Clin Nutr Res.
2020 Jan;9(1):11-19. 10.7762/cnr.2020.9.1.11.
Effects of Quercetin Supplementation on Hematological Parameters in Non-Alcoholic Fatty Liver Disease: a Randomized, Double-Blind, Placebo-Controlled Pilot Study
- Affiliations
-
- 1Research Center for Environmental Determinants of Health, Health Institute, Kermanshah University of Medical Sciences, Kermanshah 6719851351, Iran.
- 2MSC in Hematology and Blood Bank, Medical Biology Research Center, Kermanshah University of Medical Sciences, Kermanshah 6719851351, Iran.
- 3Eva Hellström Lindberg Group, H7 Department of Medicine, Huddinge, Karolinska Institute, Stockholm 17177, Sweden.
- 4Department of Nutrition Sciences, Texas Tech University, Lubbock, TX 79409, USA.
- 5Department of Nutrition, School of Health, Yasuj University of Medical Sciences, Yasuj 7591875114, Iran.
- 6Department of Nutritional Science, School of Nutritional Science and Food Technology, Kermanshah University of Medical Sciences, Kermanshah 6719851351, Iran. m.hosseinikia@yahoo.com
- KMID: 2468660
- DOI: http://doi.org/10.7762/cnr.2020.9.1.11
Abstract
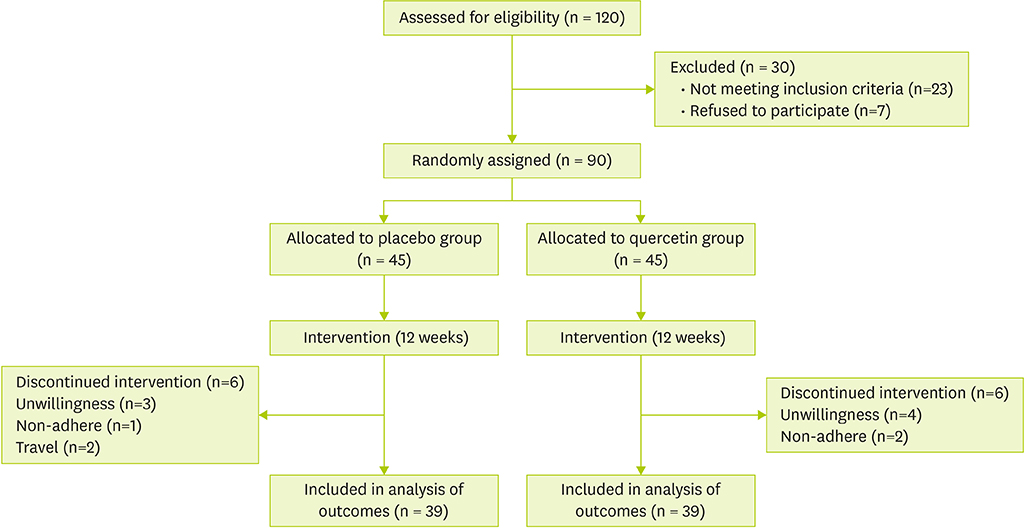
- Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease which has become a public health concern. Since oxidative stress plays a crucial role in the pathogenesis of NAFLD, subsequent hematological disorders are expected. Therefore, antioxidant compounds such as quercetin could ameliorate the related side-effect of oxidative stress. The aim of the current study was to assess the effect of quercetin on hematological parameters in NAFLD patients. A randomized, double-blind, placebo-controlled trial was conducted as a pilot study. In this study 90 patients with NAFLD were supplemented with either a quercetin or a placebo capsule twice daily (500 mg) for 12 weeks. Blood sample was obtained for laboratory parameters at baseline and the end of week 12. End of trial values for red blood cell (RBC; p = 0.002), mean corpuscular hemoglobin concentration (p = 0.029), and mean platelet volume (p = 0.017), significantly increased and the levels of mean corpuscular volume (MCV; p = 0.023), RBC distribution width-coefficient of variation (p = 0.005), platelet distribution width (p = 0.015), and ferritin (p = 0.002) significantly decreased compared to the baseline in group receiving quercetin. Between group analysis revealed that RBC significantly increased (p = 0.025) but, mean corpuscular volume (p = 0.004), mean corpuscular hemoglobin (MCH; p = 0.002), and ferritin (p = 0.013) significantly decreased compared to placebo group. In this work quercetin showed significant effect on RBC, ferritin, MCV, and MCH in intervention group. TRIAL REGISTRATION: Iranian Center for Clinical Trials Identifier: IRCT2016060628299N1
