Chonnam Med J.
2014 Aug;50(2):37-44. 10.4068/cmj.2014.50.2.37.
Update on the Epidemiology, Treatment, and Outcomes of Carbapenem-resistant Acinetobacter infections
- Affiliations
-
- 1Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea. haroc153@naver.com
- KMID: 2172157
- DOI: http://doi.org/10.4068/cmj.2014.50.2.37
Abstract
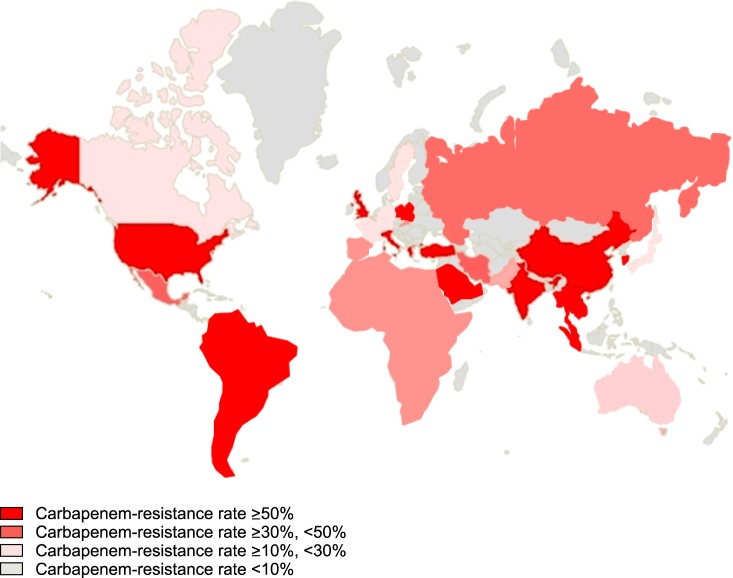
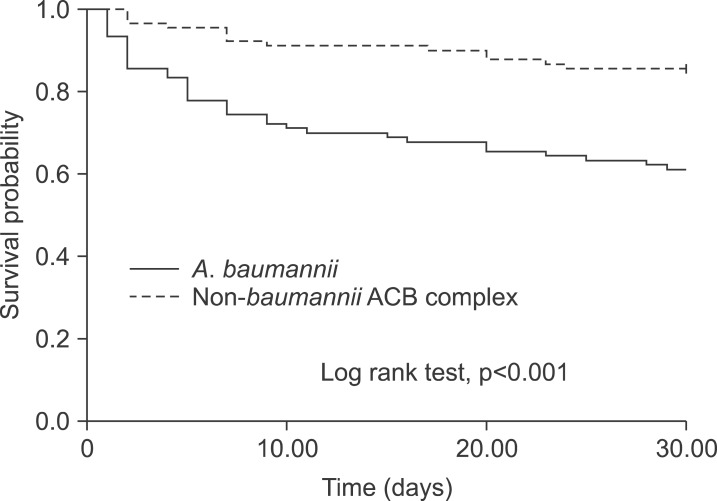
- Carbapenem-resistant Acinetobacter species are increasingly recognized as major nosocomial pathogens, especially in patients with critical illnesses or in intensive care. The ability of these organisms to accumulate diverse mechanisms of resistance limits the available therapeutic agents, makes the infection difficult to treat, and is associated with a greater risk of death. In this review, we provide an update on the epidemiology, resistance mechanisms, infection control measures, treatment, and outcomes of carbapenem-resistant Acinetobacter infections.
