J Neurocrit Care.
2019 Dec;12(2):92-97. 10.18700/jnc.190108.
Sex disparity in acute ischemic stroke outcomes in Korea
- Affiliations
-
- 1Department of Neurology, Dong-A University Hospital, Busan, Republic of Korea. nrcjk65@gmail.comed
- 2Stroke Center, Dong-A University Hospital, Busan, Republic of Korea.
- 3Department of Intensive Care Medicine, Dong-A University Hospital, Busan, Republic of Korea.
- KMID: 2470470
- DOI: http://doi.org/10.18700/jnc.190108
Abstract
- BACKGROUND
It is unclear whether women diagnosed with acute ischemic stroke (AIS) have worse outcome after adjusting for several confounding factors such as age, initial stroke severity, and risk factors. In this study, we investigated sex disparities in long-term functional outcome after AIS.
METHODS
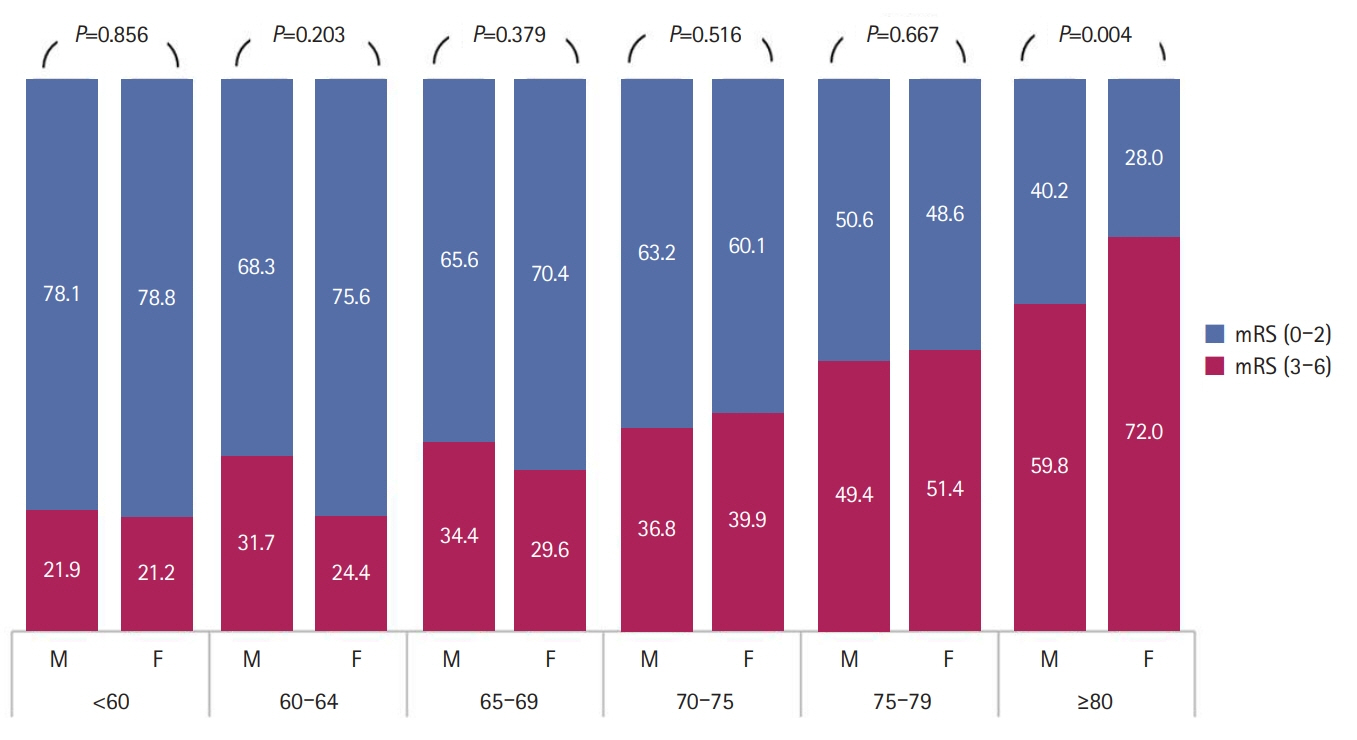
We recruited patients with AIS prospectively registered in the Clinical Research Collaboration for Stroke in Korea database of Dong-A University Stroke Center between 2015 and 2018. We reviewed the patients' clinical demographics, living type (alone or cohabitating), laboratory and radiological findings, stroke severity, stroke subtype, and cardiovascular risk profile. We compared the long-term functional outcomes between men and women using the modified Rankin Scale score at 90 days and 1 year after AIS.
RESULTS
A total of 2,711 patients with AIS were enrolled in this study. Women comprised 38.9% (1,055) of all participants. Compared with men, women were significantly older (72.7±11.6 vs.65.6±12.2, P<0.01), showed more severe neurologic deficits (median National Institutes of Health Stroke Scale, 5 vs. 4, P<0.01), and had a higher rate of living alone (57.1% vs. 42.9%, P<0.01) and a higher prevalence of poor functional outcome at 90 days and 1 year after AIS. However, differences in history of statin use, hospital arrival time, and thrombolysis between the two sexes were not observed. After adjusting for several confounding factors, differences in initial neurologic deficits or long-term functional outcomes between sexes were not observed.
