Korean J healthc assoc Infect Control Prev.
2019 Dec;24(2):81-87. 10.14192/kjicp.2019.24.2.81.
Colonization Prevalence and Risk Factor Analysis of Carbapenem-Resistant Acinetobacter baumannii in an Intensive Care Unit without Outbreaks
- Affiliations
-
- 1Department of Laboratory Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea. yakim@nhimc.or.kr
- 2Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 3Infection Control Unit, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 4Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2467907
- DOI: http://doi.org/10.14192/kjicp.2019.24.2.81
Abstract
- BACKGROUND
Acinetobacter baumannii is a well-known etiologic agent of a variety of nosocomial infections; the resistance rate to imipenem is surprisingly high in Korea. The colonization of carbapenem-resistant A. baumannii (CRAB) is known to be associated with increased mortality, hospital stay, and cost in intensive care unit (ICU)-admitted patients. In this study, the prevalence, molecular epidemiology, and risk factors of CRAB colonization were evaluated in ICU settings that did not have a current outbreak.
METHODS
Consecutive screening for the colonization of CRAB was performed with 291 patients admitted to the surgical or medical ICU within 48 hours for six months (from April to September 2017) in one general hospital (817 beds, Goyang-si, Gyeonggi-do province, Korea). An active surveillance culture (ASC) for CRAB was performed according to the Centers for Disease Control and Prevention protocols with a perirectal swab sample. After DNA extraction, multiplex PCR was performed to detect carbapenemase genes (bla(OXA-23-like), bla(OXA-24-like), bla(OXA-51-like), bla(OXA-58-like), ISAba1-bla(OXA-23-like), and ISAba1-bla(OXA-51-like gene)). A case-control study was performed to evaluate the risk factors.
RESULTS
Among the 291 patients, the colonization rate of CRAB at ICU admission was 5.2%. The carbapenem resistance mechanism of CRAB colonizers is mostly due to OXA-23-like enzyme production. A risk factor was found to be previous admission to long-term care facilities.
CONCLUSION
To perform ASC for detecting CRAB in ICU-admitted patients, the colonization rate of CRAB should be considered. Patients with a history of admission to a long-term care facility should be prioritized.
MeSH Terms
-
Acinetobacter baumannii*
Acinetobacter*
Case-Control Studies
Centers for Disease Control and Prevention (U.S.)
Colon*
Critical Care*
Cross Infection
Disease Outbreaks*
DNA
Drug Resistance, Bacterial
Gyeonggi-do
Hospital Mortality
Hospitals, General
Humans
Imipenem
Infection Control
Intensive Care Units*
Korea
Long-Term Care
Mass Screening
Molecular Epidemiology
Multiplex Polymerase Chain Reaction
Prevalence*
Risk Factors*
DNA
Imipenem
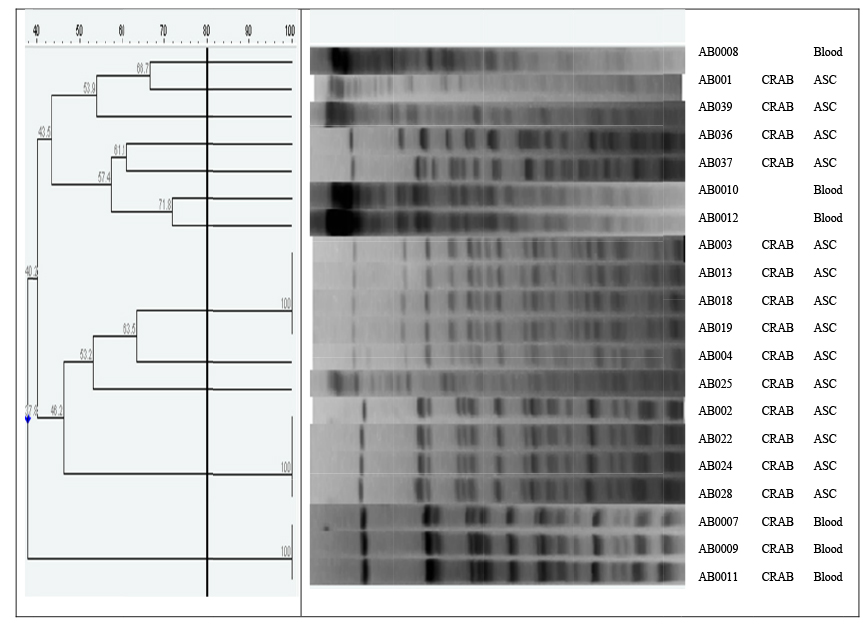
Figure
Reference
-
1. Kim D, Ahn JY, Lee CH, Jang SJ, Lee H, Yong D, et al. Increasing resistance to extended-spectrum cephalosporins, fluoroquinolone, and carbapenem in gram-negative bacilli and the emergence of carbapenem non-susceptibility in klebsiella pneumoniae: analysis of Korean antimicrobial resistance monitoring system (KARMS) data from 2013 to 2015. Ann Lab Med. 2017; 37:231–239.
Article2. Lee Y, Kim YA, Song W, Lee H, Lee HS, Jang SJ, et al. Recent trends in antimicrobial resistance in intensive care units in Korea. Korean J Nosocomial Infect Control. 2014; 19:29–36.
Article3. Kim YA. Epidemiology and treatment of antimicrobialresistant gram-negative bacteria in Korea. Korean J Intern Med. 2018; 33:247–255.