Keyword
MeSH Terms
Figure
Reference
-
1. Takahashi Y, Fukusato T. Histopathology of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014; 20:15539–15548.
Article2. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012; 55:2005–2023.
Article3. Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016; 65:1038–1048.
Article4. Leoni S, Tovoli F, Napoli L, Serio I, Ferri S, Bolondi L. Current guidelines for the management of non-alcoholic fatty liver disease: a systematic review with comparative analysis. World J Gastroenterol. 2018; 24:3361–3373.
Article5. Moghaddasifar I, Lankarani KB, Moosazadeh M, Afshari M, Ghaemi A, Aliramezany M, Afsar Gharebagh R, Malary M. Prevalence of non-alcoholic fatty liver disease and its related factors in Iran. Int J Organ Transplant Med. 2016; 7:149–160.6. Shrestha UK. Non-alcoholic fatty liver disease (NAFLD) is it an emerging risk factor for coronary artery disease? J Adv Intern Med. 2012; 1:1–2.
Article7. Ajmal MR, Yaccha M, Malik MA, Rabbani MU, Ahmad I, Isalm N, Abdali N. Prevalence of nonalcoholic fatty liver disease (NAFLD) in patients of cardiovascular diseases and its association with hs-CRP and TNF-α. Indian Heart J. 2014; 66:574–579.
Article8. Terao J. Factors modulating bioavailability of quercetin-related flavonoids and the consequences of their vascular function. Biochem Pharmacol. 2017; 139:15–23.
Article9. Lesjak M, Beara I, Simin N, Pintać D, Majkić T, Bekvalac K, Orčić D, Mimica-Dukić N. Antioxidant and anti-inflammatory activities of quercetin and its derivatives. J Funct Foods. 2018; 40:68–75.
Article10. Petersen B, Egert S, Bosy-Westphal A, Müller MJ, Wolffram S, Hubbermann EM, Rimbach G, Schwarz K. Bioavailability of quercetin in humans and the influence of food matrix comparing quercetin capsules and different apple sources. Food Res Int. 2016; 88:159–165.
Article11. Sumida Y, Niki E, Naito Y, Yoshikawa T. Involvement of free radicals and oxidative stress in NAFLD/NASH. Free Radic Res. 2013; 47:869–880.
Article12. Arias CF, Arias CF. How do red blood cells know when to die? R Soc Open Sci. 2017; 4:160850.
Article13. Diederich L, Suvorava T, Sansone R, Keller TC 4th, Barbarino F, Sutton TR, Kramer CM, Lückstädt W, Isakson BE, Gohlke H, Feelisch M, Kelm M, Cortese-Krott MM. On the effects of reactive oxygen species and nitric oxide on red blood cell deformability. Front Physiol. 2018; 9:332.
Article14. Mohanty JG, Nagababu E, Rifkind JM. Red blood cell oxidative stress impairs oxygen delivery and induces red blood cell aging. Front Physiol. 2014; 5:84.
Article15. Yang W, Huang H, Wang Y, Yu X, Yang Z. High red blood cell distribution width is closely associated with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2014; 26:174–178.
Article16. Stein J, Connor S, Virgin G, Ong DE, Pereyra L. Anemia and iron deficiency in gastrointestinal and liver conditions. World J Gastroenterol. 2016; 22:7908–7925.
