Korean J Gastroenterol.
2020 Jan;75(1):50-55. 10.4166/kjg.2020.75.1.50.
Palliative Measures with Ethanol Gallbladder Ablation and Endobiliary Radiofrequency Ablation Followed by Endoscopic Biliary Stent Placement in an Advanced Case of Common Bile Duct Cancer: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea. minky1973@hanmail.net
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Radiology, School of Medicine, Kyungpook National University, Daegu, Korea.
- KMID: 2471140
- DOI: http://doi.org/10.4166/kjg.2020.75.1.50
Abstract
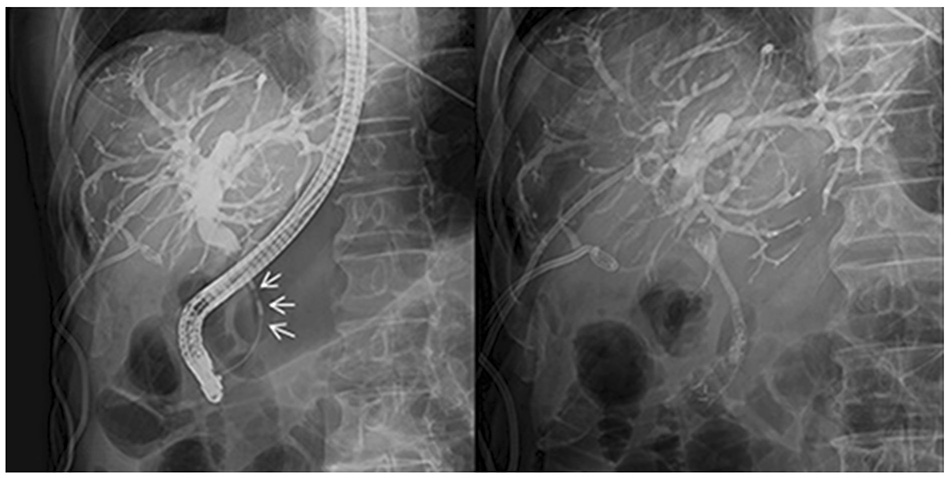
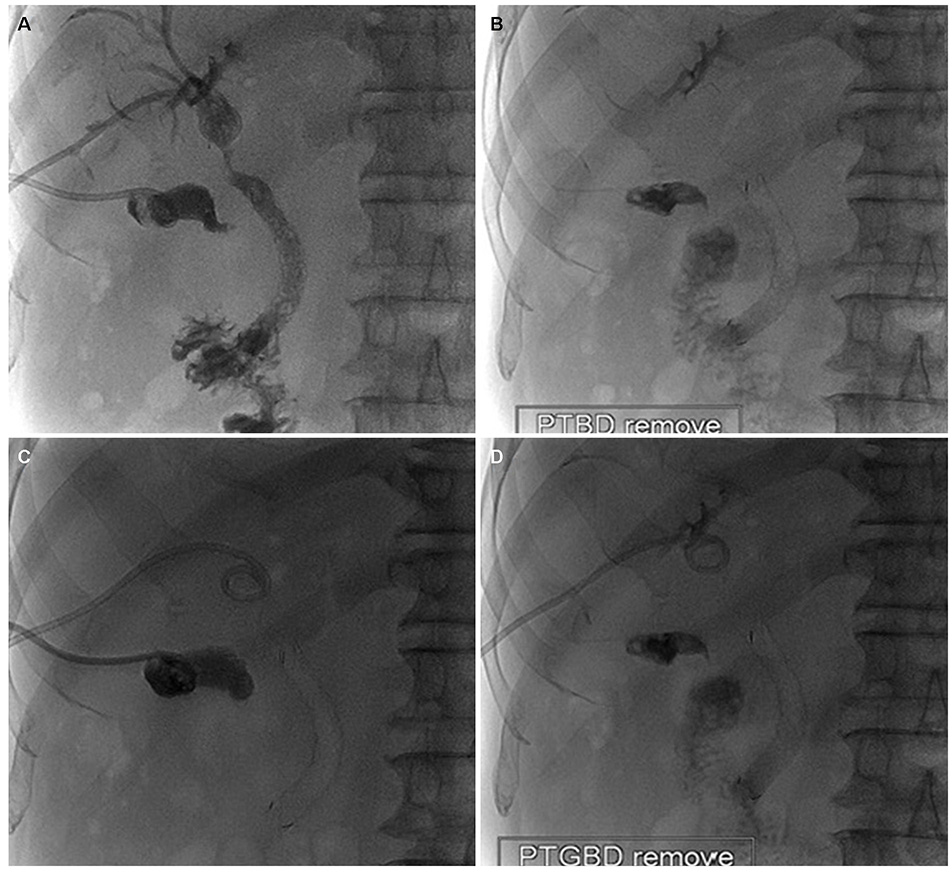
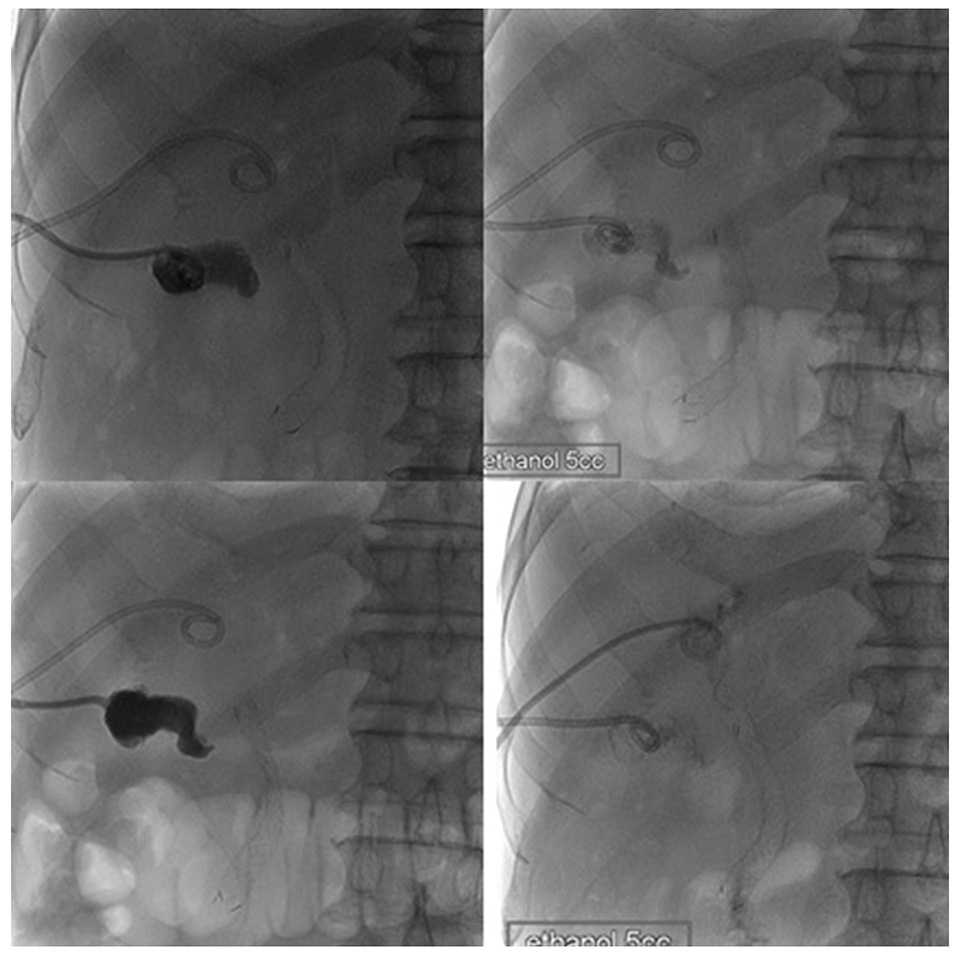
- Endobiliary radiofrequency ablation (RFA) is a procedure performed widely to induce locoregional tumor control by the transfer of thermal energy to the lesion and subsequent tumor necrosis. A 72-year-old male with a prior history of acute calculous cholangitis and perforated cholecystitis was admitted to the Kyungpook National University Hospital complaining of fever and nausea. He had an indwelling percutaneous transhepatic gallbladder drainage (PTGBD) catheter from the previous episode of perforated cholecystitis. An abdominal CT scan showed marked dilation of both the intrahepatic and extrahepatic bile ducts. Common bile duct cancer was confirmed histologically after an endobiliary biopsy. A surgical resection was considered to be the initial treatment option. During open surgery, multiple metastatic nodules were present in the small bowel mesentery and anterior abdominal wall. Resection of the tumor was not feasible, so endobiliary RFA was performed prior to biliary stenting. Cholecystectomy was required for the removal of the PTGBD catheter, but the surgical procedure could not be performed due to a cystic ductal invasion of the tumor. Instead, chemical ablation of the gallbladder (GB) with pure ethanol was performed to breakdown the GB mucosa. Palliative treatment for a biliary obstruction was achieved successfully using these procedures. In addition, a PTGBD catheter was removed successfully without significant side effects. As a result, an improvement in the patient's quality of life was accomplished.