Article4. Qureshi ZA, Hittle LE, O'Hara JA, Rivera JI, Syed A, Shields RK, et al. Colistin-resistant Acinetobacter baumannii: beyond carbapenem resistance. Clin Infect Dis. 2015; 60:1295–1303.
Article5. Kim YA. Active surveillance of multidrug-resistant organisms with rapid detection methods for infection control. Ann Clin Microbiol. 2015; 18:103–110.
Article6. Tsiatsiou O, Iosifidis Ε, Katragkou A, Dimou V, Sarafidis K, Karampatakis T, et al. Successful management of an outbreak due to carbapenem-resistant Acinetobacter baumannii in a neonatal intensive care unit. Eur J Pediatr. 2015; 174:65–74.
Article7. An JH, Kim YH, Moon JE, Jeong JH, Kim SH, Kang SJ, et al. Active surveillance for carbapenem-resistant Acinetobacter baumannii in a medical intensive care unit: can it predict and reduce subsequent infections and the use of colistin? Am J Infect Control. 2017; 45:667–672.
Article8. Lee H. Clinical and economic evaluation of multidrug-resistant Acinetobacter baumannii colonization in the intensive care unit. Infect Chemother. 2016; 48:174–180.
Article9. Richter SS. Screening for carbapenemresistant Enterobacteriaceae: who, when, and how? Virulence. 2017; 8:417–426.
Article10. Jeong S, Hong JS, Kim JO, Kim KH, Lee W, Bae IK, et al. Identification of acinetobacter species using matrixassisted laser desorption ionization-time of flight mass spectrometry. Ann Lab Med. 2016; 36:325–334.
Article11. Héritier C, Poirel L, Fournier PE, Claverie JM, Raoult D, Nordmann P. Characterization of the naturally occurring oxacillinase of Acinetobacter baumannii. Antimicrob Agents Chemother. 2005; 49:4174–4179.
Article12. Clinical and Laboratory Standards Institute. M100 performance standards for antimicrobial susceptibility testing. 27th ed. Wayne: Clinical and Laboratory Standards Institute;2017.13. Woodford N, Ellington MJ, Coelho JM, Turton JF, Ward ME, Brown S, et al. Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int J Antimicrob Agents. 2006; 27:351–353.
Article14. Segal H, Garny S, Elisha BG. Is IS(ABA-1) customized for Acinetobacter? FEMS Microbiol Lett. 2005; 243:425–429.15. Park YS, Bae IK, Kim J, Jeong SH, Hwang SS, Seo YH, et al. Risk factors and molecular epidemiology of community-onset extended-spectrum β-lactamase-producing Escherichia coli bacteremia. Yonsei Med J. 2014; 55:467–475.
Article16. Durante-Mangoni E. Global spread of drugresistant Acinetobacter baumannii: molecular epidemiology and management of antimicrobial resistance. Future Microbiol. 2011; 6:407–422.
Article17. Lee BY, McGlone SM, Doi Y, Bailey RR, Harrison LH. Economic impact of Acinetobacter baumannii infection in the intensive care unit. Infect Control Hosp Epidemiol. 2010; 31:1087–1089.
Article18. World Health Organization. Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. Geneva: World Health Organization;2017.19. Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, et al. SHEA. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol. 2003; 24:362–386.
Article20. Korean Centers for Disease Control and Prevention. Multidrug-resistant Acinetobacter baumannii (MRAB). Infectious Disease Portal;Updated on 5 Jul 2016. http://www.cdc.go.kr/CDC/cms/content/mobile/57/68857_view.html.21. Doi Y, Onuoha EO, Adams-Haduch JM, Pakstis DL, Mc-Gaha TL, Werner CA, et al. Screening for Acinetobacter baumannii colonization by use of sponges. J Clin Microbiol. 2011; 49:154–158.
Article22. Yang HY, Lee HJ, Suh JT, Lee KM. Outbreaks of imipenem resistant Acinetobacter baumannii producing OXA-23 beta-lactamase in a tertiary care hospital in Korea. Yonsei Med J. 2009; 50:764–770.
Article23. Vourli S, Dafopoulou K, Vrioni G, Tsakris A, Pournaras S. Evaluation of two automated systems for colistin susceptibility testing of carbapenem-resistant Acinetobacter baumannii clinical isolates. J Antimicrob Chemother. 2017; 72:2528–2530.
Article24. Henig O, Weber G, Hoshen MB, Paul M, German L, Neuberger A, et al. Risk factors for and impact of carbapenem-resistant Acinetobacter baumannii colonization and infection: matched case-control study. Eur J Clin Microbiol Infect Dis. 2015; 34:2063–2068.
Article25. Sheng WH, Liao CH, Lauderdale TL, Ko WC, Chen YS, Liu JW, et al. A multicenter study of risk factors and outcome of hospitalized patients with infections due to carbapenem-resistant Acinetobacter baumannii. Int J Infect Dis. 2010; 14:e764–e769.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nosocomial Infection by Sequence Type 357 Multidrug-Resistant Acinetobacter baumannii Isolates in a Neonatal Intensive Care Unit in Daejeon, Korea
- Risk Factors of Invasive Carbapenem-Resistant Acinetobacter baumannii Infection in Neonatal Intensive Care Unit during Outbreak
- Multidrug-resistant Acinetobacter baumannii infection in the intensive care unit
- Update on the Epidemiology, Treatment, and Outcomes of Carbapenem-resistant Acinetobacter infections
- Clinical Characteristics of Intensive Care Unit Patients with Carbapenem Resistant Acinetobacter Baumannii Isolated from Sputum