Keyword
MeSH Terms
Figure
Reference
-
1. Fournier PE, Richet H. The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin Infect Dis. 2006; 42:692–699. PMID: 16447117.2. Euzéby JP. List of bacterial names with standing in nomenclature: a folder available on the internet. Int J Syst Bacteriol. 1997; 47:590–592. PMID: 9103655.3. Tomaras AP, Dorsey CW, Edelmann RE, Actis LA. Attachment to and biofilm formation on abiotic surfaces by Acinetobacter baumannii: involvement of a novel chaperone-usher pili assembly system. Microbiology. 2003; 149:3473–3484. PMID: 14663080.4. Choi CH, Lee EY, Lee YC, Park TI, Kim HJ, Hyun SH, et al. Outer membrane protein 38 of Acinetobacter baumannii localizes to the mitochondria and induces apoptosis of epithelial cells. Cell Microbiol. 2005; 7:1127–1138. PMID: 16008580.5. Dorsey CW, Beglin MS, Actis LA. Detection and analysis of iron uptake components expressed by Acinetobacter baumannii clinical isolates. J Clin Microbiol. 2003; 41:4188–4193. PMID: 12958246.6. Jankowski S, Grzybek-Hryncewicz K, Fleischer M, Walczuk M. Susceptibility of isolates of Acinetobacter anitratus and Acinetobacter lwoffii to the bactericidal activity of normal human serum. FEMS Microbiol Immunol. 1992; 4:255–260. PMID: 1515154.7. Haseley SR, Pantophlet R, Brade L, Holst O, Brade H. Structural and serological characterisation of the O-antigenic polysaccharide of the lipopolysaccharide from Acinetobacter junii strain 65. Eur J Biochem. 1997; 245:477–481. PMID: 9151982.8. Smith MG, Gianoulis TA, Pukatzki S, Mekalanos JJ, Ornston LN, Gerstein M, et al. New insights into Acinetobacter baumannii pathogenesis revealed by high-density pyrosequencing and transposon mutagenesis. Genes Dev. 2007; 21:601–614. PMID: 17344419.9. Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM. Microbial biofilms. Annu Rev Microbiol. 1995; 49:711–745. PMID: 8561477.10. Martí S, Rodríguez-Baño J, Catel-Ferreira M, Jouenne T, Vila J, Seifert H, et al. Biofilm formation at the solid-liquid and air-liquid interfaces by Acinetobacter species. BMC Research Notes. 2011; 4:5. PMID: 21223561.11. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18:268–281. PMID: 21793988.12. Chuang YY, Huang YC, Lin CH, Su LH, Wu CT. Epidemiological investigation after hospitalising a case with pandrug-resistant Acinetobacter baumannii infection. J Hosp Infect. 2009; 72:30–35. PMID: 19282051.13. Queenan AM, Bush K. Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev. 2007; 20:440–458. PMID: 17630334.14. Poirel L, Nordmann P. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin Microbiol Infect. 2006; 12:826–836. PMID: 16882287.15. Gordon NC, Wareham DW. Multidrug-resistant Acinetobacter baumannii: mechanisms of virulence and resistance. Int J Antimicrob Agents. 2010; 35:219–226. PMID: 20047818.16. Lee K, Kim MN, Choi TY, Cho SE, Lee S, Whang DH, et al. Wide dissemination of OXA-type carbapenemases in clinical Acinetobacter spp. isolates from South Korea. Int J Antimicrob Agents. 2009; 33:520–524. PMID: 19091520.17. Raetz CR, Whitfield C. Lipopolysaccharide endotoxins. Annu Rev Biochem. 2002; 71:635–700. PMID: 12045108.18. Moffatt JH, Harper M, Harrison P, Hale JD, Vinogradov E, Seemann T, et al. Colistin resistance in Acinetobacter baumannii is mediated by complete loss of lipopolysaccharide production. Antimicrob Agents Chemother. 2010; 54:4971–4977. PMID: 20855724.19. Park YK, Choi JY, Shin D, Ko KS. Correlation between overexpression and amino acid substitution of the PmrAB locus and colistin resistance in Acinetobacter baumannii. Int J Antimicrob Agents. 2011; 37:525–530. PMID: 21497062.20. Cai Y, Chai D, Wang R, Liang B, Bai N. Colistin resistance of Acinetobacter baumannii: clinical reports, mechanisms and antimicrobial strategies. J Antimicrob Chemother. 2012; 67:1607–1615. PMID: 22441575.21. Lee SY, Shin JH, Park KH, Kim JH, Shin MG, Suh SP, et al. Identification, genotypic relation, and clinical features of colistin-resistant isolates of Acinetobacter genomic species 13BJ/14TU from bloodstreams of patients in a university hospital. J Clin Microbiol. 