J Korean Soc Radiol.
2017 Nov;77(5):298-308. 10.3348/jksr.2017.77.5.298.
Safety and Efficacy of Percutaneous Intraductal Radiofrequency Ablation Followed by Dual Stent Placement for Malignant Biliary Hilar Obstruction
- Affiliations
-
- 1Department of Radiology, Pusanl National University Hospital, Busan, Korea. radkim@nate.com
- 2Department of Radiology, School of Medicine, Pusan National University, Yangsan, Korea.
- KMID: 2394043
- DOI: http://doi.org/10.3348/jksr.2017.77.5.298
Abstract
- PURPOSE
To evaluate the safety and clinical efficacy of percutaneous intraductal radiofrequency ablation (RFA) followed by dual stent placement in advanced malignant biliary hilar duct obstruction.
MATERIALS AND METHODS
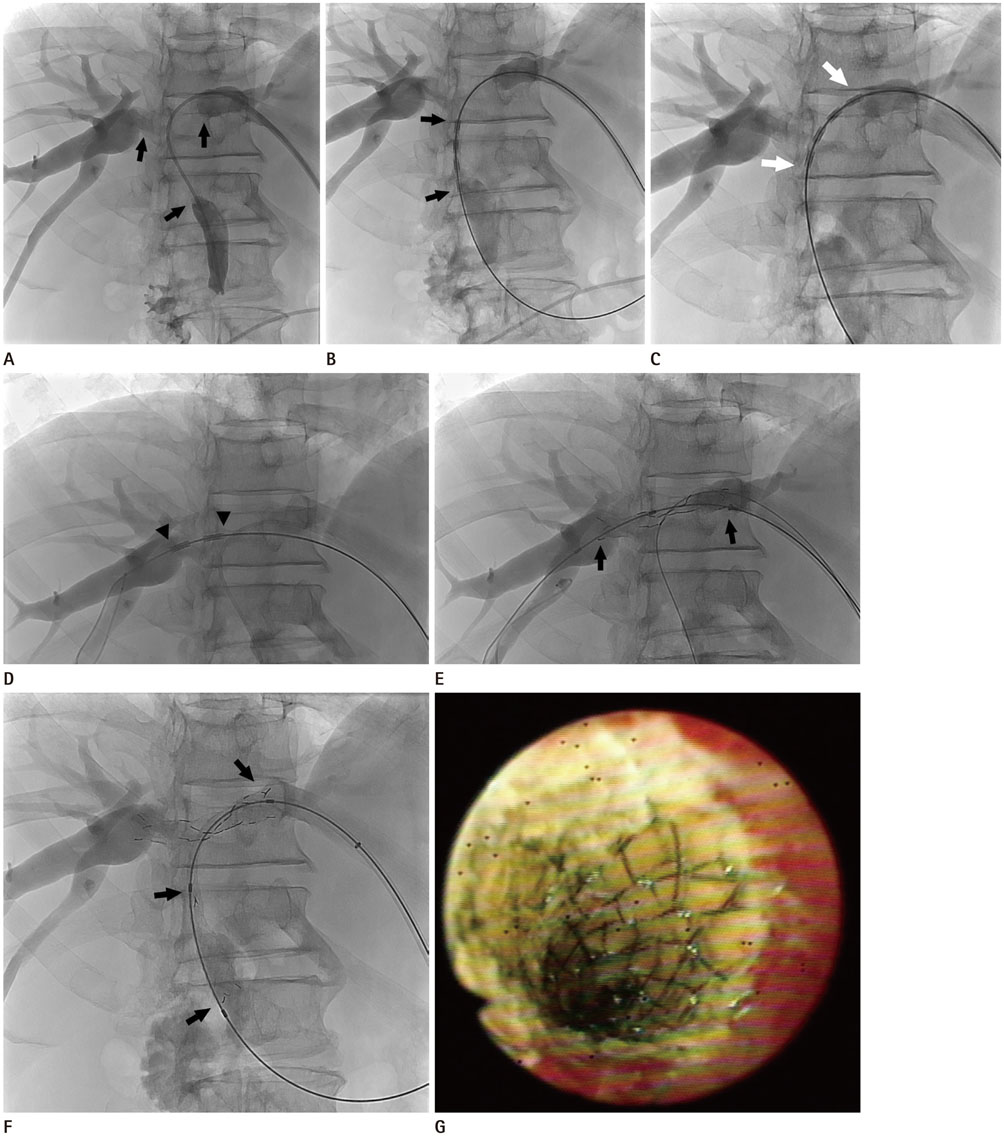
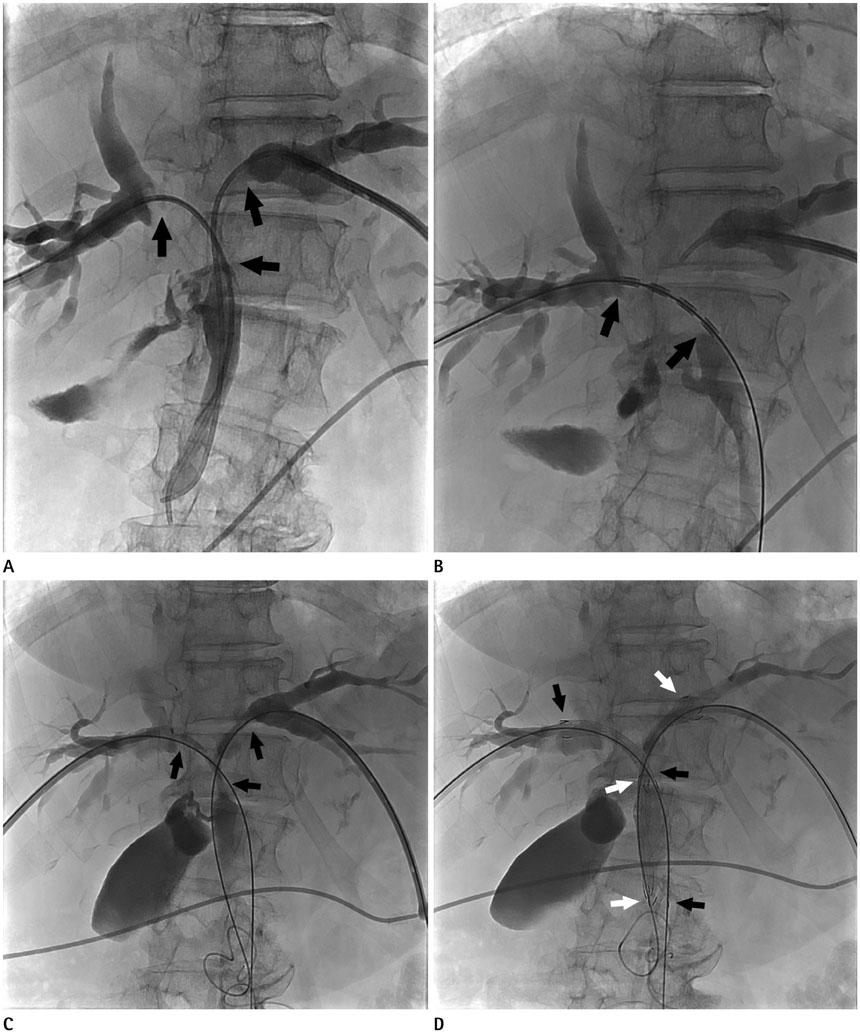
Between September 2013 and August 2015, ten patients with malignant biliary hilar duct obstruction who underwent percutaneous intraductal RFA followed by dual stent placement were included in this retrospective study. Technical success, clinical success, procedure-related complications, stent patency, and patient's survival durations after treatment were investigated.