CONCLUSION
This study demonstrated the absence of sex disparities in the status of medical attention for thrombolysis.
Keyword
MeSH Terms
Figure
Reference
-
1. National Center for Health Statistics. Health, United States, 2004 with chartbook on trends in the health of Americans. Hyattsville: US Government Printing Office;2004.2. Adamson J, Beswick A, Ebrahim S. Is stroke the most common cause of disability? J Stroke Cerebrovasc Dis. 2004; 13:171–7.
Article3. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean Stroke Society and clinical research center for stroke. J Stroke. 2013; 15:2–20.
Article4. Kim JS, Lee KB, Roh H, Ahn MY, Hwang HW. Gender differences in the functional recovery after acute stroke. J Clin Neurol. 2010; 6:183–8.
Article5. Maeda K, Toyoda K, Minematsu K, Kobayashi S; Japan Standard Stroke Registry Study Group. Effects of sex difference on clinical features of acute ischemic stroke in Japan. J Stroke Cerebrovasc Dis. 2013; 22:1070–5.
Article6. Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Basile AM, Wolfe CD, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003; 34:1114–9.7. Gall SL, Donnan G, Dewey HM, Macdonell R, Sturm J, Gilligan A, et al. Sex differences in presentation, severity, and management of stroke in a population-based study. Neurology. 2010; 74:975–81.
Article8. Holroyd-Leduc JM, Kapral MK, Austin PC, Tu JV. Sex differences and similarities in the management and outcome of stroke patients. Stroke. 2000; 31:1833–7.
Article9. Roquer J, Campello AR, Gomis M. Sex differences in first-ever acute stroke. Stroke. 2003; 34:1581–5.
Article10. Messé SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology. 2016; 87:1565–74.11. Reid JM, Dai D, Gubitz GJ, Kapral MK, Christian C, Phillips SJ. Gender differences in stroke examined in a 10-year cohort of patients admitted to a Canadian teaching hospital. Stroke. 2008; 39:1090–5.
Article12. Foerch C, Misselwitz B, Humpich M, Steinmetz H, Neumann-Haefelin T, Sitzer M, et al. Sex disparity in the access of elderly patients to acute stroke care. Stroke. 2007; 38:2123–6.
Article13. Kapral MK, Fang J, Hill MD, Silver F, Richards J, Jaigobin C, et al. Sex differences in stroke care and outcomes: results from the Registry of the Canadian Stroke Network. Stroke. 2005; 36:809–14.14. Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D'Agostino RB, Wolf PA. The influence of gender and age on disability following ischemic stroke: the Framingham study. J Stroke Cerebrovasc Dis. 2003; 12:119–26.
Article15. Lai SM, Duncan PW, Dew P, Keighley J. Sex differences in stroke recovery. Prev Chronic Dis. 2005; 2:A13.16. Lee KJ, Kim BJ, Kim DE, Ryu WS, Han MK, Kim JT, et al. Nationwide estimation of eligibility for endovascular thrombectomy based on the DAWN trial. J Stroke. 2018; 20:277–9.
Article17. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article18. Simpson CR, Wilson C, Hannaford PC, Williams D. Evidence for age and sex differences in the secondary prevention of stroke in Scottish primary care. Stroke. 2005; 36:1771–5.
Article19. Glader EL, Stegmayr B, Norrving B, Terént A, Hulter-Asberg K, Wester PO, et al. Sex differences in management and outcome after stroke: a Swedish national perspective. Stroke. 2003; 34:1970–5.20. Reeves MJ, Prager M, Fang J, Stamplecoski M, Kapral MK. Impact of living alone on the care and outcomes of patients with acute stroke. Stroke. 2014; 45:3083–5.
Article21. Redfors P, Isaksén D, Lappas G, Blomstrand C, Rosengren A, Jood K, et al. Living alone predicts mortality in patients with ischemic stroke before 70 years of age: a long-term prospective follow-up study. BMC Neurol. 2016; 16:80.
Article22. Kristofferzon ML, Löfmark R, Carlsson M. Myocardial infarction: gender differences in coping and social support. J Adv Nurs. 2003; 44:360–74.
Article23. Hanna KL, Collins PF. Relationship between living alone and food and nutrient intake. Nutr Rev. 2015; 73:594–611.
Article24. McCullough LD, Hurn PD. Estrogen and ischemic neuroprotection: an integrated view. Trends Endocrinol Metab. 2003; 14:228–35.
Article25. Bushnell CD, Hurn P, Colton C, Miller VM, del Zoppo G, Elkind MS, et al. Advancing the study of stroke in women: summary and recommendations for future research from an NINDS-Sponsored Multidisciplinary Working Group. Stroke. 2006; 37:2387–99.26. Son HC. The Confucian understanding of women. Cathol Philos. 2005; 7:109–47.27. Statics Korea. Press releases: employment and labour [Internet]. Daejeon (KR): Statics Korea;c1996-2019. [cited 2019 Dec 16]. Available from: http://kostat.go.kr/portal/eng/pressReleases/5/1/index.board.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Collateral Circulation in Ischemic Stroke: An Updated Review
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Blood Pressure in Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom