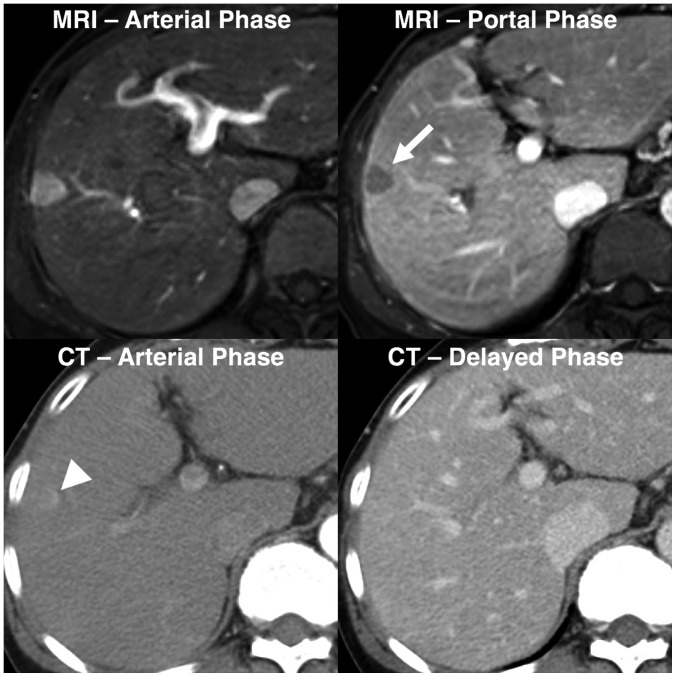
In this retrospective multicenter study, we evaluated 231 hepatic lesions (114 hepatocellular carcinomas [HCCs], 58 non-HCC malignancies, and 59 benign lesions) confirmed histologically in 217 patients with chronic liver disease who underwent both gadoxetate-enhanced MRI and dynamic CT at one of five tertiary hospitals. Four radiologists at different institutes independently reviewed all MR images first and the CT images 4 weeks later. They evaluated the major and ancillary imaging features and categorized each hepatic lesion according to the LI-RADS v2014. Diagnostic performance was calculated and compared using generalized estimating equations.
RESULTS
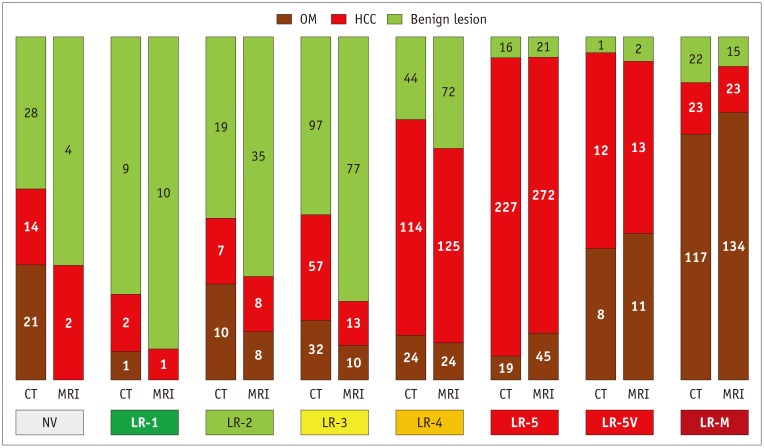
MRI showed higher sensitivity and accuracy than CT for diagnosing hepatic malignancies; the pooled sensitivities, specificities, and accuracies for categorizing LR-5/5V/M were 59.0% vs. 72.4% (CT vs. MRI; p < 0.001), 83.5% vs. 83.9% (p = 0.906), and 65.3% vs. 75.3% (p < 0.001), respectively. CT and MRI showed comparable capabilities for differentiating between HCC and other malignancies, with pooled accuracies of 79.9% and 82.4% for categorizing LR-M, respectively (p = 0.139).
CONCLUSION
Gadoxetate-enhanced MRI showed superior accuracy for categorizing LR-5/5V/M in hepatic malignancies in comparison with dynamic CT. Both modalities had comparable accuracies for distinguishing other malignancies from HCC.
Keyword
MeSH Terms
Figure
Reference
-
1. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018; 68:723–750. PMID: 29624699.
Article2. European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018; 69:182–236. PMID: 29628281.3. Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017; 11:317–370. PMID: 28620797.
Article4. Korean Liver Cancer Study Group and Korean National Cancer Center. 2014 Korean Liver Cancer Study Group-National Cancer Center Korea practice guideline for the management of hepatocellular carcinoma. Korean J Radiol. 2015; 16:465–522. PMID: 25995680.5. Kudo M, Trevisani F, Abou-Alfa GK, Rimassa L. Hepatocellular carcinoma: therapeutic guidelines and medical treatment. Liver Cancer. 2016; 6:16–26. PMID: 27995084.