RESULTS
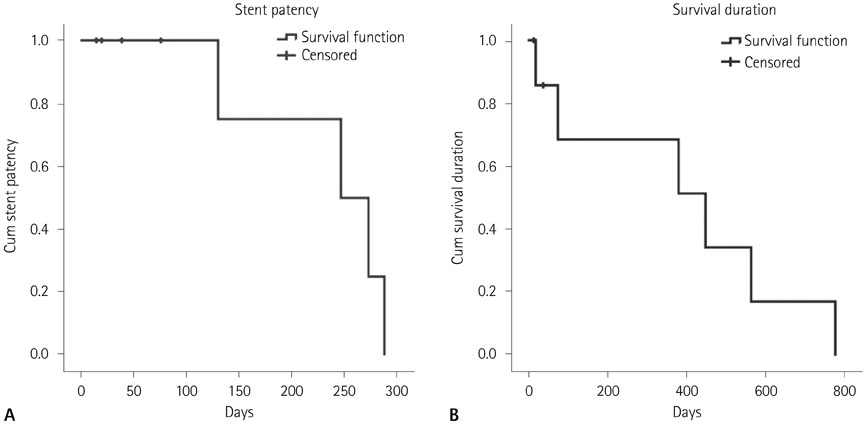
Percutaneous intraductal RFA followed by dual stent placement was successful in all patients; the technical success rate was 100%. No major complications were identified. After the procedure, serum total bilirubin levels were notably normalized, and therefore, percutaneous transhepatic biliary drainage (PTBD) catheter was successfully removed in 8 patients; the clinical success rate was 80%. Four patients with stent dysfunction associated with tumor ingrowth/overgrowth underwent a repeat PTBD procedure or secondary stent insertion. Mean stent patency and survival durations were 233.8 ± 35.6 days [95% confidence interval (CI), 164.0-303.5 days] and 387.2 ± 114.6 days (95% CI, 162.6-611.8 days), respectively.
CONCLUSION
Percutaneous intraductal RFA combined with dual stent placement in advanced malignant biliary hilar duct obstruction is a safe and feasible palliative treatment option.
MeSH Terms
Figure
Reference
-
1. Alexander F, Rossi RL, O'Bryan M, Khettry U, Braasch JW, Watkins E Jr. Biliary carcinoma. A review of 109 cases. Am J Surg. 1984; 147:503–550.2. Wade TP, Prasad CN, Virgo KS, Johnson FE. Experience with distal bile duct cancers in U.S. Veterans Affairs hospitals: 1987-1991. J Surg Oncol. 1997; 64:242–245.3. Loew BJ, Howell DA, Sanders MK, Desilets DJ, Kortan PP, May GR, et al. Comparative performance of uncoated, self-expanding metal biliary stents of different designs in 2 diameters: final results of an international multicenter, randomized, controlled trial. Gastrointest Endosc. 2009; 70:445–453.4. Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992; 340:1488–1492.5. Kaassis M, Boyer J, Dumas R, Ponchon T, Coumaros D, Delcenserie R, et al. Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. Gastrointest Endosc. 2003; 57:178–118.6. Schmassmann A, von Gunten E, Knuchel J, Scheurer U, Fehr HF, Halter F. Wallstents versus plastic stents in malignant biliary obstruction: effects of stent patency of the first and second stent on patient compliance and survival. Am J Gastroenterol. 1996; 91:654–659.7. Mizandari M, Pai M, Xi F, Valek V, Tomas A, Quaretti P, et al. Percutaneous intraductal radiofrequency ablation is a safe treatment for malignant biliary obstruction: feasibility and early results. Cardiovasc Intervent Radiol. 2013; 36:814–819.8. Li TF, Huang GH, Li Z, Hao CF, Ren JZ, Duan XH, et al. Percutaneous transhepatic cholangiography and intraductal radiofrequency ablation combined with biliary stent placement for malignant biliary obstruction. J Vasc Interv Radiol. 2015; 26:715–721.9. Cho JH, Lee KH, Kim JM, Kim YS, Lee DH, Jeong S. Safety and effectiveness of endobiliary radiofrequency ablation according to the different power and target temperature in a swine model. J Gastroenterol Hepatol. 2017; 32:521–526.10. Wang Y, Cui W, Fan W, Zhang Y, Yao W, Huang K, et al. Percutaneous intraductal radiofrequency ablation in the management of unresectable Bismuth types III and IV hilar cholangiocarcinoma. Oncotarget. 