Article17. Kasmi S, Bkhairia I, Harrabi B, Mnif H, Marrakchi R, Ghozzi H, Kallel C, Nasri M, Zeghal K, Jamoussi K, Hakim A. Modulatory effects of quercetin on liver histopathological, biochemical, hematological, oxidative stress and DNA alterations in rats exposed to graded doses of score 250. Toxicol Mech Methods. 2018; 28:12–22.
Article18. Mikstacka R, Rimando AM, Ignatowicz E. Antioxidant effect of trans-resveratrol, pterostilbene, quercetin and their combinations in human erythrocytes in vitro. Plant Foods Hum Nutr. 2010; 65:57–63.
Article19. Al-Omair MA, Sedky A, Ali A, Elsawy H. Ameliorative potentials of quercetin against lead-induced hematological and testicular alterations in Albino rats. Chin J Physiol. 2017; 60:54–61.
Article20. Keskin E, Dönmez N, Kılıçarslan G, Kandır S. Beneficial effect of quercetin on some haematological parameters in streptozotocin-induced diabetic rats. Bull Environ Pharmacol Life Sci. 2016; 5:65–68.21. Mahmoud AM. Hematological alterations in diabetic rats - Role of adipocytokines and effect of citrus flavonoids. EXCLI J. 2013; 12:647–657.22. Koren E, Kohen R, Ginsburg I. Polyphenols enhance total oxidant-scavenging capacities of human blood by binding to red blood cells. Exp Biol Med (Maywood). 2010; 235:689–699.
Article23. Xiao L, Luo G, Tang Y, Yao P. Quercetin and iron metabolism: what we know and what we need to know. Food Chem Toxicol. 2018; 114:190–203.
Article24. Lesjak M, Balesaria S, Skinner V, Debnam ES, Srai SK. Quercetin inhibits intestinal non-haem iron absorption by regulating iron metabolism genes in the tissues. Eur J Nutr. 2019; 58:743–753.
Article25. Mazhar M, Faizi S, Gul A, Kabir N, Simjee SU. Effects of naturally occurring flavonoids on ferroportin expression in the spleen in iron deficiency anemia in vivo. RSC Adv. 2017; 7:23238–23245.
Article26. Lesjak M, Hoque R, Balesaria S, Skinner V, Debnam ES, Srai SK, Sharp PA. Quercetin inhibits intestinal iron absorption and ferroportin transporter expression in vivo and in vitro. PLoS One. 2014; 9:e102900.
Article27. Hoffman R, Benz EJ Jr, Silberstein LE, Heslop H, Anastasi J, Weitz J. Hematology: basic principles and practice. 6th ed. Philadelphia (PA): Elsevier Health Sciences;2013.28. Petruška P, Kalafová A, Kolesárová A, Zbynovská K, Latacz A, Capcarová M. Effect of quercetin on haematological parameters of rabbits: agender comparison. J Microbiol Biotechnol Food Sci. 2013; 2:1540–1549.29. Selvakumar K, Bavithra S, Suganya S, Ahmad Bhat F, Krishnamoorthy G, Arunakaran J. Effect of quercetin on haematobiochemical and histological changes in the liver of polychlorined biphenyls-induced adult male Wistar rats. J Biomark. 2013; 2013:960125.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Onion peel extract reduces the percentage of body fat in overweight and obese subjects: a 12-week, randomized, double-blind, placebo-controlled study
- Effects of daily quercetin-rich supplementation on cardiometabolic risks in male smokers
- Combination of synbiotic and sitagliptin in nonalcoholic fatty liver disease: Is it better than sitagliptin alone?
- Antioxidant Supplementation for Erectile Dysfunction: Systematic Review and Meta-Analysis of Double-Blind, Randomized, Placebo-Controlled Trials
- Antioxidative Activity of Onion Peel Extract in Obese Women: A Randomized, Double-blind, Placebo Controlled Study