Article6. Kim YY, An C, Kim DY, Aljoqiman KS, Choi JY, Kim MJ. Failure of hepatocellular carcinoma surveillance: inadequate echogenic window and macronodular parenchyma as potential culprits. Ultrasonography. 2019; 38:311–320. PMID: 31079440.
Article7. Rhee H, Kim MJ, Park YN, An C. A proposal of imaging classification of intrahepatic mass-forming cholangiocarcinoma into ductal and parenchymal types: clinicopathologic significance. Eur Radiol. 2019; 29:3111–3121. PMID: 30560357.
Article8. Kim YY, Park MS, Aljoqiman KS, Choi JY, Kim MJ. Gadoxetic acid-enhanced magnetic resonance imaging: hepatocellular carcinoma and mimickers. Clin Mol Hepatol. 2019; 25:223–233. PMID: 30661336.
Article9. Han S, Choi JI, Park MY, Choi MH, Rha SE, Lee YJ. The diagnostic performance of liver MRI without intravenous contrast for detecting hepatocellular carcinoma: a case-controlled feasibility study. Korean J Radiol. 2018; 19:568–577. PMID: 29962863.
Article10. Murakami T, Tsurusaki M. Hypervascular benign and malignant liver tumors that require differentiation from hepatocellular carcinoma: key points of imaging diagnosis. Liver Cancer. 2014; 3:85–96. PMID: 24944999.
Article11. Chernyak V, Fowler KJ, Kamaya A, Kielar AZ, Elsayes KM, Bashir MR, et al. Liver imaging reporting and data system (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology. 2018; 289:816–830. PMID: 30251931.
Article12. Cerny M, Bergeron C, Billiard JS, Murphy-Lavallée J, Olivié D, Bérubé J, et al. LI-RADS for MR imaging diagnosis of hepatocellular carcinoma: performance of major and ancillary features. Radiology. 2018; 288:118–128. PMID: 29634435.
Article13. Elsayes KM, Kielar AZ, Elmohr MM, Chernyak V, Masch WR, Furlan A, et al. White paper of the Society of Abdominal Radiology hepatocellular carcinoma diagnosis disease-focused panel on LI-RADS v2018 for CT and MRI. Abdom Radiol (NY). 2018; 43:2625–2642. PMID: 30155697.
Article14. Cerny M, Chernyak V, Olivié D, Billiard JS, Murphy-Lavallée J, Kielar AZ, et al. LI-RADS version 2018 ancillary features at MRI. Radiographics. 2018; 38:1973–2001. PMID: 30289735.
Article15. Zech CJ, Ba-Ssalamah A, Berg T, Chandarana H, Chau GY, Grazioli L, et al. Consensus report from the 8th International Forum for Liver Magnetic Resonance Imaging. Eur Radiol. 2019; 8. 05. [Epub ahead of print]. DOI: 10.1007/s00330-019-06369-4.
Article16. Li J, Wang J, Lei L, Yuan G, He S. The diagnostic performance of gadoxetic acid disodium-enhanced magnetic resonance imaging and contrast-enhanced multi-detector computed tomography in detecting hepatocellular carcinoma: a meta-analysis of eight prospective studies. Eur Radiol. 2019; 6. 27. [Epub ahead of print]. DOI: 10.1007/s00330-019-06294-6.
Article17. Korean Society of Abdominal Radiology. Diagnosis of hepatocellular carcinoma with gadoxetic acid-enhanced MRI: 2016 consensus recommendations of the Korean Society of Abdominal Radiology. Korean J Radiol. 2017; 18:427–443. PMID: 28458595.18. Imai Y, Katayama K, Hori M, Yakushijin T, Fujimoto K, Itoh T, et al. Prospective comparison of Gd-EOB-DTPA-enhanced MRI with dynamic CT for detecting recurrence of HCC after radiofrequency ablation. Liver Cancer. 2017; 6:349–359. PMID: 29234638.
Article19. Roberts LR, Sirlin CB, Zaiem F, Almasri J, Prokop LJ, Heimbach JK, et al. Imaging for the diagnosis of hepatocellular carcinoma: a systematic review and meta-analysis. Hepatology. 2018; 67:401–421. PMID: 28859233.
Article20. Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014; 48:193–204. PMID: 24582925.
Article21. Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008; 27:157–172. discussion 207-212. PMID: 17569110.
Article22. Liu X, Jiang H, Chen J, Zhou Y, Huang Z, Song B. Gadoxetic acid disodium-enhanced magnetic resonance imaging outperformed multidetector computed tomography in diagnosing small hepatocellular carcinoma: a meta-analysis. Liver Transpl. 2017; 23:1505–1518. PMID: 28886231.