2016; 7:53911–53920.11. Kim CW, Park AW, Won JW, Kim S, Lee JW, Lee SH. T-configured dual stent placement in malignant biliary hilar duct obstructions with a newly designed stent. J Vasc Interv Radiol. 2004; 15:713–717.12. Gwon DI, Ko GY, Yoon HK, Kim YJ, Kim TH, Lee WH, et al. Safety and efficacy of percutaneous Y-configured covered stent placement for malignant hilar biliary obstruction: a prospective, pilot study. J Vasc Interv Radiol. 2012; 23:528–534.13. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S199–S202.14. Shepherd HA, Royle G, Ross AP, Diba A, Arthur M, Colin-Jones D. Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Br J Surg. 1988; 75:1166–1168.15. Dahlstrand U, Sandblom G, Eriksson LG, Nyman R, Rasmussen IC. Primary patency of percutaneously inserted self-expanding metallic stents in patients with malignant biliary obstruction. HPB (Oxford). 2009; 11:358–336.16. Lee SJ, Kim MD, Lee MS, Kim IJ, Park SI, Won JY, et al. Comparison of the efficacy of covered versus uncovered metallic stents in treating inoperable malignant common bile duct obstruction: a randomized trial. J Vasc Interv Radiol. 2014; 25:1912–1920.17. Yoon WJ, Lee JK, Lee KH, Lee WJ, Ryu JK, Kim YT, et al. A comparison of covered and uncovered Wallstents for the management of distal malignant biliary obstruction. Gastrointest Endosc. 2006; 63:996–1000.18. Bezzi M, Zolovkins A, Cantisani V, Salvatori FM, Rossi M, Fanelli F, et al. New ePTFE/FEP-covered stent in the palliative treatment of malignant biliary obstruction. J Vasc Interv Radiol. 2002; 13:581–589.19. Coté GA, Kumar N, Ansstas M, Edmundowicz SA, Jonnalagadda S, Mullady DK, et al. Risk of post-ERCP pancreatitis with placement of self-expandable metallic stents. Gastrointest Endosc. 2010; 72:748–754.20. Khorsandi SE, Zacharoulis D, Vavra P, Navarra G, Kysela P, Habib N. The modern use of radiofrequency energy in surgery, endoscopy and interventional radiology. Eur Surg. 2008; 40:204–210.21. Steel AW, Postgate AJ, Khorsandi S, Nicholls J, Jiao L, Vlavianos P, et al. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc. 2011; 73:149–153.22. Dolak W, Schreiber F, Schwaighofer H, Gschwantler M, Plieschnegger W, Ziachehabi A, et al. Endoscopic radiofrequency ablation for malignant biliary obstruction: a nationwide retrospective study of 84 consecutive applications. Surg Endosc. 2014; 28:854–860.23. Monga A, Gupta R, Ramchandani M, Rao GV, Santosh D, Reddy DN. Endoscopic radiofrequency ablation of cholangiocarcinoma: new palliative treatment modality (with videos). Gastrointest Endosc. 2011; 74:935–937.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraductal Radiofrequency Ablation as a Palliative Treatment for Advanced Malignant Hilar Biliary Obstruction
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Role of radiofrequency ablation in advanced malignant hilar biliary obstruction
- Multiple metallic stents placement for malignant hilar biliary obstruction: Perspective of a radiologist
- Interventional radiologic approach to hilar malignant biliary obstruction