2014; 52:931–939. PMID: 24403305.22. Lee SY, Shin JH, Lee K, Joo MY, Park KH, Shin MG, et al. Comparison of the Vitek 2, MicroScan, and Etest methods with the agar dilution method in assessing colistin susceptibility of bloodstream isolates of Acinetobacter species from a Korean university hospital. J Clin Microbiol. 2013; 51:1924–1926. PMID: 23536402.23. Farrell DJ, Sader HS, Flamm RK, Jones RN. Ceftolozane/tazobactam activity tested against Gram-negative bacterial isolates from hospitalised patients with pneumonia in US and European medical centres (2012). Int J Antimicrob Agents. 2014; 43:533–539. PMID: 24856078.24. Zarrilli R, Pournaras S, Giannouli M, Tsakris A. Global evolution of multidrug-resistant Acinetobacter baumannii clonal lineages. Int J Antimicrob Agents. 2013; 41:11–19. PMID: 23127486.25. Kim DH, Choi JY, Kim HW, Kim SH, Chung DR, Peck KR, et al. Spread of carbapenem-resistant Acinetobacter baumannii global clone 2 in Asia and AbaR-type resistance islands. Antimicrob Agents Chemother. 2013; 57:5239–5246. PMID: 23939892.26. Gaynes R, Edwards JR. National Nosocomial Infections Surveillance System. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis. 2005; 41:848–854. PMID: 16107985.27. Wisplinghoff H, Edmond MB, Pfaller MA, Jones RN, Wenzel RP, Seifert H. Nosocomial bloodstream infections caused by Acinetobacter species in United States hospitals: clinical features, molecular epidemiology, and antimicrobial susceptibility. Clin Infect Dis. 2000; 31:690–697. PMID: 11017817.28. Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004; 39:309–317. PMID: 15306996.29. Hilf M, Yu VL, Sharp J, Zuravleff JJ, Korvick JA, Muder RR. Antibiotic therapy for Pseudomonas aeruginosa bacteremia: outcome correlations in a prospective study of 200 patients. Am J Med. 1989; 87:540–546. PMID: 2816969.30. Valencia R, Arroyo LA, Conde M, Aldana JM, Torres MJ, Fernández-Cuenca F, et al. Nosocomial outbreak of infection with pan-drug-resistant Acinetobacter baumannii in a tertiary care university hospital. Infect Control Hosp Epidemiol. 2009; 30:257–263. PMID: 19199531.31. Falagas ME, Karveli EA, Siempos II, Vardakas KZ. Acinetobacter infections: a growing threat for critically ill patients. Epidemiol Infect. 2008; 136:1009–1019. PMID: 17892629.32. Choi JY, Kim CO, Park YS, Yoon HJ, Shin SY, Kim YK, et al. Comparison of efficacy of cefoperazone/sulbactam and imipenem/cilastatin for treatment of Acinetobacter bacteremia. Yonsei Med J. 2006; 47:63–69. PMID: 16502486.33. Smolyakov R, Borer A, Riesenberg K, Schlaeffer F, Alkan M, Porath A, et al. Nosocomial multi-drug resistant Acinetobacter baumannii bloodstream infection: risk factors and outcome with ampicillin-sulbactam treatment. J Hosp Infect. 2003; 54:32–38. PMID: 12767844.34. Oliveira MS, Prado GV, Costa SF, Grinbaum RS, Levin AS. Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J Antimicrob Chemother. 2008; 61:1369–1375. PMID: 18367459.35. Betrosian AP, Frantzeskaki F, Xanthaki A, Douzinas EE. Efficacy and safety of high-dose ampicillin/sulbactam vs. colistin as monotherapy for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. J Infect. 2008; 56:432–436. PMID: 18501431.36. Yang SC, Chang WJ, Chang YH, Tsai YS, Yang TP, Juan CW, et al. Prevalence of antibiotics resistance and OXA carbapenemases genes in multidrug-resistant Acinetobacter baumannii isolates in central Taiwan. Eur J Clin Microbiol Infect Dis. 2010; 29:601–604. PMID: 20186452.37. Nation RL, Li J. Colistin in the 21st century. Curr Opin Infect Dis. 2009; 22:535–543. PMID: 19797945.38. Dalfino L, Puntillo F, Mosca A, Monno R, Spada ML, Coppolecchia S, et al. High-dose, extended-interval colistin administration in critically ill patients: is this the right dosing strategy? A preliminary study. Clin Infect Dis. 2012; 54:1720–1726. PMID: 22423120.39. Kim BN, Peleg AY, Lodise TP, Lipman J, Li J, Nation R, et al. Management of meningitis due to antibiotic-resistant Acinetobacter species. Lancet Infect Dis. 2009; 9:245–255. PMID: 19324297.40. Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004; 39:1267–1284. PMID: 15494903.41. Durante-Mangoni E, Signoriello G, Andini R, Mattei A, De Cristoforo M, Murino P, et al. Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: a multicenter, randomized clinical trial. Clin Infect Dis. 2013; 57:349–358. PMID: 23616495.42. Sirijatuphat R, Thamlikitkul V. Colistin versus Colistin plus Fosfomycin for Treatment of Carbapenem - Resistant Acinetobacter baumannii Infections: A Preliminary Study. Antimicrob Agents Chemother. 2014; 6. 30. pii: AAC.02435-13. [Epub ahead of print].43. Lopez-Cortes LE, Cisneros JM, Fernandez-Cuenca F, Bou G, Tomas M, Garnacho-Montero J, et al. Monotherapy versus combination therapy for sepsis due to multidrug-resistant Acinetobacter baumannii : analysis of a multicentre prospective cohort. J Antimicrob Chemother. 2014; 6. 25. pii: dku233. [Epub ahead of print].44. Paul M, Carmeli Y, Durante-Mangoni E, Mouton JW, Tacconelli E, Theuretzbacher U, et al. Combination therapy for carbapenem-resistant Gram-negative bacteria. J Antimicrob Chemother. 2014; 5. 28. pii: dku168. [Epub ahead of print].45. Montravers P, Bassetti M, Dupont H, Eckmann C, Heizmann WR, Guirao X, et al. Efficacy of tigecycline for the treatment of complicated skin and soft-tissue infections in real-life clinical practice from five European observational studies. J Antimicrob Chemother. 2013; 68(Suppl 2):ii15–ii24. PMID: 23772042.46. Eckmann C, Montravers P, Bassetti M, Bodmann KF, Heizmann WR, Sánchez García M, et al. Efficacy of tigecycline for the treatment of complicated intra-abdominal infections in real-life clinical practice from five European observational studies. J Antimicrob Chemother. 2013; 68(Suppl 2):ii25–ii35. PMID: 23772043.47. Prasad P, Sun J, Danner RL, Natanson C. Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis. 2012; 54:1699–1709. PMID: 22467668.48. Fishbain J, Peleg AY. Treatment of Acinetobacter infections. Clin Infect Dis. 2010; 51:79–84. PMID: 20504234.49. King AM, Reid-Yu SA, Wang W, King DT, De Pascale G, Strynadka NC, et al. Aspergillomarasmine A overcomes metallo-β-lactamase antibiotic resistance. Nature. 2014; 510:503–506. PMID: 24965651.50. Schleicher X, Higgins PG, Wisplinghoff H, Körber-Irrgang B, Kresken M, Seifert H. Molecular epidemiology of Acinetobacter baumannii and Acinetobacter nosocomialis in Germany over a 5-year period (2005-2009). Clin Microbiol Infect. 2013; 19:737–742. PMID: 23034071.51. Wisplinghoff H, Paulus T, Lugenheim M, Stefanik D, Higgins PG, Edmond MB, et al. Nosocomial bloodstream infections due to Acinetobacter baumannii, Acinetobacter pittii and Acinetobacter nosocomialis in the United States. J Infect. 2012; 64:282–290. PMID: 22209744.52. Lee YC, Huang YT, Tan CK, Kuo YW, Liao CH, Lee PI, et al. Acinetobacter baumannii and Acinetobacter genospecies 13TU and 3 bacteraemia: comparison of clinical features, prognostic factors and outcomes. J Antimicrob Chemother. 2011; 66:1839–1846. PMID: 21653602.53. Park KH, Shin JH, Lee SY, Kim SH, Jang MO, Kang SJ, et al. The clinical characteristics, carbapenem resistance, and outcome of Acinetobacter bacteremia according to genospecies. PLoS One. 2013; 8:e65026. PMID: 23755171.54. Chusri S, Chongsuvivatwong V, Rivera JI, Silpapojakul K, Singkhamanan K, McNeil E, et al. Clinical outcomes of hospital-acquired infection with Acinetobacter nosocomialis and Acinetobacter pittii. Antimicrob Agents Chemother. 2014; 58:4172–4179. PMID: 24820079.55. Carbonne A, Naas T, Blanckaert K, Couzigou C, Cattoen C, Chagnon JL, et al. Investigation of a nosocomial outbreak of extended-spectrum beta-lactamase VEB-1-producing isolates of Acinetobacter baumannii in a hospital setting. J Hosp Infect. 2005; 60:14–18. PMID: 15823651.56. De Jong G, Duse A, Richards G, Marais E. Back to basics--optimizing the use of available resources during an outbreak of multi-drug resistant Acinetobacter spp. J Hosp Infect. 