Keyword
MeSH Terms
-
Abdominal Wall
Aged
Bile Ducts, Extrahepatic
Biopsy
Catheter Ablation*
Catheters
Cholangiocarcinoma
Cholangiopancreatography, Endoscopic Retrograde
Cholangitis
Cholecystectomy
Cholecystitis
Common Bile Duct*
Cystic Duct
Drainage
Ethanol*
Fever
Gallbladder*
Gyeongsangbuk-do
Humans
Male
Mesentery
Mucous Membrane
Nausea
Necrosis
Palliative Care
Quality of Life
Stents*
Tomography, X-Ray Computed
Ethanol
Figure
Reference
-
1. Cho JH, Lee KH, Kim JM, Kim YS, Lee DH, Jeong S. Safety and effectiveness of endobiliary radiofrequency ablation according to the different power and target temperature in a swine model. J Gastroenterol Hepatol. 2017; 32:521–526.
Article2. Majeed AW, Reed MW, Stephenson TJ, Johnson AG. Chemical ablation of the gallbladder. Br J Surg. 1997; 84:638–641.
Article3. Dawwas MF, Oppong KW, Webster GJ. Endoscopic assessment and management of biliary strictures. Frontline Gastroenterol. 2016; 7:170–175.
Article4. Yang J, Wang J, Zhou H, et al. Efficacy and safety of endoscopic radiofrequency ablation for unresectable extrahepatic cholangiocarcinoma: a randomized trial. Endoscopy. 2018; 50:751–760.
Article5. Sharaiha RZ, Sethi A, Weaver KR, et al. Impact of radiofrequency ablation on malignant biliary strictures: results of a collaborative registry. Dig Dis Sci. 2015; 60:2164–2169.
Article6. Sofi AA, Khan MA, Das A, et al. Radiofrequency ablation combined with biliary stent placement versus stent placement alone for malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc. 2018; 87:944–951.e1.7. Isayama H, Kawabe T, Nakai Y, et al. Cholecystitis after metallic stent placement in patients with malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2006; 4:1148–1153.
Article8. Suk KT, Kim HS, Kim JW, et al. Risk factors for cholecystitis after metal stent placement in malignant biliary obstruction. Gastrointest Endosc. 2006; 64:522–529.
Article9. Lee TH, Park SH, Kim SP, et al. Chemical ablation of the gallbladder using alcohol in cholecystitis after palliative biliary stenting. World J Gastroenterol. 2009; 15:2041–2043.
Article10. Xu Z, Wang L, Zhang N, Ling X, Hou C, Zhou X. Chemical ablation of the gallbladder: clinical application and long-term observations. Surg Endosc. 2005; 19:693–696.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Endobiliary Radiofrequency Ablation for Malignant Biliary Obstruction
- Role of radiofrequency ablation in advanced malignant hilar biliary obstruction
- Comparing palliative treatment options for cholangiocarcinoma: photodynamic therapy vs. radiofrequency ablation
- Safety and Efficacy of Percutaneous Intraductal Radiofrequency Ablation Followed by Dual Stent Placement for Malignant Biliary Hilar Obstruction
- Intraductal Radiofrequency Ablation as a Palliative Treatment for Advanced Malignant Hilar Biliary Obstruction