Article23. Choi SH, Lee SS, Kim SY, Park SH, Park SH, Kim KM, et al. Intrahepatic cholangiocarcinoma in patients with cirrhosis: differentiation from hepatocellular carcinoma by using gadoxetic acid-enhanced MR imaging and dynamic CT. Radiology. 2017; 282:771–781. PMID: 27797675.
Article24. Chen N, Motosugi U, Morisaka H, Ichikawa S, Sano K, Ichikawa T, et al. Added value of a gadoxetic acid-enhanced hepatocyte-phase image to the LI-RADS system for diagnosing hepatocellular carcinoma. Magn Reson Med Sci. 2016; 15:49–59. PMID: 26104079.
Article25. Joo I, Lee JM, Lee DH, Ahn SJ, Lee ES, Han JK. Liver imaging reporting and data system v2014 categorization of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: comparison with multiphasic multidetector computed tomography. J Magn Reson Imaging. 2017; 45:731–740. PMID: 27474328.
Article26. Kim YN, Song JS, Moon WS, Hwang HP, Kim YK. Intra-individual comparison of hepatocellular carcinoma imaging features on contrast-enhanced computed tomography, gadopentetate dimeglumine-enhanced MRI, and gadoxetic acid-enhanced MRI. Acta Radiol. 2018; 59:639–648. PMID: 28825310.
Article27. Fraum TJ, Tsai R, Rohe E, Ludwig DR, Salter A, Nalbantoglu I, et al. Differentiation of hepatocellular carcinoma from other hepatic malignancies in patients at risk: diagnostic performance of the liver imaging reporting and data system version 2014. Radiology. 2018; 286:158–172. PMID: 28853673.28. Kim MJ, Lee S, An C. Problematic lesions in cirrhotic liver mimicking hepatocellular carcinoma. Eur Radiol. 2019; 29:5101–5110. PMID: 30788586.
Article29. Kim YY, Kim MJ, Kim EH, Roh YH, An C. Hepatocellular carcinoma versus other hepatic malignancy in cirrhosis: performance of LI-RADS version 2018. Radiology. 2019; 291:72–80. PMID: 30694166.
Article30. Lee HS, Kim MJ, An C. How to utilize LR-M features of the LI-RADS to improve the diagnosis of combined hepatocellular-cholangiocarcinoma on gadoxetate-enhanced MRI? Eur Radiol. 2019; 29:2408–2416. PMID: 30552477.
Article31. Ludwig DR, Fraum TJ, Cannella R, Ballard DH, Tsai R, Naeem M, et al. Hepatocellular carcinoma (HCC) versus non-HCC: accuracy and reliability of liver imaging reporting and data system v2018. Abdom Radiol (NY). 2019; 44:2116–2132. PMID: 30798397.
Article32. Ronot M, Fouque O, Esvan M, Lebigot J, Aubé C, Vilgrain V. Comparison of the accuracy of AASLD and LI-RADS criteria for the non-invasive diagnosis of HCC smaller than 3 cm. J Hepatol. 2018; 68:715–723. PMID: 29274407.33. Becker AS, Barth BK, Marquez PH, Donati OF, Ulbrich EJ, Karlo C, et al. Increased interreader agreement in diagnosis of hepatocellular carcinoma using an adapted LI-RADS algorithm. Eur J Radiol. 2017; 86:33–40. PMID: 28027763.
Article34. Barth BK, Donati OF, Fischer MA, Ulbrich EJ, Karlo CA, Becker A, et al. Reliability, validity, and reader acceptance of LI-RADS— An in-depth analysis. Acad Radiol. 2016; 23:1145–1153. PMID: 27174029.35. Fowler KJ, Tang A, Santillan C, Bhargavan-Chatfield M, Heiken J, Jha RC, et al. Interreader reliability of LI-RADS version 2014 algorithm and imaging features for diagnosis of hepatocellular carcinoma: a large international multireader study. Radiology. 2018; 286:173–185. PMID: 29091751.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comprehensive Review of Hepatocellular Carcinoma Enhancement Patterns in MRI: Emphasis on Gadoxetate-Enhanced Imaging
- Hemangioma Diagnosed by Gadoxetate Disodium-Enhanced MRI in a Patient with Chronic Hepatitis C
- Fusion imaging of real-time ultrasonography with CT or MRI for hepatic intervention
- Hepatic Arterioportal Shunts: Dynamic CT and MR Features
- Hepatic Angiomyolipoma Presenting as a Hyperintense Lesion During the Hepatobiliary Phase of Gadoxetic Acid Enhanced-MRI: a Case Report