2004; 57:186–187. PMID: 15183255.57. Denton M, Wilcox MH, Parnell P, Green D, Keer V, Hawkey PM, et al. Role of environmental cleaning in controlling an outbreak of Acinetobacter baumannii on a neurosurgical intensive care unit. J Hosp Infect. 2004; 56:106–110. PMID: 15019221.58. Idzenga D, Schouten MA, van Zanten AR. Outbreak of Acinetobacter genomic species 3 in a Dutch intensive care unit. J Hosp Infect. 2006; 63:485–487. PMID: 16815591.59. Kraniotaki E, Manganelli R, Platsouka E, Grossato A, Paniara O, Palù G. Molecular investigation of an outbreak of multidrug-resistant Acinetobacter baumannii, with characterisation of class 1 integrons. Int J Antimicrob Agents. 2006; 28:193–199. PMID: 16904293.60. Longo B, Pantosti A, Luzzi I, Placanica P, Gallo S, Tarasi A, et al. An outbreak of Acinetobacter baumannii in an intensive care unit: epidemiological and molecular findings. J Hosp Infect. 2006; 64:303–305. PMID: 16978736.61. Pimentel JD, Low J, Styles K, Harris OC, Hughes A, Athan E. Control of an outbreak of multi-drug-resistant Acinetobacter baumannii in an intensive care unit and a surgical ward. J Hosp Infect. 2005; 59:249–253. PMID: 15694983.62. Cookson B. The working party guidance on the control of multi-resistant AcinetobacterOutbreaks. [Internet]. [place unknown]: 2006. 8. 29. Cited 2009 April 1. Available from: http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Acinetobacter/Guidelines/.63. Morgan DJ, Liang SY, Smith CL, Johnson JK, Harris AD, Furuno JP, et al. Frequent multidrug-resistant Acinetobacter baumannii contamination of gloves, gowns, and hands of healthcare workers. Infect Control Hosp Epidemiol. 2010; 31:716–721. PMID: 20486855.64. Gayoso CM, Mateos J, Méndez JA, Fernández-Puente P, Rumbo C, Tomás M, et al. Molecular mechanisms involved in the response to desiccation stress and persistence in Acinetobacter baumannii. J Proteome Res. 2014; 13:460–476. PMID: 24299215.65. Podnos YD, Cinat ME, Wilson SE, Cooke J, Gornick W, Thrupp LD. Eradication of multi-drug resistant Acinetobacter from an intensive care unit. Surg Infect (Larchmt). 2001; 2:297–301. PMID: 12593705.66. Wilks M, Wilson A, Warwick S, Price E, Kennedy D, Ely A, et al. Control of an outbreak of multidrug-resistant Acinetobacter baumannii-calcoaceticus colonization and infection in an intensive care unit (ICU) without closing the ICU or placing patients in isolation. Infect Control Hosp Epidemiol. 2006; 27:654–658. PMID: 16807837.67. Urban C, Segal-Maurer S, Rahal JJ. Considerations in control and treatment of nosocomial infections due to multidrug-resistant Acinetobacter baumannii. Clin Infect Dis. 2003; 36:1268–1274. PMID: 12746772.68. Wybo I, Blommaert L, De Beer T, Soetens O, De Regt J, Lacor P, et al. Outbreak of multidrug-resistant Acinetobacter baumannii in a Belgian university hospital after transfer of patients from Greece. J Hosp Infect. 2007; 67:374–380. PMID: 18023922.69. Husni RN, Goldstein LS, Arroliga AC, Hall GS, Fatica C, Stoller JK, et al. Risk factors for an outbreak of multi-drug-resistant Acinetobacter nosocomial pneumonia among intubated patients. Chest. 1999; 115:1378–1382. PMID: 10334156.70. Villegas MV, Hartstein AI. Acinetobacter outbreaks, 1977-2000. Infect Control Hosp Epidemiol. 2003; 24:284–295. PMID: 12725359.71. Apisarnthanarak A, Pinitchai U, Thongphubeth K, Yuekyen C, Warren DK, Fraser VJ. Thammasat University Pandrug-Resistant Acinetobacter baumannii Control Group. A multifaceted intervention to reduce pandrug-resistant Acinetobacter baumannii colonization and infection in 3 intensive care units in a Thai tertiary care center: a 3-year study. Clin Infect Dis. 2008; 47:760–767. PMID: 18684100.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Therapy for Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria
- Antimicrobial Therapy for Infections Caused by Multidrug-Resistant Gram-Negative Bacteria
- Carbapenem-Resistant Acinetobacter baumannii
- Epidemiology and treatment of antimicrobialresistant gram-negative bacteria in Korea
- Optimizing Treatment for Carbapenem-Resistant Acinetobacter baumannii Complex Infections: A Review of Current Evidence